Anestesia para px con aneurisma (colocación de stent)
- 1. Anesthesia for Patients With Aortic Aneurysm Undergoing Endovascular Stenting Benjamin Drenger, MD and Sudheer Jain, MD Department of Anesthesiology and Critical Care Medicine Hebrew University - Hadassah Medical Center Jerusalem, Israel Department of Anesthesiology New York University Langone Medical Center New York, New York aortic surgery, thoracic aortic repair carries an even higher Learning Objectives: risk for postoperative morbidity and mortality. Although As a result of completing this activity, the participant these risks have diminished in recent years with the will be able to significant advances in perioperative care and surgical Evaluate the risks, different approaches to anesthe- techniques, aortic aneurysm surgery is still considered a sia, outcome and anesthesia, motor evoked poten- high-risk procedure. The introduction of less invasive and tials, and anesthetic considerations, for patients potentially safer stent grafts as an alternative to open undergoing endovascular stenting surgical repair has led to new perspectives in the treatment Describe the important role of transesophageal of aneurysms and aortic dissections. echocardiography in diagnosing abnormalities and guiding endovascular stenting procedures Endovascular grafting has the distinct advantage of Discuss mechanisms of cerebrospinal fluid (CSF) being a much less traumatic technique compared with pressure rise, indications and risks of CSF drainage, conventional arterial reconstruction, owing to the unique the risk of cerebral hemorrhage, and blood patch ability of being able to insert these grafts through small incisions in remote arterial access sites. In patients with Author Disclosure Information: multiple comorbidities, avoiding the need for extensive The authors have disclosed that they have no periaortic dissection, prolonged aortic occlusion, sig- financial interests or significant relationship with nificant fluid shifts, and substantial blood loss has special any commercial companies pertaining to this educa- significance in patient outcome. Proper placement of an tional activity. endovascular stent may reduce the incidence of aortic rupture, whereas in cases of dissection, it will seal the in- timal tear, decompress the false lumen, and may even re- ortic aneurysm surgery is a formidable burden for A every patient and carries substantial risks for serious complications. When compared with abdominal place conventional medical therapy for this condition. In recent years, the accumulated experience in endovascular stent surgery has allowed long-term outcome comparisons with open surgery. The common conclusion of these stu- dies is that the significantly lower operative mortality of Supplemental digital content is available for this article. Direct URL stent-graft surgery in the short term (30 days post- citations appear in the printed text and are available in both the HTML operatively) is offset in the long term by higher rates of and PDF versions of this article. Links to the digital files are provided in graft-related complications and costlier reinterventions for the HTML and PDF text of this article on the Journal’s Web site (www.asa-refresher.com). endovascular repair.1,2 41
- 2. 42 Drenger and Jain The current indications for endovascular treatment of echocardiography—transesophageal echocardiography (TEE) thoracic and abdominal aortic lesions are no longer limited for thoracic aortic lesions—is performed to confirm that to patients who are unfit for open surgical repair due to the endovascular stent graft has successfully excluded the older age and severe systemic concomitant diseases (sub- lesion from central aortic flow. stantial cardiac, pulmonary, and renal dysfunction). An In aortic arch pathology and in descending thoracic open surgical repair is still recommended for patients with dissection, special consideration is taken to exclude the thoracoabdominal aneurysms, for whom endovascular initial intimal tear. Excluding the intimal tear with a short stent graft options are limited.3 Most aortic aneurysms and endoluminal stent is usually followed by rapid thrombosis type B aortic dissections can be treated by endovascular of the false lumen; however, because long-term sealing of procedures as long as they meet the technical criteria for the secondary lumen is less certain, longer grafts are safe advancement and deployment of the stent. In younger usually needed. By inhibiting the continued flow of blood patients with minimal or no medical comorbidities, an open into the false lumen, end organ ischemia, infarction, and surgical repair is indicated because of its established track risk of rupture are prevented and future aneurysm forma- record of low complications and because the long-term tion is retarded. In cases of aortic arch pathology, addi- outcome of endovascular stenting remains uncertain.4 tional surgical interventions might be needed to preserve A patient is considered to be a candidate for a stent-graft carotid flow, such as carotid to carotid bypass, carotid to procedure if the major prerequisites are met: (a) The mor- subclavian bypass, or femoroaxillary bypass.5 When the phology of the aneurysm, with special attention to the whole arch is in need of repair, reimplantation of the bra- ‘‘landing zone,’’ will allow the graft to be anchored. A chiocephalic artery and the left carotid artery is performed minimum of 20 mm of normal aortic wall is required for first, followed by arch endograft implantation either im- safe stent deployment, secure anchoring, and avoiding the mediately or two weeks later. These aortic arch endografts obstruction of