PA_Pro_August_2016-final
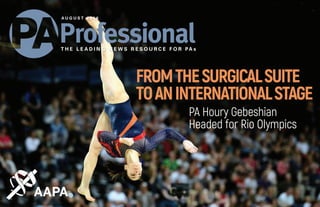
- 1. PA Houry Gebeshian Headed for Rio Olympics FROMTHESURGICALSUITE TOANINTERNATIONALSTAGE T H E L E A D I N G N E W S R E S O U R C E F O R PA s A U G U S T 2 0 1 6
- 2. Today, we helped Jennifer find the latest clinical guidelines on managing her patients with psoriasis. Next week, we will help her maintain her certification with free and discounted self-assessment CME in Learning Central. Next month, we will provide her with 24/7 online access to sessions from AAPA 2016 with AAPA Conference on Demand. Next year, we will make sure she aces PANRE – and saves – with AAPA PANCE/PANRE Review, powered by Hippo Education. ThThroughout her career, we will provide the leading CME resources Jennifer needs, whenever she needs it. And because she’s an AAPA member, she saves hundreds each year. Just one of the ways we help you practice strong. Explore it all. aapa.org/learn STRONGER. TOGETHER.
- 3. ContentsA U G U S T 2 0 1 6 • V O L . 8 , N O . 7 ABOUT THE COVER The Wall Street Journal named PA Houry Gebeshian one of the gymnasts to watch at the Rio Olympics. Photo courtesy of Houry Gebeshian Inside C O V E R S T O R Y From the Surgical Suite to an International Stage PA Houry Gebeshian Headed for Rio Olympics S I D E B A R Answering the Call to Provide Care at Olympics F E AT U R E S T O R I E S Learning to Lead PAs Taking Their Place at the Table Offering Students a Glimpse of the Future AAPA’s Preceptor of the Year: PA Maureen Barrett 18 23 32 26 Departments Laws + Legislation The Colorado Academy coalition leads to sweeping harmonization act Payment Matters CMS clarifies PA ordering of restraint and seclusion STAT AAPA statement in response to NCCPA press release | PAs eligible to prescribe buprenorphine for opioid addiction | The Hospitalist profiles PAs in executive leadership | AAPA responds to Dear Abby column | and more Professional Practice Contract negotiation tips for early career PAs Reflections Life lessons a PA learned hiking the Appalachian Trail 7 10 13 36 38 PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 1
- 4. When It Comes To Protecting Your Career These Are The Only Three Letters You’ll Ever Need To Remember. The Country’s Leading Malpractice Insurance Program For PAs. n AAPA Endorsed Insurance Provider For 20 Years. n Occurrence, Claims-Made & Tail Coverage Options. n Full Time, Part Time, Moonlighting & Student Liability. n Insuring Over 100,000 Healthcare Professionals. Quality, Trust & Value www.CMFGroup.com & 99 Hudson Street, 12th Floor New York, NY 10013-2815 1-800-221-4904 Fax: 646-390-5163 Email: info@cmfgroup.com www.CMFGroup.com Most credit cards accepted Like us at facebook.com/cmfgroupinsurance Follow us on twitter.com/cmfgroup_
- 5. Get hired for your next PA position! Chat live & one-on-one Chat one-on-one with recruiters and interview with employers who have nationwide PA openings in all settings and specialties. Register today Register today and log in any time before the event to learn more about participating employers and new career opportunities. Build your network Build your network by continuing conversations with recruiters after the event. AAPA Virtual Career Fair Wednesday, October 12th, 12-3 PM EDT REGISTER HERE! MPAS Degree Advancement Option Division of Physician Assistant Education Requirements § Graduate of accredited PA program and possess a baccalaureate degree § Current or prior NCCPA certification § Physician/Mentor who agrees to be your preceptor Learn more and apply at: unmc.edu/alliedhealth/padao | 402-559-6673 Program Highlights § Over 30 years of proven success granting master’s degrees to nearly 2000 practicing PAs § 36 semester credit hours of courses including a clinical or education track § Affordable program with no required resident time on the UNMC campus § Graduate in 5 semesters with up to 5 years to complete studies
