The erythron
- 1. Toxicology of the Erythron Dr R B Cope BVSc BSc(Hon 1) PhD cGLPCP DABT ERT
- 2. Learning Objectives • To understand the key basic functional concepts of the erythron; • To understand the fundamentals of erythrokinetics; • To understand and accurately interpret changes in erythrocyte physical parameters (PCV/hematocrit, MCH, MCHC, MCV); • To understand and accurately interpret changes to erythrocyte morphology; • To understand and accurately recognize common abnormal changes in the erythron.
- 3. Basic Concepts of Erythrocyte Function • The erythron: – Consists of circulating erythrocytes + bone marrow precursors + bone marrow progenitor centers + stem cells; – Key function is oxygen transport mediated by hemoglobin;
- 4. Basic Concepts of Erythrocyte Function: Heme Synthesis Disruption of heme synthesis will result in prophyrias due to the accumulation of heme precursors or catabolites. Porphyrias are most commonly genetic (heritable) disorders of metabolism, however xenobiotic- induced porphyrias (or exacerbation of inherited porphyrias) may also occur (common: e.g. lead inhibits ferrochetalase). Porphyrias may or may not be associated with anemia depending on which part of the heme cycle is disrupted. The most common cause (in humans) of reduced heme synthesis is iron deficiencies.
- 5. Basic Concepts of Erythrocyte Function: Globin Synthesis The switch from fetal to adult Hb varies considerably across species. In normal humans, fetal Hb is present until about 8 months of life. In normal adult humans ~ 97% of Hb is HbA, ~ 3% is HbA2. The types of Hb present in adults varies across species
- 6. Note: Fe is in the Fe2+ in the majority of Hb under normal conditions
- 7. Porphyrias • Supplementary reading: – http://emedicine.medscape.com/article/1389981- overview – Xenobiotic-induced porphyria cutanea tarda is the only one I have personally come across: http://emedicine.medscape.com/article/1103643-overview
- 8. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Fetal Hb has a higher affinity for O2 than normal adult Hb – lower oxygen delivery to the tissues compared with adults
- 9. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves
- 10. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves 2,3-DPG = 2,3-diphosphoglycerate • Remember: • Left shift = less oxygen to the tissues = tissue hypoxia • Right shift = more oxygen to the tissues
- 11. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Common and important toxicological situations affecting the O2Hb dissociation curve include: – Oxidative attack on erythrocytes and methemoglobinemias – Formation of sulfhemaglobin – Carbon monoxide
- 12. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Methemoglobinemia – Common cause of toxicological insult to the erythron – The presence of Fe in the Fe2+ reduction state is critical for normal O2 carrying capacity – Any oxidizing agent has the capacity to produce metHb by oxidizing Hb Fe2+ to Hb Fe3+ (ferrous ferric)
- 13. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Methemoglobinemia – The critical effect of metHb is decreased tissue oxygen supply (i.e. tissue hypoxia) – MetHb cannot bind oxygen – The presence of metHb results in a left shift of the O2Hb dissociation curve, further exacerbating tissue hypoxia
- 14. • Blood and mucous membranes are discolored brown (“muddy”) • Blood color change does not reverse (or reverses slowly) with exposure to oxygen (i.e. bubbling oxygen through tube of blood)
- 17. Hemolysis and other signs of oxidative erythrocyte injury are commonly present (e.g. Heinz bodies, intravascular hemolysis)
- 18. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Methemoglobinemia – Note: Rodents are notoriously resistant to oxidative damage to the erythron and the formation of metHb – Note: Routine rodent studies alone may not detect the propensity for metHb formation and/or oxidative damage to the erythron – Note: Children under 4 years of age are more susceptible to oxidative damage to the erythron – Note: Cats are notoriously susceptible to oxidative damage to the erythron
- 19. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Methemoglobinemia – Note: in some human subpopulations glucose-6- phosphate dehydrogenase deficiency common (typically people of African, Middle Eastern and South Asian descent – protective adaptation to endemic malaria). These subpopulations are highly susceptible to oxidative assault on the erythron
- 21. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Methemoglobinemia – Note: Persons with pyruvate kinase deficiency are highly susceptible to oxidative damage to the erythron (lower energy generation lower capacity to recycle GSH) • Also increases 2,3-bisphosphoglycerate (2,3 BPG) right shift of the O2Hb dissociation curve increased tissue oxygenation individuals with PK deficiency may have a greater capacity for physical activity than others with similarly low hemoglobin levels. – Note: Persons with cytochrome b5 reductase deficiency are highly susceptible to oxidative damage to the erythron (reduced capacity to reverse metHb)
- 22. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Methemoglobinemia – Note: Any organo-amine compound should be suspected of being a cause of oxidative damage to the erythron until proven otherwise – Note: any nitrite or nitrate compound (or compounds that are metabolized to a nitrite or a nitrate) are similarly suspect – Note: chromates are also similarly suspect – Note: Halogenated benzenes are also similarly suspect
- 23. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Sulfhemoglobinemia – Due to the formation of ferric sulfide in Hb – Cannot be reversed metabolically – requires the replacement of affected erythrocytes – Produces a right shift of the O2Hb dissociation curve • Question: does this make tissue oxygenation better or worse?