major branch-artery ostia. (b) Distal vas- are currently not approved by the U.S. Food and Drug cular access of sufficient size is present. Severe stenosis or Administration and their use is limited to centers partici- occlusion of the abdominal aorta or the iliac arteries may pating in studying this evolving technique. prevent the passage of the endograft delivery system. (c) There is limited tortuosity of the aorta. Substantial kinking may result in arterial dissection after insertion of the vas- By inhibiting the continued flow of blood into cular sheath (see Supplemental Digital Content 1, http:// the false lumen, end organ ischemia, infarc- links.lww.com/ASA/A108). Thoracic aneurysms are con- sidered for repair in cases of pain symptoms and when the tion, and risk of rupture are prevented and maximum diameter is more than 5.5 cm (smaller diameter limit in Marfan syndrome). In cases of aortic dissection, future aneurysm formation is retarded. continuing pain despite ‘‘optimal’’ medical treatment, sus- picion of end organ or lower extremity ischemia, and acute Most of the acute complications of thoracic endograft aneurysmal expansion of the false lumen are all indications procedures are related to problems with access to the im- for endovascular intervention. Aortic transection from plantation site and with device implantation. Major ad- blunt trauma and acutely ruptured aorta are emerging as verse events related to the device occur in 10% to 12% of additional indications for endograft repair. patients in the initial 30-day perioperative period with stroke rate between 2.5% and 8%, spinal cord ischemia in 1.5%, acute renal failure in 1.3%, and endoleaks in 10% SURGICAL TECHNIQUE to 20% of the patients.4 Blood loss ranges from approxi- During endovascular aortic repair, a remote arterial site mately 300 to 500 mL; it may be considerably higher, (usually the femoral artery) is exposed and isolated however, as in many cases it is not readily apparent. Cat- through a small groin incision. More aggressive retro- astrophic bleeding is rare, but when it occurs, the an- peritoneal dissections may become necessary to expose the esthesiologist must be ready with large bore venous access external iliac artery if the femoral artery is small, stenotic, and available blood products. or severely calcified. The aortic anatomy is defined using fluoroscopy with particular attention toward the selection PREOPERATIVE PATIENT EVALUATION of appropriate ‘‘landing zones’’ for the endovascular stent graft. After heparinization (5,000 IU), a large endovas- As in open abdominal aortic aneurysm surgery, the pri- cular stent-graft delivery system is introduced into the re- mary goal of perioperative evaluation is to achieve mote artery over a stiff guide wire and is advanced under accurate estimation of the patient’s current condition fluoroscopic guidance to the diseased aortic segment. and the expected risk to organ function. Comorbidities When the final position of the stent graft is achieved after tend to be similar in patients scheduled for endovascular confirming patency of important branch arteries, the de- stent insertion as in those planned for open repair. The livery device is withdrawn and the endograft is deployed same anesthetic considerations should be observed, both in within the aorta. After deployment, fluoroscopy and possibly the preoperative evaluation and in selection of monitoring
- 3. Anesthesia for Endovascular Aortic Stenting 43 for the procedure (Table 1). Furthermore, intervention for a incisions. With such a wide preparation and exposure, descending thoracic aneurysm carries additional risks of temperature monitoring and maintenance is crucial. mortality and morbidity, including the risk of ischemic spinal cord injury. No data conclusively demonstrates that the prevalence of spinal cord ischemic injury is less for en- ANESTHETIC TECHNIQUES dovascular approaches than for open surgical repair.4 Different anesthetic techniques have been described for Both procedures should be classified as high-risk surgery aortic stent graft placement including local anesthesia, re- according to the American College of Cardiology/Amer- gional anesthesia, and general anesthesia (GA). With in- ican Heart Association guidelines on preoperative cardiac creasing physician experience and the development of evaluation.6 For such high-risk surgery, preoperative non- more sophisticated devices, regional anesthetics (including invasive or invasive coronary interventions (PCI) are in- epidural, spinal-epidural, and spinal) and MAC using local dicated if the patient has major or intermediate clinical anesthetics supplemented with sedation may be used. predictors of cardiac risk. However, if the patient’s cardiac However, it is important to remember that in such en- condition is stable, medical therapy should be seriously dovascular procedures, painful stimuli are concentrated at considered over PCI, especially if the urgency of the op- specific moments, separated by intervals devoid of pain; eration becomes an important factor. PCI invariably will thus, these moments of pain can be anticipated. Providing cause postponement of surgery by two months to one year. a short-acting anesthetic by bolus is preferable to con- These days, high-resolution multidetector computed to- tinuous infusion, as patient cooperation can be maintained mographic coronary angiography is gaining wide accep- better. Remifentanil (0.03 mg/kg/minute) in 0.02 incre- tance as an alternative for invasive coronary angiography, ments with midazolam is an appropriate method to pro- sparing some of the complications related to invasive ca- vide effective analgesia for patients