- 6. © Copyright 2016 by the American Academy of PAs. PA Professional is published monthly and is a registered trademark of AAPA, 2318 Mill Road, Suite 1300, Alexandria, VA 22314-6868. MAGAZINE STAFF PUBLISHER Steve Gardner sgardner@aapa.org EDITOR-IN-CHIEF Janette Rodrigues jrodrigues@aapa.org WRITER/EDITOR Steven Lane slane@aapa.org STAFF WRITER Sarah Sonies ssonies@aapa.org GRAPHIC DESIGNER Joan Dall’Acqua jd@acquagraphics.com CLASSIFIED AND DISPLAY ADVERTISING SALES Tony Manigross 571-319-4508 tmanigross@aapa.org 2318 Mill Road, Suite 1300 Alexandria, VA 22314-6868 PH: 703-836-2272 | FX: 703-684-1924 EM: aapa@aapa.org | WB: aapa.org AAPA BOARD OF DIRECTORS 2016–2017 PRESIDENT AND CHAIR OF THE BOARD Josanne K. Pagel, MPAS, PA-C, Karuna® RMT, DFAAPA PRESIDENT-ELECT L. Gail Curtis, MPAS, PA-C, DFAAPA IMMEDIATE PAST PRESIDENT Jeffrey A. Katz, PA-C, DFAAPA VICE PRESIDENT AND SPEAKER OF THE HOUSE David I. Jackson, DHSc, PA-C, DFAAPA SECRETARY-TREASURER Jonathan E. Sobel, PA-C, MBA, DFAAPA, FAPACVS FIRST VICE SPEAKER William T. Reynolds, Jr., MPAS, PA-C, DFAAPA SECOND VICE SPEAKER Todd A. Pickard, MMSc, PA-C DIRECTOR-AT-LARGE Laurie E. Benton, PhD, MPAS, PA-C, RN, DFAAPA DIRECTOR-AT-LARGE Diane M. Bruessow, MPAS, PA-C, DFAAPA DIRECTOR-AT-LARGE Lauren G. Dobbs, MMS, PA-C DIRECTOR-AT-LARGE David E. Mittman, PA, DFAAPA DIRECTOR-AT-LARGE Beth R. Smolko, MMS, PA-C STUDENT DIRECTOR Joseph D. Sutherland CHIEF EXECUTIVE OFFICER Jennifer L. Dorn, MPA V O L 8 | N O 7 | A U G U S T 2 0 1 6 AAPA.ORG PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 4
- 7. Your AAPA Membership Has Benefits! Voluntary Group Short Term and Long Term Disability Insurance Protect your most valuable asset, your paycheck! Protection will replace a portion of your income when a sickness, injury or pregnancy keeps you from working; up to $4,000 per month in Short Term and $8,000 per month in Long Term Benefits. 1. New eligible AAPA Fellows who apply within the first 60 days of membership are guaranteed to be accepted. No medical questions or records required! AAPA Fellow members with a date of membership longer than 60 days can still apply, but medical underwriting is required. 2. Discounted Premiums- 50% lower than individual disability policies with similar features. 3. Short Term disability coverage has no preexisting condition limitation (for eligible applicants). 4. Benefits can be used immediately upon your effective date - guaranteed acceptance applicants do not have to satisfy any time period before filing a claim. Contact us for more details. 5. Benefits do not offset individual disability coverage you may have in place. Want to learn more? www.MyPABenefits.com If you are not covered by a group disability insurance plan, now is the time to consider enrolling in this valuable coverage. If you already have 60% of your earnings covered by a group disability plan through your employer, and would like information on how to increase that benefit to 75-80%, contact Ryan Insurance Strategy Consultants directly at 800-796-0909 ext. 107. "Protecting Your Financial Plans Since 1978" NEW PROFESSIONAL LAB COATS SLIM FIT, SOPHISTICATED STYLE AAPA MEMBERS RECEIVE 15% OFF ENTER CODE AAPAMEM15 AAT CHECKOUT To place an order, visit www.medelita.com
- 8. SoFimemberswhorefinance theirstudentloanssavean averageof$19K1 . NowAAPAispartneringwith SoFitosaveyouevenmore. ApplythroughSoFi.com/AAPAtogeta $300bonus2 forstudentloanrefinancing. TermsandConditionsApply.SOFIRESERVESTHERIGHTTOMODIFYORDISCONTINUEPRODUCTSANDBENEFITSATANYTIMEWITHOUTNOTICE.Seesofi.com/legalforacomplete listoftermsandconditions.SoFiloansareoriginatedbySoFiLendingCorp(dbaSoFi)CaliforniaFinanceLender#6054612.NMLS#1121636.1 Seesofi.com/disclaimer12 Ifyouapplythrough SoFi.com/AAPA,paymentwillbeissuedelectronicallyonceyoubecomeaSoFiborrower;youhavesubmittedacompletedapplicationwithdocumentsandyourloanhasbeendisbursed. Offergoodfornewcustomersonly. Opportunity for Emergency Department PA-C FA C U LT Y The Baylor College of Medicine, a top medical school, is looking for stellar candidates to join us to work in the world’s largest medical center. We are recruiting experienced Physician Assistants who will be an integral part of our Emergency Medicine team at BCM. Our need is night and weekend shifts, and we offer highly competitive academic salary and benefits. The program is based out of Ben Taub General Hospital, a busy Level 1 trauma center in the heart of Houston that sees more than 100,000 emergency visits per year. BCM is affiliated with eight world class hospitals and clinics in the renowned Texas Medical Center. These affiliations, along with the medical school’s preeminence in research, help to create one of the strongest emergency medicine programs/experiences in the country. F E L L O W S H I P The program also recruits biannually for the Physician Assistant Fellowship program for those recently out of school or interested in gaining Emergency Medicine experience. Those interested in a position or further information may contact PA Amanda Reynado via email reynado@bcm.edu or by phone at 713-873-2626. BCM_MLP_AD-1.indd 1 5/23/16 12:43 PM Join us for the 2016 CAPA Annual Conference in the city of Winnipeg October 27 to 30, 2016 • The Fairmont Winnipeg Hotel,Winnipeg, MB Canadian Association of Physician Assistants Register at capa-acam.ca Experience Canadian Continuing Professional Development at its finest