- 24. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • Sulfhemoglobinemia – Usually drug induced • Drugs associated with sulfhemoglobinemia include acetanilid, phenacetin, nitrates, trinitrotoluene and sulfur compounds (mainly sulphonamides, sulfasalazine) – Occupational exposure to sulfur compounds is another potential cause – > 0.5 g% sulfHb is abnormal
- 27. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • CO-Hb; carbon monoxide poisoning; carboxy-Hb – Can occur due to either inhalation of CO (notably products of incomplete combustion) or xenobiotics that are metabolized to CO (common example is methylene chloride) – Hemoglobin binds to carbon monoxide preferentially compared to oxygen (approx 240:1) – COHb will not release the carbon monoxide, and therefore hemoglobin will not be available to transport oxygen from the lungs to the rest of the body
- 28. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • CO-Hb; carbon monoxide poisoning; carboxy-Hb – COHb has a half-life in the blood of 4 to 6 hours – T½ reduced by exposure to oxygen – COHb increases the risk of infarction (increased incidence of ischemic disease in users of methylene chloride) – Produces a left shift of the O2Hb dissociation curve • Question: does this make tissue oxygenation better or worse?
- 29. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • CO-Hb; carbon monoxide poisoning; carboxy-Hb – Produces a distinctive “cherry red” discoloration of blood, tissues, skin – Skeletal muscle is notably bright red due to the formation of carboxymyoglobin (used commercially to keep meat red and more attractive) – Persons who have died from CO poisoning are described as looking rosy cheeked and healthy (cherry red means dead)
- 30. Conditions Affecting Oxygen Carrying Capacity: Oxygen Hb Dissociation Curves • CO-Hb; carbon monoxide poisoning; carboxy-Hb – Important issues: • Samples must be collected in air-tight tubes • Samples must be analyzed quickly otherwise falsely low levels of COHb may be detected • “Cherry red” discoloration of blood, skin, tissues etc. fades with time – important diagnostically • Bubbling oxygen through a tube of blood will hasten the loss of discoloration – used diagnostically
- 35. Basic Concepts of Erythrocyte Function: Iron Metabolism • Except for external blood loss, there is no normal mechanism for the excretion of iron; • Provided the enterothelium remains intact, iron absorption is highly regulated; • Under normal circumstances, there is little free iron present in plasma (total iron binding capacity is not saturated) • Transferrin is a gamma-globulin
- 36. Basic Concepts of Erythrocyte Function: Iron Metabolism • A wide variety of divalent metals compete with Fe2+ for uptake by DMT-1 (notably Cd2+, Pb2+); • The pH of the small intestine favors the formation of Fe3+ (mostly insoluble) which must be reduced by Dcytb to Fe2+ (soluble) for absorption to occur.
- 37. Basic Concepts of Erythrocyte Function: Iron Metabolism • Hepcidin is the key hormone regulating Fe uptake from the GI; • Increased hepcidin occurs in a wide variety of chronic disease states (carcinogenesis) or inflammatory diseases leading to “anemia of chronic disease.” • Anemia of chronic disease is a common finding in chronic toxicology studies.