in whom deep sedation theterization. Preliminary data provides promising scope is considered sufficient.11 for use of computed tomography preoperatively to evalu- ate patients at risk for cardiac ischemia who are scheduled for noncardiac surgery.7 In such endovascular procedures, painful Perioperative b-blockade, ACE inhibitor, and statin ther- apy are recommended to reduce the risk of cardiac morbidity stimuli are concentrated at specific moments, and mortality, especially in patients scheduled for high-risk surgery.8 b-Blockade, in particular, has been shown to reduce separated by intervals devoid of pain; thus, the risk of perioperative mortality while cessation of therapy these moments of pain can be anticipated. has been associated with an increase in short- and long-term mortality.9 Similarly, perioperative use of ACE inhibitors, although associated with greater need for vasoconstrictors, Choice of anesthetic technique is dependent on the showed a significant reduction in major vascular complica- planned surgical interventions and the patient’s comorbid tions, whereas cessation of therapy postoperatively seems to conditions. The need for extensive inguinal exploration be related to fatal and nonfatal ischemic events (studied in and dissection or for the construction of a femoral artery to recent coronary artery bypass graft patients).10 If therapy has femoral arterial conduit may favor either regional an- not been initiated already, b-blockade, ACE inhibitor, and esthesia or GA. When thoracic stent placement analysis by statin therapy should optimally be started between 30 days TEE is required, or a complex procedure is planned, or and one week before surgery. conversion to open surgery is more likely, then GA should Endovascular repair of aortic pathology carries a variable be considered. If surgical dissection is extended into the risk of sudden conversion to a laparotomy or combined surgi- retroperitoneum, a higher level of regional anesthesia or cal intervention (iliac artery exploration, arterial bypass at- GA will be necessary to provide adequate anesthesia. If the tachment of critical vessels) and thus, appropriate anesthetic patient is undergoing local anesthesia with MAC or re- monitoring should be considered. Large bore intravenous ca- gional anesthesia, adequate intravenous sedation is theters should be placed for volume replacement and a right- necessary because of agitation associated with restlessness sided arterial line. A central venous line and a pulmonary artery and pain from lying in one position for a prolonged period catheter for volume monitoring may also be indicated, and of time. The disadvantage of high epidural anesthesia is should be based on the institution’s perceived risk of conversion related to the difficulty in precisely controlling the anes- to an open repair and the patient’s comorbidities. With an thetic level, and the concern for intercostal muscle weak- average blood loss of approximately 500 mL and fluid re- ness with the need to support ventilation. For patients with quirements of approximately 3,000 mL, invasive monitoring is severe coexisting diseases, a spinal/epidural technique or a indicated in selected populations even when monitored an- continuous spinal anesthetic is likely to be a better option. esthesia care (MAC) or regional anesthesia is used. The latter may offer hemodynamic stability and more ac- Although there may be only two small incisions in the curate control of the anesthetic level.12 groin, the patient is usually prepared from the nipple line An unanswered question is whether the type of anesthesia to the knees because of the possible need to extend the used for endovascular repair affects patient outcome.
- 4. 44 Drenger and Jain Table 1. Perioperative Anesthetic Management for Endovascular Aortic Procedures Identify Patient’s Comorbidities, with Emphasis on Neurologic, Cardiac, and Renal Conditions with Preoperative Optimization Preoperative Neurologic At risk for stroke or spinal cord ischemia Comprehensive neurologic evaluation Consider with the surgeon the option of CSF drainage in high-risk patients Cardiac High risk according to ACC/AHA preoperative guidelines Follow ACC/AHA guidelines for workup (evaluation of coronary vasculature, ventricular function) Consider using coronary computed tomography angiography when delay in operation is unwarranted Perioperative b-blockade, ACE inhibitors, and statins are recommended Renal Risk for contrast-induced nephropathy Renal function tests and creatinine clearance Consider postponement of surgery until recovery if renal function deteriorated due to recent imaging test Intraoperative Hemodynamic Standard ASA monitors Continuous arterial blood pressure monitoring (preferably right radial artery), large bore intravenous access Be prepared for pharmacological intervention to slow heart rate (adenosine, b-blockers) Sudden major hemorrhage possible (visible or occult) Be prepared for significant blood loss Neurologic Consider CSF drainage Intraoperative—Keep CSF pressure at 10 cmH2O Postoperative—Keep CSF pressure at 15 cmH2O for 48 hours Consider myogenic motor evoked potential monitoring Use intravenous anesthesia, avoid volatile anesthetics. N2O is allowed If very small dose of muscle relaxant is used, keep twitch height greater than 80% Periods of pain are defined according to intervention Consider ultra-short-acting opioids when needed Cardiac TEE is essential in thoracic aorta endovascular stenting See Table 2 Renal Large dose of contrast material is used Adequate intravenous hydration with N-acetylcysteine and bicarbonate In renal dysfunction patients, consider use of low osmotic type dye and