- 9. LAWS+LEGISLATION Big Legislative Win for Colorado PAs PAs Added Throughout State Statutes B Y A D A M S . P E E R ADAM S. PEER, is an AAPA director of constituent organization outreach and advocacy. Contact him via email or 571-319-4314. B y anyone’s measure, June 1, 2016, was a ground- breaking day for PAs in Colorado: Gov. John Hickenlooper signed Senate Bill 158 into law. Known as the“harmonization act,”this legislation strategically adds PAs to sections throughout Colorado’s statutes, removing significant barriers to patient care. Collaboration between the Colorado Academy of PAs (CAPA) and AAPA led to its passage. The new law goes into effect Aug. 10, 2016. This is the largest legislative undertaking by CAPA since the original PA law was enacted in 1983. CAPA President Meg Townsend, President-elect Meagan Hillman, and Immediate Past President Brenda VanderWel, worked closely with AAPA to review all 44 titles of Colorado statutes. Their meticulous efforts identified the most effi- cient and sensible places to include PAs where other healthcare providers were listed. The first draft was nearly 300 pages long. “There was so much uncertainty during the first stake- holder meeting,”recalled Townsend.“The legislative change that our organization was requesting was massive. Gov. John Hickenlooper signs Senate Bill 158 into law at the Children's Hospital of Colorado. Front row: Hickenlooper and children. Back row, left to right, PA Jocelyn Cavender, state Rep. Dianne Primavera and PAs Meg Townsend, Alysia Wiley and Meagan Hillman. PHOTOCOURTESYOFCAPA PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 7
- 10. LAWS+LEGISLATION | continued However, by the time we left the meeting we had a stronger strat- egy and formed new alliances with stakeholders for PAs.” The story behind this legislation has roots in Seattle. During the 2015 Legislative Summit of the National Conference of State Legis- latures, AAPA staff sat next to state Sen. Kevin Lundberg, chair of the Colorado Senate Health and Human Services (HHS) Committee, and started a conversation about the important role PAs play in healthcare. Lundberg normally does not sponsor legislation before his com- mittee. However, after several months of work, he decided to intro- duce SB158. State Rep. Dianne Primavera introduced the state House version of the bill. It was well received, unanimously passing out of the state Senate HHS Committee. CAPA testified along with representatives of the Colorado Medical Society, Colorado Academy of Family Physicians, Colorado Community Health Network, and the Division of Workers’ Compensation in both chambers. The bill received no opposing testimony. It was adopted unanimously by both sides of the state legislature. “One of the key aspects achieved during the project was board cohesiveness,”said Townsend.“Now we’re a board that’s 100 percent united—we have clear goals and a firm strategy to achieve them.” This legislative victory also opened up excellent opportunities to engage with other groups active in Colorado’s healthcare issues. This will lead to further discussions on how the laws can better authorize expanded roles for PAs in other areas of healthcare, including mental health. What Is a Harmonization Act? Generally, a harmonization act is legislation that amends various sections of the law that may only mention physicians, or physi- cians and NPs, to include PAs. The results not only mean that there is no longer con- fusion over whether or not PAs can perform a medical function that they are qualified to perform, but that when new sections of law and regulations are drafted in the future, legislators and regulators will include PAs. What did Senate Bill 158 do? ■ Clarifies that PAs may perform any act that has been delegated by a physician— including signing forms, making certain statements and making certain findings or declarations ■ Allows certain patients direct access to PAs by naming PAs as primary care providers ■ Specifies that under workers’compensa- tion, level I accreditation is also extended to PAs ■ Removes the requirement that a physician’s name must appear on prescriptions issued by a PA, except for controlled substances PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 8