- 38. Measures of Iron Status: Serum Iron • Measures the amount of iron bound to transferrin in the serum • Unreliable as a measure of total body iron stores • Can be reported as a % of total iron binding capacity (see later)
- 39. Measures of Iron Status: Serum Iron • Conditions associated with low SI – Iron deficiency – Acute and chronic inflammatory processes/disease (anemia of chronic disease, anemia of inflammatory disease) – Hypoproteinemia (notably advanced liver disease)s – Hypothyroidism – Renal disease
- 40. Measures of Iron Status: Serum Iron • Conditions associated with high SI – Hemolytic anemia (due to release of Fe from destroyed erythrocytes) – Sampling error resulting in hemolysis – Excessive glucocorticoids in some species (e.g. Cushing’s disease) – Iron overload • Acquired – Fe overload (Fe poisoning, excessive transfusions etc.) • Hereditary – Non-regenerative anemias (decreased Fe utilization)
- 41. Measures of Iron Status: Serum Total Iron Binding Capacity • TIBC is an indirect measure of how much Fe the transferring present in serum will bind • Under normal conditions, about ⅓ of transferring binding sites are occupied under normal conditions – serum transferrin is not saturated under normal conditions • The difference between TIBC and SI is the amount of available Fe-binding capacity = unbound iron-binding capacity
- 42. Measures of Iron Status: Serum Total Iron Binding Capacity • TIBC is increased in Fe deficiency in most species • TIBC is reduced (or even saturated [i.e. UIBC = 0]) in: – Fe poisoning – Intravascular hemolysis – Sampling error (hemolysis)
- 43. Measures of Iron Status: Ferritin • Ferritin represent the labile (i.e. rapidly available) storage form of Fe • Small amounts of ferritin are normally present in the circulation as part of normal Fe homeostasis • Serum ferritin is decreased during iron deficiency
- 44. Measures of Iron Status: Ferritin • Serum ferritin is increased during: – Hemolytic anemia – Iron overload – Acute and chronic inflammation – Liver disease – Neoplasia (notably lymphoma) – Malnutrition
- 45. Common Causes of Disruptions of Iron Status in Repeated Dose Toxicology Studies • Iron deficiency and/or reduced iron uptake – More likely to be seen in chronic studies – Early stages may occasionally be seen in sub-chronic studies – In rodent studies, the animals are relatively young at the start of the study and are still rapidly growing (increased iron requirement + reduce capacity to absorb it from the GI + higher Hb turnover associated with switch from HbF to HbA) – Iron deficiencies can also can result when high concentrations of the test article are used in the diet – dietary dilution of essential minerals
- 46. Common Causes of Disruptions of Iron Status in Repeated Dose Toxicology Studies • Iron deficiency and/or reduced iron uptake – Test article either inhibits or is a competitive substrate for enterothelial DMT-1 (typically other divalent metals) or Dcytb – Test article is an inhibitor of or competitor ferroportin – Test article reduced dietary iron bioavailability (binding in gut insoluble) e.g. starches, tanins, phytates, vit. C, etc..
- 47. Common Causes of Disruptions of Iron Status in Repeated Dose Toxicology Studies • Chronic disease states, notably neoplasia (increased hepcidin) • Significant inflammatory diseases (acute or chronic; increased hepcidin) • Hemolysis (error or due to toxicological effects) • Severe liver disease
- 48. Erythrokinetics Essential for RBC production: • Iron • Vitamin B12 (cobalamin) • Folic Acid
- 50. Erythrokinetics • The cell is released from the bone marrow as a reticulocyte – Circulating red blood cells are ~1% reticulocytes – After 1–2 days these ultimately become "erythrocytes" or mature red blood cells Question: what does it mean if you have an increased % of reticulocytes in the peripheral blood? Question: what does it mean if you have an increased % of normoblasts or nucleated RBCs in the peripheral blood?
- 53. Erythrokinetics • The following characteristics can be seen changing in the erythrocytes when they are maturing: – They show a reduction in the cell size; – The cytoplasmic matrix increases in amount; – Staining (Wright’s stain) reaction of the cytoplasm changes from blue to pinkish red (this is because of the decrease in the amount of RNA and DNA); – Initially the nucleus was large in size and contained open chromatin. But with the maturation of RBC's the size of the nucleus decreases and finally disappears with the condensation of the chromatin material. Question: what does it mean if you have an increase in the number of RBCs in the peripheral circulation that stain blue (technical term = polychromasia or polychromatophilia)?
- 55. Erythrokinetics Question: what does it mean if you have an increase in variation of erythrocyte size in peripheral blood (technical term = anisocytosis)?