limit dye load Postoperative Cardiac Patients are at high cardiac risk Use monitored bed for 24 hours; postoperative ECG Expect cardiac morbidity (ischemia, congestive heart failure, arrhythmias) Neurologic Spinal cord ischemia is possible Maintain good hydration, and keep systolic blood pressure at preoperative values Perform neurologic examination Keep CSF drainage for 48 hours CSF ¼ cerebrospinal fluid; ECG ¼ echocardiography; TEE ¼ transesophageal echocardiography. Although stent-graft insertion is minimally invasive com- 2,387 patients, Walschot et al.15 showed that GA was an pared with the conventional procedure, the use of GA is independent risk factor for mortality after endovascular traditionally preferred by the surgeons. Several studies repair. However, the EuroSTAR study14 demonstrated no have demonstrated that GA was associated with increased advantage for any anesthetic technique regarding outcome duration of surgery, intensive care unit admissions, in- or the incidence of intraoperative complications. tensive care unit length of stay, and systemic complica- tions. Verhoeven et al.13 in a study of 239 consecutive patients and Ruppert et al.14 in a prospective multicenter PROXIMAL GRAFT DEPLOYMENT study of 5,557 patients (EuroSTAR) showed that older age Distal migration of the device occurring during proximal and greater surgical complexity are the main reasons for endograft deployment may result in inadequate exclusion the difference in patient outcomes with GA. Additional of the aneurysm sac with resultant endoleak. Device studies reached opposite conclusions about the role of GA malposition caused by inadvertent migration may result in in determining patient outcome. In a meta-analysis of either occlusion of major arterial branches or incomplete
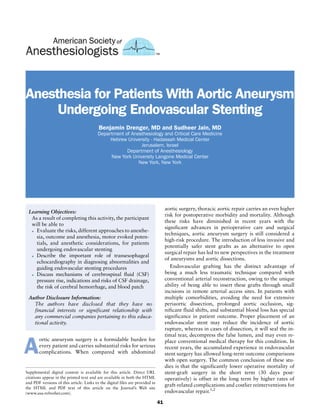
- 5. Anesthesia for Endovascular Aortic Stenting 45 Table 2. TEE Examination in Thoracic Aortic Stenting Aortic Aneurysm Identification Preoperative Evaluation Normal aortic diameters Aortic valve 23–26 mm Ascending aorta/arch 29–36 mm Descending aorta 17–26 mm Transducer angle (degrees) Short axis aortic valve 40–60 degrees Depth—6 cm from aortic valve/ Long axis aortic valve with proximal ascending aorta 90–120 degrees antiflexion use color Doppler flow Short axis ascending aorta 0 degrees Long axis aortic arch 0 degrees Short axis aortic arch 90 degrees Probe in stomach—withdraw slowly Short axis descending aorta 0 degrees Long axis descending aorta 90 degrees Aortic pathology Aortic aneurysm Ascending aorta—fusiform aneurysm Aortic arch—saccular aneurysm Descending aorta—pseudoaneurysm Aortic dissection—site of tear (entry) Stanford type A—involves ascending aorta/aortic arch Stanford type B—involves descending thoracic aorta Intraoperative Evaluation Before stent anchoring 1. Measurement of aortic dimensions 2. Aortic wall thickness diameter 3. Adequate wall length (landing zone) without aneurysm involvement below the subclavian artery 4. Visceral vessels identified Aortic Dissection 1. Classification (Stanford type A and B) 2. Proximal site of entry 3. False and true lumen identification 4. Slow flow in the false lumen 5. Guide wire positioning After stent anchoring 1. Incomplete stent-graft apposition 2. Adequate seal in healthy aorta; that is, parallel walls, consistent diameter, no luminal debris 3. Endoleaks Type 1—incompetent seal at proximal or distal stent attachment Type 2—leakage to aneurysmal sac from branch vessels Type 3—Failure of anastomosis between stent components Type 4—leakage through graft material Limitations of TEE 1. Limited view to segment of ascending aorta, behind the right bronchus, parts of arch, and abdominal segments beyond the celiac trunk 2. The need for general anesthesia TEE ¼ transesophageal echocardiography. exclusion of the aneurysm. Induced hypotension, by sodium TRANSESOPHAGEAL ECHOCARDIOGRAPHY nitroprusside or nitroglycerin, during device deployment has MONITORING been successfully used by some centers to assist in proximal endovascular stent graft placement and may reduce the With the rapid evolution of TEE technology and with the magnitude of migration. The risk of malposition may theo- esophagus being in close approximation to the aorta, TEE retically be decreased further by ventricular quiescence, has become an excellent and safe tool for diagnosing pa- which can be achieved by pharmacological induction of thology of the distal aortic arch, the descending thoracic sinoatrial and atrioventricular nodal inhibition with high- aorta, and the proximal abdominal aorta (Table 2). TEE is dose adenosine.16 an excellent tool with a high rate of accuracy in revealing
- 6. 46 Drenger and Jain renovascular disease due to atherosclerosis and/or diabetes mellitus. After successful exclusion of the aneurysm by the stent graft, there will be aneurysm sac thrombosis with subsequent hemolysis contributing to myoglobinuria. In addition, myoglobinuria may occur in cases of ischemia and reperfusion injury. All of these factors add to the risk of renal complications. The incidence of renal complica- tions after endovascular repair of an abdominal aortic aneurysm can be as high as 10% compared with 25% in open aortic surgery.21,22 Adequate hydration should be ensured and urine output closely monitored during the procedure. The intravenously injected contrast material can induce diuresis, and can give a false sense of adequate hydration and urine output if one relies solely on urine output as a measure of volume status. Central venous Figure. 