- 11. PATIENTS FIRST. Cyndy Flores, PA-C Regional Medical Center of San Jose “It’s why we went into medicine, and that’s easily lost. CEP America walks the walk by keeping the patients in focus. CEP America knows how to care for patients across the Acute Care Continuum. Team-based practices are more efficient and effective for great care.” YOUR LIFE. YOUR CAREER. YOUR PARTNERSHIP. To learn more about a career with CEP America visit: go.cep.com/topcareer In health care, knowledge is what elevates you. And, while doctors and patients count on your knowledge, staying on top of your game in this ever-changing profession can be a challenge. Oakstone’s family of products – including CMEinfo and Practical Reviews – is your go-to source for evidence-based specialty reviews, clinical updates and journal reviews. Explore credit-earning opportunities in 40+ specialties at Oakstone.com, and you’ll learn you can rely on us the same way your patients rely on you: to be a trusted, authoritative source of critical information. Education for Every Stage of Your Career. Oakstone.com | 800.633.4743 SPECIAL LIMITED TIME OFFER! Save 35% at Oakstone.com with discount code AAPA35 Some restrictions apply. Offer expires 7/31/16. Cannot be combined with other discounts. Min. purchase $399.
- 12. PAYMENTMATTERS CMS Clarifies PA Ordering of Restraint and Seclusion AAPA Calls on PAs to Support Change B Y M I C H A E L P O W E W e all know that words matter. That may be especially true when it comes to regulatory language that authorizes or guides the inter- pretation of how PAs and other healthcare professionals deliver care to patients. For years, the Medicare program, which is administered by CMS, has been using an anti- quated and confusing term to describe who could order restraint and seclusion in hospitals. The problematic term is“licensed independent practitioner,”or LIP. Responding to protracted lobbying efforts by AAPA, CMS issued a proposed rule,“Medicare and Medicaid Programs; Hospital and Critical Access Hospital (CAH) Changes to Promote Innovation, Flexibility, and Improve- ment in Patient Care,”on June 15. One provision of the proposed rule would officially change the term“licensed independent practitioner”to“licensed practitioner”in order to improve hospitals’utilization of PAs. MICHAEL POWE is AAPA vice president of reimbursement and professional advocacy and an adjunct assistant professor at The George Washington University School of Medicine and Health Sciences. Contact him at michael@aapa.org or 571-319-4345. PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 10
- 13. PAYMENT MATTERS | continued AAPA applauds CMS’recognition that PAs have the education and exper- tise to provide this level of care. As CMS noted in the proposal,“PAs are trained on a medical model that is similar in content, if not duration, to that of physicians.”CMS language in the proposal goes on to say that“Fur- ther, PA training and education is comparable in many ways to that of APRNs and in some ways, more extensive.” Brief History LIP is not a term that emanates from a law or statute. Rather, it’s a term created by CMS and also used by The Joint Commission (JC). Because the term contained the word“independent,”there were questions as to whether PAs—who practice medicine autonomously, but collaborate with physicians—were included as LIPs. Over the years, some hospitals contin- ued to be confused as to whether PAs were included among those profes- sionals who were officially authorized to order restraint and seclusion, as allowed by state law and facility policy. In previous comments to CMS, AAPA recommended that the word“inde- pendent”be struck from any term describing qualified healthcare profes- sionals, arguing that“independence”is not a measure of a healthcare pro- fessional’s educational preparation, competency or ability to provide quality medical care. Eliminating confusing language supports increased patient access to care, improves team-based healthcare delivery and allows PAs to work at the top of their license. Previous CMS Interpretation Was Positive The existing LIP language did not necessarily exclude PAs from ordering restraint and seclusion, but it did create confusion. AAPA worked exten- sively with CMS to obtain a PA-friendly interpretation of the LIP terminol- ogy. As far back as 2006, and in direct response to AAPA’s comments to a CMS rule, CMS issued the following statement,“For the purposes of this rule, a LIP is any individual permitted by State law and hospital policy to order restraints and seclusion for patients independently, within the scope of the individual’s license and consistent with the individually granted clinical privileges. This provision is not to be construed to limit the author- ity of a physician to delegate tasks to other qualified healthcare personnel, that is, physician assistants and advanced practice nurses, to the extent recognized under State law or a State’s regulatory mechanism, and hospi- tal policy. It is not our intent to interfere with State laws governing the role PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 11