- 57. Erythrokinetics • Lifespan of an RBC in peripheral blood is species specific – in the range of 70 – 150 days in mammals depending on species; 35 days or so in birds • Eryptosis (RBC programmed cell death) – Form of apoptosis – Process makes the RBC prone to the extravascular pathway of erythrocyte destruction (phagocytosis by the reticuloendothelial systems of the liver, spleen and bone marrow [predominantly the red pulp of the spleen]) – Normally eryptosis and erthyropoesis exist in balance
- 58. Erythrokinetics • Two pathways for RBC destruction: – Extravascular pathway (predominantly in the spleen, but also bone marrow and liver) – Intravascular pathway (i.e. lyse within the circulation)
- 59. The anatomic structure of the spleen is ideal for testing the metabolic machinery and pliability of the red blood cells. Within the splenic pulp, red blood cells are concentrated and their intracellular metabolic pathways stressed. Following this, red blood cells must pass through 2- to 5-µm pores to enter the sinusoidal system. Unusually rigid cells or a cell containing inclusion bodies will be unable to pass this test and will be destroyed by sinusoidal reticuloendothelial cells.
- 60. Bite Cell
- 65. Regulation of Erythropoesis EPO is produced in the juxtaglomerular apparatus of the kidney
- 66. Evaluation of the Erythron: Indicators of the Circulating RBC Mass • Endpoints that are commonly used are: – Hematocrit (= packed cell volume = PCV) – Hemoglobin concentration of peripheral blood – RBC count
- 67. Evaluation of the Erythron: Hematocrit (Packed Cell Volume = PCV)
- 68. Evaluation of the Erythron: Hematocrit (=HCT=Packed Cell Volume = PCV) • HCT measured by centrifugation is a very accurate measure (± 1%) • Most commonly HCT is a calculated value from automated cell counters where HCT% = RBC/ul x mean corpuscular volume (fL) – Calculated HCT has a higher level of error – Cell counter MUST be calibrated to the species being examined – Birds have eliptical nucleated RBCs which interferes with this method
- 69. Evaluation of the Erythron: Hematocrit (=HCT=Packed Cell Volume = PCV) • Typically plasma protein concentration by refractometry is measured at the same time • Typically the plasma color is examined (red for hemolysis, yellow of icterus/jaundice, lipidemia = pink and opaque)
- 71. Evaluation of the Erythron: Hb Concentration • Provides the most direct measurement of the oxygen transport capacity of blood • Value should be ~ ⅓ of the HCT if RBCs are of normal size • Typically a colorimetric measurement • Must be corrected if Heinz bodies, hemolysis, or lipidemia is present • Major advantage over HCT is it allows calculation of the MCH and MCHC
- 72. Evaluation of the Erythron: RBC Count • Automated machine counting is reasonably accurate if appropriately calibrated (except for birds) • Manual hemocytometer counts have a large error and are of little value except in birds • Major value of RBC count is that it allows calculation of the MCV and MCH (see below)
- 73. Evaluation of the Erythron: RBC Count • Low values occur in anemia • High values occur in polycythemia (or blood doping) • Spuriously high values occur with dehydration and excitement in species with a contractile spleen (notably horses)
- 74. Evaluation of the Erythron: Factors Affecting HCT, Hb, RBC • Low values occur in anemia • High values occur in polycythemia (or blood doping) • Spuriously high values occur with dehydration and excitement in species with a contractile spleen (notably horses) • Overhydration will result in spuriously low values • Fluid shifts (e.g. shock) can cause spurious values
- 75. Evaluation of the Erythron: Factors Affecting HCT, Hb, RBC • The hydration/intravascular volume status of the animal must be determined in order to accurately interpret HCT, Hb and RBC! • How do you do this? – Total serum or plasma protein (serum or plasma specific gravity) in combination with the albumen:globulin ratio (A:G) is a useful quick guide – If the TP and plasma albumen are increased (in proportion) and the A:G ratio remains within the normal range, this is an indicator of dehydration (particularly if combined with an increased HCT HB & RBC) Why?
- 76. Evaluation of the Erythron: Factors Affecting HCT, Hb, RBC • If both the TP and A:G are within the normal range and the HCT Hb & RBC are low, what does this suggest? • If the TP and A:G ratio are within the normal range and the HCT Hb & RBC are high, what does this suggest?