1. Transesophageal echocardiography Doppler image of blood flow pressure monitoring may be a useful adjunct. Another in the aortic arch and in the subclavian artery in 35-degree angle. consequence of multiple angiograms is the increased ra- diation exposure for all personnel involved. In one review pericardial effusion, the presence of aortic regurgitation, of 47 cases over a year, the average fluoroscopy time was the extent of a dissection, and the intimal tear location approximately 40 minutes per case.23 Lead aprons at- (almost 100% of the time). It can provide instantaneous tenuate greater than 85% of the radiation dose and, if views of the location of the guide wires (95%) and an es- keeping the appropriate distance, the average exposure of timation of endograft sizing and location before deploy- an anesthesiologist was found to be 0 mSv over 6 months at ment in relation to the normal and diseased thoracic one institution.24 aorta.4 TEE appears to have distinct advantages over peri- Blood loss can be steady and considerable, but hidden, operative angiography as it provides exact vessel and lesion during endovascular repair of an abdominal aortic aneur- sizing and localization, which is difficult to obtain during ysm. Most blood loss occurs as the introducer sheaths and single plane angiography (Figure 1) (see Supplemental Di- stent grafts are passed into and out of the femoral arteries, gital Content 2, http://links.lww.com/ASA/A109). In con- and may be hidden in the surgical drapes. The actual blood trast to angiography, both endograft leakage and iatrogenic loss will depend on the amount of catheter manipulation and dissections may easily be diagnosed by TEE. Although not duration of the procedure. A sudden, unexplained decrease always possible, large intercostal arteries have been imaged, in blood pressure should alert the anesthesiologist to the thus avoiding inadvertent obstruction by the aortic stent possibility of a vascular catastrophe such as rupture, per- graft; however, consistent visualization of intercostal ar- foration, or avulsion of the aorta or a large artery. An aortic teries may not be assured in all patients. After stent-graft rupture, recognized in a timely manner, may sometimes be placement, exclusion of flow from the aorta into the aneur- amenable to treatment with intraluminal balloon tamponade ysm, thrombosis of the false lumen, and the existence of re- and subsequent deployment of the device beyond the area of sidual endoleaks can usually be confirmed using color rupture, but an emergent laparotomy is often necessary. Doppler flow imaging.17,18 TEE can also become very decisive in choosing the stent landing zone and in identifying (B mode) incomplete obliteration of the false lumen that ne- A sudden, unexplained decrease in blood cessitates additional balloon expansions of the stent (see Sup- pressure should alert the anesthesiologist to plemental Digital Content 3, http://links.lww.com/ASA/A110). Initial thrombosis of the false lumen was noticed as ‘‘smoke’’ by the possibility of a vascular catastrophe such the TEE.19 Intravascular ultrasound has been recommended in endovascular repairs. It has no advantage over TEE; however, it as rupture, perforation, or avulsion of the was found to be helpful in patients with complex anatomy and abdominal extension of the dissection.20 aorta or a large artery. INTRAOPERATIVE COMPLICATIONS AND PATIENT OUTCOME SOMATOSENSORY AND MOTOR EVOKED With multiple angiograms to position the prosthesis and to POTENTIALS check blood flow for endoleaks, approximately 250 to Today, the major risk from thoracic aortic repair procedures 300 mL of contrast will be administered during the comes from the central nervous system and not from the procedure. Contrast-induced renal failure is a serious heart. Thus, monitoring the central nervous system and the concern, particularly in those with chronic underlying spinal cord is advocated both in open surgery and in certain
- 7. Anesthesia for Endovascular Aortic Stenting 47 endovascular aortic procedures. It is indicated when a long SPINAL CORD ISCHEMIA thoracic stent is planned, with previous aortic repair in The reported incidence of neurologic injuries in the post- which segmental arteries were probably not reimplanted, operative period after endovascular thoracic aortic re- when the stent placement involves critical level—T8-L1, and construction is similar to that after open thoracic aortic in the presence of dissection or rupture. repair. Matsuda et al.29 reported an overall incidence of Rapid loss of somatosensory evoked potentials (SSEPs) paralysis of 3.7%; 6% when a large, distal thoracic section occurs soon after aortic clamping, but may also be caused of the aorta is covered by the endograft; and 12.5% when by peripheral hypoperfusion, temperature changes, an- the artery of Adamkiewicz is sacrificed.30 Open athero- esthesia, and other factors. We found a consistent distinc- sclerotic thoracic aneurysm repair carries an incidence of tion between patients who received adequate distal bypass paralysis of 2% to 8.3%.31,32 Intercostal arteries that shunting and those who did not.25 Without distal bypass, supply the anterior spinal cord may be sacrificed during SSEP disappeared within 5 to 30 minutes of aortic cross- reconstruction of the descending aorta, resulting in spinal clamping, whereas with adequate distal perfusion, the cord injury. The anterior spinal cord enjoys little if any behavior of SSEP was commensurate with the clinical reserve blood supply. The major collateral joining the neurologic outcome. In recent years, transcranial motor anterior spinal artery is the arteria radicularis magna of evoked potentials (tcMEPs) have become the preferred Adamkiewicz, which in most patients originates from an method for clinical use during high aortic