- 14. PAYMENT MATTERS | continued BUT WE STILL HAVE MORE TO DO. Keep reminding your patients to read and follow their labels, and to only take one medicine with acetaminophen at a time. Get your free Know Your Dose education materials online. Thanks to you, more Americans than ever know how to use acetaminophen safely. 10 MILLION EDUCATIONAL MATERIALS DISTRIBUTED CONSUMER AWARENESS HITS ALL-TIME HIGH EDUCATION REACHES 400 MILLION AMERICANS UNINTENTIONAL MISUSE DRAMATICALLY DECLINES Adding Your Voice Go here to tell CMS you support clarifying a PA’s ability to order restraint and seclusion. of physician assistants, advanced practice registered nurses, or other groups that in some States have been authorized to order restraint and seclusion or, more broadly, medical interventions or treatments.” While this statement is certainly useful, those making utilization and employment decisions in hospitals may not have had access to this lan- guage or may have chosen to adopt a more conservative interpretation. Conclusion The proposed rule, once finalized, will help eliminate confusion about the right of PAs to order restraint and seclusion under the Medicare program. In addition, AAPA will ask that the JC align itself with CMS policy and elimi- nate the term LIP in its manuals and publications. AAPA will submit formal comments to CMS in support of the proposed change. Comments are due to CMS by August 15.
- 15. STAT | Industry News AAPA STATEMENT IN RESPONSE TO NCCPA PRESS RELEASE The recent decision by the AAPA Board of Direc- tors to investigate the creation of an alternative certifying body for PAs was made after careful deliberation, extensive communications with the leadership of the NCCPA and in response to the large number of concerns voiced by PAs to AAPA. The decision to explore the establishment of a new certification organization was not made lightly and reflects the priority of PAs to put patient care ahead of burdensome and unnecessary recertifica- tion testing. The Board’s action was the direct result of the overwhelming vote by the AAPA House of Del- egates (HOD) in May to reject the principles that underlie NCCPA’s recertification proposal. NCCPA is incorrect when it asserts that AAPA hasn’t engaged with it about the proposal. We have. At AAPA’s invitation, NCCPA spoke to national and state PA leaders at the Academy’s Leadership and Advocacy Summit in February and, in an unprecedented move, addressed the HOD in May. The AAPA Board has also issued numerous invitations to speak directly with NCCPA leaders, which have been rebuffed or pushed off to lawyers. AAPA’s invitation for a board-to-board dialogue remains open. NCCPA is incorrect when it says it has evidence that recertification testing helps patient outcomes. PA Josanne Pagel AAPA TO TAKE NEXT STEPS TOWARD CREATING NEW PA CERTIFYING BODY At its July meeting, the AAPA Board of Directors unanimously voted to take the next steps toward establishing a new certifying organization by gath- ering more information and developing the neces- sary documents. “The changes to the recertifica- tion process proposed by NCCPA would have such a significant det- rimental impact on PA practice and patient access to care that the AAPA Board decided it would be pru- dent to begin the work necessary to establish a new certifying body,” said AAPA President Josanne Pagel. “Of course, we continue to hope that NCCPA will accept our invita- tion, which was extended after the May HOD meeting and again after our most recent Board meeting, to discuss its recertification exam proposal with us directly, board to board.” For more information on the NCCPA recertifica- tion proposal and the latest news on AAPA's ongo- ing response, visit www.news-center.aapa.org. Here is NCCPA's response to AAPA's decision to take the next steps toward creating a new PA certifying body. There simply is no such evidence. NCCPA is espe- cially incorrect when it says that PAs support its recertification proposal. We have heard—and hear daily—from individual PAs and the elected representatives of constituent organizations who disagree with the NCCPA plan. AAPA has not yet decided to stand up a new organization. The Acad- emy will continue to take the steps that are in the best interest of PAs and the patients they serve. For more information on this issue, please visit and bookmark this website. THE HOSPITALIST PROFILES PAs IN EXECUTIVE LEADERSHIP The Society of Hospital Medicine’s The Hospitalist reports on the evolving role of PAs and nurse practitioners NPs in hospital medicine groups and health systems.