- 77. Evaluation of the Erythron: RBC Indices Used in the Classification of Anemia • Mean corpuscular volume (MCV) = average RBC volume in fL • Mean corpuscular hemoglobin (MCH) = average mass of Hb present per RBC in pg • Mean corpuscular hemoglobin concentration (MCHC) = average concentration of Hb in RBC in g/100 mL of RBCs • Red cell distribution width = coefficient of variation of the RBC volume distribution
- 78. Evaluation of the Erythron: Mean Corpuscular Volume (MCV) • Can be a calculated value or determined by an automated cell counter – Calculate by dividing the HCT by the RBC count and converting to fL
- 79. Evaluation of the Erythron: Mean Corpuscular Volume (MCV) • Common causes of increased MCV (macrocytosis) – Reticulocytosis – Why? – Anything that inhibits nucleic acid synthesis and inhibits cell division i.e. reduced number of cell divisions during RBC ontogeny in the bone marrow. Commonly B12 deficiency • B12 deficiency is classically macrocytic and hypochromic (see later) – Anything that delays RBC maturation – Why? – Genetics – must make sure you are using the correct normal control values for the given strain – Spurious – RBC agglutination will result in falsely high MCV values
- 80. Evaluation of the Erythron: Mean Corpuscular Volume (MCV) • Common causes of increased MCV (macrocytosis) – Megaloblastic anemia, the most common cause of macrocytic anemia, is due to a deficiency of either vitamin B12, folic acid, or both – Pernicious anemia is caused by a lack of intrinsic factor, which is required to absorb vitamin B12 from food. A lack of intrinsic factor may arise from an autoimmune condition targeting the parietal cells (atrophic gastritis) that produce intrinsic factor or against intrinsic factor itself. These lead to poor absorption of vitamin B12. Alcoholism is a major cause of B12 malabsorption – Macrocytic anemia can also be caused by damage to the stomach (reduced B12 and folate absorption) – Hypothyroidism – Methotrexate, zidovudine, and other drugs may inhibit DNA replication.
- 81. Evaluation of the Erythron: Mean Corpuscular Volume (MCV) • Common causes of increased MCV (macrocytosis) – Macrocytic anemia can be further divided into "megaloblastic anemia" or "nonmegaloblastic macrocytic anemia". – The cause of megaloblastic anemia is primarily a failure of DNA synthesis with preserved RNA synthesis, which results in restricted cell division of the progenitor cells. The megaloblastic anemias often present with neutrophil hypersegmentation (six to 10 lobes). – The nonmegaloblastic macrocytic anemias have different etiologies (i.e. unimpaired DNA globin synthesis,) which occur, for example, in alcoholism.
- 82. Evaluation of the Erythron: Mean Corpuscular Volume (MCV) • Immature animals of most species have small RBCs and lower normal MCV values – must use the correct normal range for the species, strain and age group! • Causes of reduced MCV (microcytosis) • Iron deficiency is a classical cause of microcytosis – due to an additional round of cell division required to reach the critical cytoplasmic concentration of Hb necessary to stop further DNA synthesis and cell division of RBC precursors. Typically Fe deficiency anemias are microcytic hypochromic anemais
- 83. Evaluation of the Erythron: Mean Corpuscular Volume (MCV) • Causes of reduced MCV (microcytosis) – Heme synthesis defect • Iron deficiency anemia • Anemia of chronic disease (more commonly presenting as normocytic anemia) – Globin synthesis defect • Alpha-, and beta-thalassemia • HbE syndrome • HbC syndrome • Various other unstable hemoglobin diseases
- 84. Evaluation of the Erythron: Mean Corpuscular Volume (MCV) • Normocytic anemias – Normocytic anemia occurs when the overall hemoglobin levels are decreased, but the red blood cell size (mean corpuscular volume) remains normal. – Causes include: • Acute blood loss • Anemia of chronic disease • Aplastic anemia (bone marrow failure) • Hemolytic anemia
- 86. Evaluation of the Erythron: Mean Corpuscular Hb (MCH) • MCH = Hb ÷ RBC count • Generally factors affecting the MCV affect the MCH in a similar way – If the MCV is decreased (e.g. Fe deficiency), the MCH decreases since smaller RBCs contain less Hb • In general, the MCH is much less value than the other parameters in the classification of anemias • Interpretation of the Hb status of RBCs should be based on the MCHC rather than the MCV because the MCHC corrects for cell volume
- 87. Evaluation of the Erythron: Mean Corpuscular Hb Concentration (MCHC) • MCHC = Hb ÷ HCT and then adjusted to g/dL • MCHC is the most accurate of the RBC indices because it does not require a RBC count • MCHC is the most useful parameter in classification of anemias • A true increase in MCHC does not normally occur – Increased MCHC is almost always spurious – due to hemolysis (calculation assumes that all Hb is contained within RBCs which is not true if hemolysis has occurred)