surgery. The intercostal artery between the T8 and L1 level. If this cri- pressure of time under which surgeons are trying to com- tical branch is patent and emerges from the aneurysmal plete the repair during aortic cross-clamping necessitates a wall, a significant ischemic risk to the spinal cord might be very fast response time for the expression of ischemic anticipated if the vessel is excluded by the endoluminal spinal changes in EP recordings. The tcMEP method was stent. Additional supply to the distal cord comes from the found to be highly sensitive in predicting neurologic out- iliolumbar arteries and the lateral sacral arteries, branches come, with a decrease in the myogenic signal amplitude of the hypogastric arteries. Several reports demonstrated within 2 to 5 minutes after the onset of spinal cord ische- an increased incidence of poststent paralysis in patients mia.26,27 Such short notice facilitated timely, fashioned who had previously undergone operations on the abdom- surgical and anesthetic interventions such as reattachment inal aorta. It seems that during such operations, several of intercostal arteries, relocation of the aortic clamp, tributaries to the cord are sacrificed—a fact that becomes management of distal aortic perfusion, induced hyperten- crucial later, when additional endograft repair is needed. sion, and cerebrospinal fluid (CSF) drainage. The ex- Long-segment thoracic endovascular repair or con- planation offered by van Dongen et al.26 and de Haan and secutive endograft segments connected in a row also create Kalkman27 for the faster myogenic response compared a significant risk factor for spinal cord ischemia.33,34 Ap- with SSEP recording is that synaptic transmission is much plication of short endografts and avoiding the placement more sensitive to ischemia compared with axonal trans- of stent grafts between T8 and L2 is therefore re- mission. The interneurons connecting the gray to white commended to prevent spinal cord ischemia (see Supple- matter are the first to be affected by ischemia. The energy mental Digital Content 4, http://links.lww.com/ASA/ utilization of the axon to action potential propagation is A111). very low, resulting in late appearance of cell ischemia. The successful use of CSF drainage during endovascular In a series of 21 patients, Weigang et al.28 showed im- aortic repair has been described anecdotally in several case mediate, but short-term loss of tcMEPs after stent de- reports of patients who underwent thoracic aortic aneur- ployment in 3 of their patients (14%). The EPs recovered ysm repair.35,36 Clinical symptoms of paralysis were re- and no postoperative neurologic deficit was noticed, ex- solved although the primary CSF pressure upon catheter cept in one patient who suffered delayed onset paraplegia insertion was not always high, and as several rescue pro- after 21 days. The reaction to the loss of both tcMEPs and cedures are used in parallel, the relative contribution of SSEPs in this series was abrupt elevation of blood pressure each method is not clear. The increase in CSF pressure after with norepinephrine, reduction in central venous pressure stent-graft deployment might be attributed to sympathetic with nitroglycerin, and aspiration of CSF to reduce CSF spinal stimulation or to the local acidosis-induced veno- pressure to 10 cmH2O. dilation that occurs in the presence of inadequate spinal A critical disadvantage of tcMEPs is the high sensitivity cord perfusion.37 CSF drainage should be continued for 48 to volatile anesthetics and muscle relaxants. Thus, when to 72 hours, and strict control of hemodynamic status EP monitoring is planned, intravenous anesthesia should maintained to prevent hypotension. be used with no volatile anesthetics. N2O can be used ex- cept for patients in whom nerve conduction defects were previously noted. If muscle twitch height is continuously CEREBROVASCULAR COMPLICATIONS OF CSF monitored electronically, a small infusion dose of vecur- DRAINAGE onium (30 mg/kg/hour) to maintain 80% of the twitch height can be performed without interfering with the Stroke after high aortic surgery is a devastating complica- quality of EP monitoring26 (B.D., personal experience). tion and is usually thromboembolic in origin, which can
- 8. 48 Drenger and Jain result in either an ischemic or a hemorrhagic presentation. 3. Prinssen M, Verhoeven ELG, Buth J, et al.: A randomized trial Recently, after sporadic reports of intracranial hemorrhage comparing conventional and endovascular repair of abdominal aortic aneurysms. New Engl J Med 2004; 351:1607–18. occurring while spinal catheters were still in place, CSF 4. Hiratzka LF, Bakris GL, Beckman JA, et al.: ACCF/AHA/AATS/ACR/ drainage was implicated as a possible explanation for the ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and cerebral bleeding.38,39 Dardik et al.39 retrospectively re- management of patients with thoracic aortic disease. J Am Col Cardiol 2010; 55:e27–129. corded 8 of 230 patients (3.5%) who developed subdural 5. Criado FJ, Clark NS, Barnatan MF: Stent graft repair in the aortic hematomas. In their multivariate analysis, they emphasized arch and descending thoracic aorta: A 4-year experience. J Vasc Surg 2002; 36:1121–8. that the only significant factor correlating with the occur- 6. Fleisher LA, Beckman JA, Brown KA, et al.: ACC/AHA 2007 rence of subdural hematoma was large volume of CSF guidelines on perioperative cardiovascular evaluation and care for drained. However, only one patient developed neurologic noncardiac surgery: A report of the American College of Cardiology/ symptoms while the spinal drainage catheter was still in