“Some PAs and NPs have ascended to positions of leadership in their HM groups or health systems, in some cases even supervising the physicians.” The Hospitalist interviewed five PAs for the arti- cle, including AAPA Director-at-Large Laurie Benton and PA Michael Huckabee, director of the Division of Physician Assistant Education at the University of Nebraska Medical Center in Omaha. Read more about PAs in executive leadership and management on page 26 of this issue of PA Pro. PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 13
- 16. STAT | continued AAPA RESPONDS TO DEAR ABBY COLUMN AAPA responded to mislead- ing information about PAs published recently in a“Dear Abby”column. While the original question and Abby's response were concerning, it was heartening to see the many positive responses in support of PAs in the com- ments to the story. AAPA encourages PAs and PA stu- dents to provide clarifying comments regarding misin- formation about PAs in any publication or public forum. TELL CMS YOU SUPPORT PAs’ ABILITY TO ORDER RESTRAINT AND SECLUSION Responding to AAPA’s lobbying efforts, CMS issued a proposed rule containing a provision to officially remove an antiquated regulatory term,“licensed inde- pendent practitioner,”to avoid continued confusion regarding hospitals’utilization of PAs. Add your voice and tell CMS that you strongly sup- port their proposal to use the term“licensed practitio- ner,”especially when it comes to determining which health professionals are authorized to order restraint and seclusion for patients in hospitals. The new term will make it clear that PAs are included among the pro- fessionals who can order restraint and seclusion for Medicare beneficiaries. Some hospitals are confused as to whether PAs are able to order restraint and seclusion due to the word“independent.”The proposed language change will remove that uncertainty. Learn more here and see story on page 10. PAs ELIGIBLE TO PRESCRIBE BUPRENORPHINE FOR OPIOID ADDICTION Over the past year, AAPA aggressively lobbied for PAs to be part of the solution to the nation’s opioid epidemic. As a result of our efforts, PAs will soon be eligible to become waiv- ered to prescribe buprenorphine for the treatment of opioid addiction. On July 8, the U.S. House of Representatives over- whelmingly supported passage of the House-Senate Con- ference report to S. 524, the Comprehensive Addiction and Recovery Act (CARA) of 2016 and the U.S. Senate followed suit on July 13. The legislation amends federal law (the Drug Addiction Treatment Act of 2000 or DATA 2000) to permit PAs to become waivered to prescribe buprenorphine for the treat- ment of opioid addiction. It will now be sent to the president for his expected signature. “As a PA with a background in addiction medicine and com- munity health clinics, I am pleased Congress is bringing more resources to bear to tackle the opioid addiction crisis in this country,”said AAPA President Josanne Pagel.“The inclusion of PAs in CARA is crucial to our ability to provide proven treat- ment options to more Americans suffering from addiction.” Although CARA was crafted in a bipartisan manner, funding was a contentious issue leading up to the bill’s passage and shaped many of the bill’s final provisions. This was because the Congressional Budget Office gave the bill a high cost esti- mate for the Medication-Assisted Treatment (MAT) Program, Section 303, of the bill. This unexpectedly high cost ultimately determined the conditions in which DATA 2000 was amended to permit PAs and nurse practitioners NPs to become waiv- ered to prescribe buprenorphine for the treatment of opioid addiction. According to Tillie Fowler, AAPA’s senior vice president for advocacy and government relations,“Although Section 303 of CARA does not include all of AAPA’s policy recommenda- tions; we believe it is a significant step forward in utilizing PAs to expand access to treatment for the millions of Americans who are struggling with opioid addiction. And AAPA will push to extend this authorization for PAs beyond its current 2021 expiration date.” Read more here. INGIMAGE.COM PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 14