- 88. Evaluation of the Erythron: Mean Corpuscular Hb Concentration (MCHC) • Reduced MCHC (Hypochromasia = hypochromia) – Occurs with reticulocytosis – reticulocytes are larger cells and contain less Hb, accordingly the Hb concentration is decreased – Iron deficiency due to reduced synthesis of Hb – Vitamin B6 deficiency – reduced synthesis of Hb – Lead exposure (inhibition of synthesis of Hb) – Drugs or xenobiotics that disrupt Hb synthesis
- 89. Microcytic hypochromic anemia (Fe deficiency)
- 90. Evaluation of the Erythron: RBC Distribution Width (RDW) • Coeficient of variation of the RBC volume distribution • RDW = SDMCV ÷ MCV x 100 • Index of the variation in size (i.e. aniocytosis) of RBCs • Anemias which are microcytic or macrocytic will have increased anioscytosis and an increased RDW • Significant reticulocytosis will result in an increased RDW and anisocytosis
- 91. Aniosocytosis
- 92. Reticulocytosis
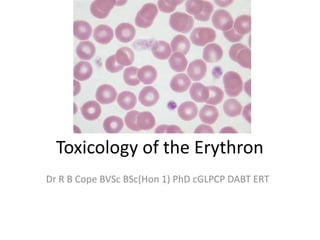
- 93. Peripheral Blood Smear – RBC Morphology • Stains – New methylene blue – acidic structures stain blue or purple (i.e. DNA, RNA, basophil granules) – Romanowsky stains (e.g. Wright’s, Diff-Quick) – acidic structures stain blue to purple, basic groups stain red (protein, eosinophil granules)
- 94. Peripheral Blood Smear – RBC Morphology • Rouleaux formation – RBCs for stacks – Presence indicates an alteration of RBC surface charge (zeta potential) – Interpretation depends on the species • Horses normally have some Rouleaux formation in health – Rouleaux formation correlates with the RBC sedimentation rate i.e. protein coating of the surface of RBCs (e.g. fibrin during inflammatory processes, increased globulins, multiple myeloma) increased ESR + increased Rouleaux formation
- 96. Peripheral Blood Smear – RBC Morphology • Agglutination – Grape-like congregations of RBCs due to the presence of a cross-linking antibody (typically anti RBC IgM) – Important in toxicology because there are numerous xenobiotics that act as haptens on the surface of RBCs and generate an autoimmune anemia
- 98. Peripheral Blood Smear – RBC Morphology • Spherocytes – Associated with immune mediated anemias – an important biomarker of extravascular immune-mediated RBC destruction – Result of phagocytosis of antigens on the surface of RBCs – Can result from phagocytosis of Heinz bodies (areas of oxidative precipitation of Hb in the erythrocyte – biomarker of oxidative damage to Hb) – Rarely, can result of changes to cell membrane compositon (acquired or hereditary)
- 100. Peripheral Blood Smear – RBC Morphology • Polychromatophilia – Cells have a light blue-gray color when stained with a Wright’s stain – Classical feature of increased numbers of immature peripheral RBCs in the peripheral blood i.e. accelerated release of RBCs from the bone marrow – Classical characteristic feature of reticulocytes i.e. reticulocytosis is described as macrocytic, polychromasia and polychromatophilic..
- 102. Peripheral Blood Smear – RBC Morphology • Poikilocytosis – General term for abnormally shaped RBCs – Can be spurious due to storage of sample before analysis – Can be normal in some species and at some stages of development e.g. switching from fetal to adult Hb – Indicate trauma to the RBC cell membrane due to • Turbulent blood flow • Intravascular fibrin (microangiopathic effects) – Specific types of poikilocytes can be associated with particular diseases e.g. acanthocytes are associated with particular types of liver diseases
- 103. Acanthocytosis Typical response to listening to Barry Manilow music…..
- 104. Peripheral Blood Smear – RBC Morphology • Echinocytosis – Form of poikiloctyes – Can be due to artifact – Can be due to xenobiotic exposure, particularly if effected blood electrolytes or membrane electrolyte transport or osmotic effects
- 106. Peripheral Blood Smear – RBC Morphology • Hemlet cells (keratocytes) – Biomarker of oxidative damage to RBCs – Develop due to rupturing of a cell membrane vesicle or membrane blebs – Can also be produced by microangiopathic processes (see schistocytes below)
- 107. Peripheral Blood Smear – RBC Morphology • Schistocyte – Irregular RBC fragments due to cutting of the RBC into pieces by intravascular fibrin deposits
- 109. Peripheral Blood Smear – RBC Morphology • Basophilic stippling – Due to residual clumps of RNA, or precipitated ribosomes or mitochondria in RBCs – A characteristic of lead exposure (rare finding) – typically there is basophilic stippling but NO polychromasia (why?) – Can occur during regenerative anemias in conjunction with polychromasia – Also seen with severe burns, some xenobiotics, septicemia
- 111. Peripheral Blood Smear – RBC Morphology • Heinz bodies – A classical biomarker of oxidative damage to the erythron – Due to denatured Hb – RBCs prone to hemolysis
- 112. Peripheral Blood Smear – RBC Morphology • Metarubricyte – Term refers to the presence of any form of nucleated RBC in the peripheral blood – Indicates highly increased demand for RBCs and may be appropriate (e.g. response to increased erythropoesis in responsive anemias) or inappropriate (e.g. due to lead poisoning, Fe deficiency, Cu deficiency etc.)