American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Society of Echocardio- place. Despite the conflicting data, the role of CSF drainage graphy, American Society of Nuclear Cardiology, Heart Rhythm as a causative factor in subarachnoid, intracerebral, or sub- Society, Society of Cardiovascular Anesthesiologists, Society for tentorial hemorrhage should be addressed. It has been at- Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. J Am Coll tributed to a cerebral hypotension related traction effect, Cardiol 2007; 50:e159–e241. which subsequently may trigger a tear of bridging veins and 7. Durst R, Bogot N, Gilon D, Drenger B: Potential role for coronary computerized angiography for assessing preoperative ischemic risk. intracranial hemorrhage.40 A substantial loss of CSF may J Cardiothorac Vasc Anesth 2010; 24:348–55. retract the brain from the meninges, or in the case of the 8. Poldermans D, Bax J, Boersma E, et al.: Guidelines for pre-operative cerebellum, from the tentorium. This may cause a temporary cardia risk assessment and perioperative cardiac management in non- occlusion of stretched veins, increasing the intraparen- cardiac surgery. Eur Heart J 2009; 30:2769–812. 9. Wallace A, Au S, Cason B: Association of the pattern of use of chymal venous pressure and creating the appropriate en- perioperative b-blockade and postoperative mortality. Anesthesi- vironment for venous hemorrhage.41 Recently, Franzini ology 2010; 113:794–805. 10. Drenger B, Gozal Y, Fontes M, Mangano D: McSPI members: The et al.42 proposed that the normally antireflux venous valves association between ACE inhibitors pattern of use and patient in the systemic venous system prevent pressure buildup in the outcome after coronary artery bypass surgery. Anesthesiology 2006; spinal cord, thus exerting an aspiration mechanism in the 105: A1737. spinal cord veins that disappears in the presence of a dural 11. Bonfreschi V, Giuliani E, Malagnino FC, et al.: Analgesia during abdominal aortic aneurysm endovascular repair: remifentanil versus hole. The CSF leak may persist unless a blood patch is placed fentanyl-midazolam: A randomized controlled trial. Eur J Anaes- to reverse the CSF blood gradient. The main purpose of an thesiol 2009; 26:782–7. epidural blood patch is not to seal the dura; rather, it is to 12. Mathes DD, Kern JA: Continuous spinal anesthesia technique for endovascular aortic stent graft surgery. J Clin Anesth 2000; 12:487–90. provoke a rise in the epidural pressure, no matter where the 13. Verhoeven ELG, Cina CS, Tielliu IFJ, et al.: Local anesthesia for ` blood patch was performed in relation to the original dural endovascular abdominal aortic aneurysm repair. J Vasc Surg 2005; 42:402–9. hole, and thus to reinstitute the function of the antireflux 14. Ruppert V, Leurs LJ, Steckmeier B, et al.: Influence of anesthesia type venous valves. on outcome after endovascular aortic aneurysm repair: An analysis based on EUROSTAR data. J Vasc Surg 2006; 44:16–21. 15. Walschot LHB, Laheij RJF, Verbeek ALM: Outcome after endovas- POSTOPERATIVE CARE cular abdominal aortic aneurysm repair: A meta-analysis. J Endovasc Ther 2002; 9:82–9. In the postoperative period, after successful exclusion of 16. Kahn RA, Moskowitz DM, Marin M, Hollier L: Anesthetic the aortic aneurysm, thrombosis will occur in the excluded considerations for endovascular aortic repair. Mt Sinai J Med 2002; aneurysmal sac. Platelet count invariably decreases due to 69:57–67. 17. Fattori R, Caldarera I, Rapezzi C, et al.: Primary endoleakage in thrombosis, and this may sometimes result in clinically endovascular treatment of the thoracic aorta: Importance of significant thrombocytopenia and fever, and rarely a con- intraoperative transesophageal echocardiography. J Thorac Cardio- sumptive coagulopathy. This postimplantation syndrome vasc Surg 2000; 120:490–5. 18. Orihashi K, Matsuura Y, Sueda T, et al.: Echocardiography-assisted may be attributed to a significant inflammatory response surgery in transaortic endovascular stent grafting: Role of transeso- resulting in endothelial and macrophage cell activation phageal echocardiography. J Thorac Cardiovasc Surg 2000; from intraaneurysmal device manipulation. We should 120:672–8. 19. Gonzalez-Fajardo JA, Gutierrez V, San Roman JA, et al.: Utility of keep in mind that this high-risk group of patients share a intraoperative transesophageal echocardiography during endovascu- similar postoperative course to those operated on for aor- lar stent-graft repair of acute aortic dissection. Ann Vasc Surg 2002; tic aneurysm resection, and thus, close monitoring for 24 16:297–303. 20. Koschyk DH, Nienaber CA, Knap M, et al.: How to guide stent-graft to 48 hours is recommended. implantation in type B aortic dissection? Comparison of angiography, transesophageal echocardiography, and intravascular ultrasound. Circulation 2005; 112(suppl I):I-260–I-264. REFERENCES 21. Alsac JM, Zarins CK, Heikkinen MA, et al.: The impact of aortic endografts on renal function. J Vasc Surg 2005; 41:926–30. 1. Greenhalgh RM: United Kingdom EVAR Trial Investigators: En- 22. Fairman RM, Criado F, Farber M, et al.: Pivotal results of the dovascular versus open repair of abdominal aortic aneurysm. N Engl Medtronic vascular Talent thoracic stent graft system: The J Med 2010; 362:1863–71. VALOR trial. J Vasc Surg 2008; 48:546–54. 2. Greenhalgh RM: United Kingdom EVAR Trial Investigators: En- 23. Lipsitz EC, Weith FJ, Ohki T, et al.: Does the endovascular repair of dovascular repair of aortic aneurysm in patients physically ineligible aortoiliac aneurysms pose a radiation safety hazard to vascular for open repair. N Engl J Med 2010; 362:1872–80. surgeons? J Vasc Surg 2000; 32:704–10.