- 17. STAT | continued NEW PA JOB SOURCE AAPA recently launched its new“PA JobSource”website, designed to connect employers with PAs across all disciplines and career levels. The PA profession is one of the fastest growing and most in-demand healthcare professions in America and the competition to recruit PAs has been intensifying nationwide. The profession has grown nearly 40 percent in the last five years and, according to the U.S. Bureau of Labor Statistics, employment of PAs is projected to continue to increase 30 percent by 2024. PA PROFESSOR EARNS DISTINGUISHED SERVICE AWARD PA Heidi Miller, Rochester Institute of Technology (RIT) PA program director and professor, was recently rec- ognized with a Distinguished Service Award from the Roch- ester Academy of Medicine during a ceremony to honor her for her service to the community. An active member of the local medical community, Miller and her PA colleagues have forged strong, lasting relationships with healthcare providers in the region to ensure vital clinical rotation sites for RIT PA students. Miller is the inaugural director of the PA program, which she launched in 1993. NEW SYPHILIS SCREENING RECOMMENDATION FOR ADULTS The U.S. Preventive Services Task Force (USPSTF) recently published a final recommendation state- ment and evidence summary on screening for syphilis infection in non-pregnant adults and adolescents. The USPSTF strongly recommends screening individuals at increased risk for syphilis infection. This is an A recommendation. The Task Force’s recommendation has been published in the Journal of the American Medical Association, as well as on the USPSTF website. A fact sheet that explains the final recommendation in plain lan- guage is also available. AAPA is a USPSTF partner. AAPA CREATES NEW LIAISONS TO OSTEOPATHIC PHYSICIANS AND PSYCHIATRISTS The AAPA Board of Directors recently created two new medical liaison positions—to the American Psychiatric Association (APA) and the Ameri- can Osteopathic Association (AOA). The Board appointed PAs Phyllis Peterson of Texas and Melissa Bowlby of Ohio to fill the new positions. AAPA’s medical liaisons are official representa- tives tasked with building and sustaining relation- ships with national physician and medical specialty organizations. Liaisons work to shape PA-positive policies within the broader medical community by providing information as policies are formed and reacting to proposed policies that would be dam- aging for PAs and bad for patients. “In the past couple of years, organized psychiatry has had a growing interest in PAs,”said Jeff Katz, then AAPA president.“Combined with the move- ment to integrate behavioral and primary care, the Board thought it was an opportune time to estab- lish a formal liaison relationship with APA.” “AOA is a major, multispecialty medical organiza- tion that AAPA has previously collaborated with, but we have not had a formal liaison relationship,”Katz added.“In 2013, we issued a joint policy statement supporting team-based medicine and have a strong staff-to-staff relationship. The BOD felt this was the next logical step in building that relationship.” Peterson and Bowlby’s terms run from July 1, 2016–June 30, 2018. With these additions, AAPA now appoints official liaisons to 22 national physi- cian and medical specialty organizations. Read more here. PA Heidi Miller PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 15
- 18. STAT | continued • NEW AAPA CONSTITUENT ORGANIZATIONS Three new constituent organizations (COs) were welcomed to the AAPA fam- ily during the House of Delegates meeting in May. They are the Association of Neurology PAs, Society of PAs in Clinical Ultrasound and PAs in Critical Care. COs are independent organizations affiliated with AAPA that collaborate and combine resources in support of strategic professional goals. They provide their members with an amplified voice for PAs, advocacy leadership, CME and networking opportunities. AAPA’s CO community is comprised of: Chapters: Fifty-six chapters representing 50 states, the District of Columbia and five federal services Specialty organizations: Twenty-seven specialty organizations of individuals working within a specific medical specialty Caucuses: Eight groups of individuals sharing a common concern, interest or goal in healthcare delivery and access Special