- 113. Bone Marrow Evaluation • Parameters: – Cellularity – Number of megakaryocytes (platelet precursors) – Myeloid: erythroid ratio – Morphology
- 115. Bone Marrow Evaluation • M:E ratio – Usually used to determine the efficiency of the response to anemia – Should be interpreted with the WBC count i.e. if the WBC count is normal and the M:E is decreased it is indicative of an increased production of RBCs and a normal response to anemia – A high M:E ratio in the presence of a normal WBC count and anemia indicates a problem with RBC production
- 117. Regenerative Vs Non-Regenerative Anemias • Characteristics of regenerative anemias = evidence of increased production of RBCs – Polychromasia – Why? – Reticulocytosis – Why? – Anisocytosis + increased RDW – Why? – Increased MCV + macrocytosis – Why? – Basophilic stippling – Why? – Hypercellular bone marrow with a reduced M:E – Why? – Are all of the above responses appropriate and if so, why?
- 118. Regenerative Vs Non-Regenerative Anemias • Characteristics of regenerative anemias = evidence of increased production of RBCs – Polychromasia – Why? – Reticulocytosis – Why? – Anisocytosis + increased RDW – Why? – Increased MCV + macrocytosis – Why? – Basophilic stippling – Why? – Hypercellular bone marrow with a reduced M:E – Why? – Are all of the above responses appropriate and if so, why?
- 119. Regenerative Vs Non-Regenerative Anemias • Characteristics of regenerative anemias – Tend to be non-chronic – Internal blood loss and hemolytic anemias tend to respond more rapidly than external blood loss anemias (why?)
- 120. Regenerative Vs Non-Regenerative Anemias • Characteristics of non-regenerative anemias – Tend to chronic – why? – By definition there is an inadequate bone marrow response which may be due to: • Not enough time – RBC destruction is faster than RBC production • Inadequate precursor materials (e.g. Fe, B12, B6 etc.) • Increased hepcidin due to inflammatory diseases (decreased Fe) • Renal disease – not enough erythropoeitin • Bone marrow destruction (neoplasia, infections)
- 121. Case Studya1 • Following data (group mean from treatment group) was from day 45 of a 90 day study in rats: Parameter Value High or low relative to normal Range, Pre- exposure measurements and control Group (all changes statistically significant) HCT 13 % Low Hb 3.9 g/dL Low RBC 1.59 x 106/ul Low MCV 81 fL High MCH 24.5 pg MCHC 30.0 % Low Reticulocytes 16.5 % High 264 x 103/ul Nucleated RBCs 3 per 100 WBC High Total protein 3.8 g/dL Low Albumin 1.8 g/dL Low A:G 0.90 Normal RBC morphology: anisocytosis, polychromasia
- 122. Case Studya1 • Following data (group mean from treatment group) was from day 45 of a 90 day study in rats: Parameter Value High or Low Compared With Normal Range and Control Group Platelets 653 x 103/uL High WBC 17.5 x 103/uL High WBC morphology is normal 1.59 x 106/ul Low
- 123. Case Study 1 • Answer the following questions – What is the type of erythron problem present? – What other problems are present? – What is the likely mechanism involved? – Is the problem being reversed/repaired? – What would you hope to see by day 90 of the study? – What would you expect to see 30 days following the cessation of exposure to the test article? • Why? • What conditions might have to happen for any change to occur? • What conditions might prevent any putative recovery?