- 9. Anesthesia for Endovascular Aortic Stenting 49 24. Park KW, Hamdan A. Anesthesia for endovascular repair of 34. Greenberg RK, Lu Q, Roselli EE, et al.: Contemporary analysis of de- abdominal aortic aneurysm. In: Progress in Anesthesiology XVI ed. scending thoracic and thoracoabdominal aneurysm repair: a comparison Philadelphia: Lippincott Williams Wilkins, 2002, pp 147–160. of endovascular and open techniques. Circulation 2008; 118:808–17. 25. Drenger B, Parker SD, McPherson RW, et al.: Spinal cord stimulation 35. Oberwalder PJ, Tiesenhausen K, Hausegger K, Rigler B: Successful evoked potentials during thoracoabdominal aortic aneurysm surgery. reversal of delayed paraplegia after endovascular stent grafting. Anesthesiology 1992; 76:689–95. J Thor Cardiovasc Surg 2002; 124:1259–60. 26. van Dongen EP, ter Beek HT, Schepens MA, et al.: The relationship 36. Fleck T, Hutschala D, Weissl M, et al.: Cerebrospinal fluid drainage between evoked potentials and measurements of S-100 protein in as a useful treatment option to relieve paraplegia after stent-graft cerebrospinal fluid during and after thoracoabdominal aortic implantation for acute aortic dissection type B. J Thor Cardiovasc aneurysm surgery. J Vasc Surg 1999; 30:293–300. Surg 2002; 123:1003–5. 27. de Haan P, Kalkman CJ: Spinal cord monitoring: Somatosensory- and 37. Drenger B, Parker SD, Frank SM, Beattie C: Changes in cerebrospinal motor-evoked potentials. Anesthesiol Clin North America 2001; fluid pressure and lactate concentrations during thoracoabdominal 19:923–45. aortic aneurysm surgery. Anesthesiology 1997; 86:41–7. 28. Weigang E, Hartert M, Siegenthaler MP, et al.: Neurophysiological 38. McHardy FE, Bayly PJ, Wyatt MG: Fatal subdural haemorrhage monitoring during thoracoabdominal aortic endovascular stent graft following lumbar spinal drainage during repair of thoraco-abdom- implantation. Eur J Cardiothorac Surg 2006; 29:392–6. inal aneurysm. Anaesthesia 2001; 56:168–70. 29. Matsuda H, Fukuda T, Iritani O, et al.: Spinal cord injury is not 39. Dardik A, Perler BA, Roseborough GS, Williams GM: Subdural negligible after TEVAR for lower descending aorta. Eur J Vasc hematoma after thoracoabdominal aortic aneurysm repair: An Endovasc Surg 2010; 39:179–86. underreported complication of spinal fluid drainage? J Vasc Surg 30. Morales JP, Taylor PR, Bell RE, et al.: Neurological complications 2002; 36:47–50. following endoluminal repair of thoracic aortic disease. Cardiovasc 40. Leyvi G, Ramachandran S, Wasnick JD, et al.: Risk and benefits of Intervent Radiol 2007; 30:833–9. cerebrospinal fluid drainage during thoracoabdominal aortic aneur- 31. Richards JM, Nimmo AF, Moores CR, et al.: Contemporary results ysm surgery. J Cardiothorac Vasc Anesth 2005; 19:392–9. for open repair of suprarenal and type IV thoracoabdominal aortic 41. Settepani F, van Dongen EP, Schepens MA, Morshuis WJ: Intracer- aneurysms. Br J Surg 2010; 97:45–9. ebellar hematoma following thoraco abdominal aortic repair: an 32. Schepens MA, Heijmen RH, Ranschaert W, et al.: Thoracoabdominal unreported complication of cerebrospinal fluid drainage. Eur J aortic aneurysm repair: Results of conventional open surgery. Eur J Cardiothorac Surg 2003; 24:659–61. Vasc Endovasc Surg 2009; 37:640–5. 42. Franzini A, Messina G, Nazzi V, et al.: Spontaneous intracranial 33. Gravereaux EC, Faries PL, Burks JA, et al.: Risk of spinal cord hypotension syndrome: A novel speculative physiopathological ischemia after endograft repair of thoracic aortic aneurysms. J Vasc hypothesis and a novel patch method in a series of 28 consecutive Surg 2001; 34:997–1003. patients. J Neurosurg 2010; 112:300–6.