- 124. Case Studya2 • Following data (group mean from treatment group) was from day 90 of a rat study Parameter Value High or low relative to normal Range, Pre- exposure measurements and control Group (all changes statistically significant) HCT 15% Low Hb 4.4 g/dL Low RBC 1.79 x 106/ul Low MCV 84 fL High MCH 24.6 pg MCHC 29.3 % Low Reticulocytes 24 % High 430 x 103/ul Nucleated RBCs 6 per 100 WBC High Total protein 6.5 g/dL Normal Albumin 2.9 g/dL Normal A:G 0.81 Normal RBC morphology: anisocytosis, polychromasia, spherocytosis,
- 125. Case Study 2 • Answer the following questions – What is the type of erythron problem present? – What other problems are present? – What is the likely mechanism involved? – Is the problem being reversed/repaired? – What would you hope to see by day 90 of the study? – What would you expect to see 30 days following the cessation of exposure to the test article? • Why? • What conditions might have to happen for any change to occur? • What conditions might prevent any putative recovery?
- 126. Case Study 3 • Following data (group mean from a treatment group) was from day 3 of a 90 day study in cats. Some deaths have occurred in this exposed group Parameter Value High or low relative to normal Range, Pre- exposure measurements and control Group (all changes statistically significant) HCT 25.2% Low Hb 11.2 g/dL Normal RBC 5.5 x 106/ul Low MCV 45 fL Normal MCH 20 pg MCHC 44 % High Total protein 8.5 High Albumin 3.9 g/dL Normal A:G 0.85 Normal RBC morphology: excessive Heinz bodies present Additional comments: serum is red tinged, blood was chocolate colored, urine was dark brown
- 127. Case Study 3 • Answer the following questions – What is the type of erythron problem present? – What other problems are present? – What is the likely mechanism involved? – Is the problem being reversed/repaired? – What other problems might occur with this? – What would you hope to see by day 90 of the study? – What would you expect to see 30 days following the cessation of exposure to the test article? • Why? • What conditions might have to happen for any change to occur? • What conditions might prevent any putative recovery?
- 128. Case Studya4 • Following data (group mean from treatment group) was from day 90 of a 90 day study in rats: Parameter Value High or low relative to normal Range, Pre- exposure measurements and control Group (all changes statistically significant) HCT 12.8 % Low Hb 4.0 g/dL Low RBC 2.25 x 106/ul Low MCV 56.9 fL High MCH 17.8 pg Low MCHC 31.3 % Low Reticulocytes 0% Low Nucleated RBCs 0 per 100 WBC High RBC morphology: hypochromasia
- 129. Case Study 4 • Answer the following questions – What is the type of erythron problem present? – What other problems are present? – What is the likely mechanism involved? – Is the problem being reversed/repaired? – What other problems might occur with this? – What would you hope to see by day 90 of the study? – What would you expect to see 30 days following the cessation of exposure to the test article? • Why? • What conditions might have to happen for any change to occur? • What conditions might prevent any putative recovery?
- 130. Case Studya5 • Following data (group mean from treatment group) was from day 90 of a 90 day study in rats: Parameter Value High or low relative to normal Range, Pre- exposure measurements and control Group (all changes statistically significant) HCT 26 % Low Hb 8.8 g/dL Low RBC 5.23 x 106/ul Low MCV 49.7 fL Normal MCH 16.8 pg MCHC 33.8 % Normal Reticulocytes 0.1 % Normal 52 x 103/ul Nucleated RBCs 0 per 100 WBC High Total protein 9.3 g/dL High Albumin 1.9 g/dL Low A:G 0.0.26 low RBC morphology: Normal
- 131. Case Study 5 • Answer the following questions – What is the type of erythron problem present? – What other problems are present? – What is the likely mechanism involved? – Is the problem being reversed/repaired? – What other problems might occur with this? – What would you hope to see by day 90 of the study? – What would you expect to see 30 days following the cessation of exposure to the test article? • Why? • What conditions might have to happen for any change to occur? • What conditions might prevent any putative recovery?
- 132. Case Study 1 • Regenerative blood loss anemia • Macrocytic hypochromic anemia with polychromasia and reticulocytosis • Loss of total protein due to hemorrhage + subsequent fluid shifts into the vascular compartment
- 133. Case Study 2 • Macrocytic hypochromic regenerative hemolytic anemia with evidence of extravascular erythrophagocytosis • Autoimmune mediated anemia
- 134. Case Study 3 • Oxidative intravascular hemolytic anemia + met Hb
- 135. Case Study 4 • Microcytic, hypochromic non-regenerative anemia • Fe deficiency
- 136. Case Study 5 • Normocytic, normochromic anemia + hyperproteinemia due increased globulins + decreased albumen • Chronic inflammatory disease
Notas do Editor
- ----- Meeting Notes (16/11/12 23:57) -----Case 1: External blood loss anemia
- ----- Meeting Notes (16/11/12 23:57) -----Case 1: External blood loss anemia