interest groups: Nineteen groups of individuals that share a common goal or interest EARLY TREATMENT FOR ACUTE KIDNEY INJURY IMPROVES OUTCOMES The initiation of renal replacement therapy less than eight hours after the onset of stage 2 acute kidney injury significantly reduces all-cause mortal- ity at 90 days, according to results from the ELAIN randomized clinical trial, whose findings were published recently in the Journal of the American Medical Association. PAs SEEK INCREASED CAREER FLEXIBILITY AND OPTIONS A new partnership between AAPA’s Center for Healthcare Leadership and Management (CHLM) and CompHealth will provide PAs with job oppor tunities to fit their lifestyles. The 2015 AAPA National Survey found that 38.8 percent, or more than a third, of respondents indi- cated that they chose their current specialty due to“greater flexibility.” “The PA profession is not one-size-fits-all and opportunities for PAs shouldn’t be either,”said AAPA CEO Jennifer L. Dorn. “AAPA and CHLM are commit- ted to creating progressive work environments for PAs, the most in-demand medical profession in the U.S. This alliance with CompHealth will give PAs exclusive access to a special level of career customization.” PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 16
- 19. Online and Print Versions available Cost Effective CME Money Back Guarantee North America’s most widely recognized program for Family Medicine CME and Board Preparation. Visit www.CoreContent.com Call 888-343-CORE (2673) Email mail@CoreContent.com PO Box 30, Bloomfield, CT 06002
- 20. COVER STORY FROM THE SURGICAL SUITE TO AN INTERNATIONAL STAGE PA Houry Gebeshian Headed for Rio Olympics Gebeshian is a PA by night and a gymnast by day. BY HILLEL KUTTLER Every day she works at the Cleveland Clinic, PA Houry Gebeshian welcomes new lives to the world.“It’s an amazing experience to see these squirming babies take their first breath,”she says. Gebeshian is about to accomplish a first herself. In August, she will be competing in the Olym- pic Games in Rio de Janeiro. The first female gym- nast to represent her ancestral land of Armenia in the Games, Gebeshian will do four events: floor PHOTOCOURTESYOFCLEVELANDCLINICVIAHOURYGEBESHIAN PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 18
- 21. COVER STORY, continued exercise, vault, uneven bars and balance beam. The Wall Street Journal named her one of the gymnasts to watch in Rio. Gebeshian, who specializes in obstetric surgery, could even attain immortality in Brazil. That would occur if she executes a new maneuver she’s devised for the uneven bars and has successfully completed in practices. (We’re keeping it under wraps because she’s going to unveil it at the Games.) In keeping with the sport’s tradition, the move would then be named for her: The Gebeshian. Connecting the Dots Gebeshian’s pathways in gymnastics and medicine have touched at several points in her career. Always interested in medicine, she started her career as a certified athletic trainer. She later realized that she wanted to further her education, switching paths to become a PA. That led her to a clinical rotation in Cleveland when she was a second-year PA student at Wake Forest University. Gebeshian arranged a rotation in podiatric surgery at St. Vincent Charity Medical Center’s Spine and Orthopedic Institute. Her preceptor was a podi- atrist and former gymnast, Michael Canales, who she had met years before in Tokyo at the 2011 World Championships when she was making her first attempt to earn a berth at the 2012 Olympic Games in London. She ended up retiring from gymnastics following a calcaneal stress fracture that ended her chances to qualify for the 2012 Games. Canales and his wife Dominique Moceanu—Gebeshian’s childhood idol, former U.S. gymnast, and 1996 Olympic gold medalist—were covering the event for a gymnastics magazine.“I always marvel at how the dots of life are supernaturally connected,”he now says of the chain of events. Gebeshian is a PA in obstetric surgery at Cleveland Clinic. PHOTOCOURTESYOFCLEVELANDCLINICVIAHOURYGEBESHIAN PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 19
- 22. COVER STORY, continued Canales remains impressed with the“rare”skill Gebeshian exhibited during the rotation, when she did histories and physicals for patients and assisted him in surgery. “By the end of the month, she was performing like a first-year resident, an intern,”Canales says.“Within the first week, she’d picked it up; oftentimes, it takes a full year, year and a half, for someone new to the OR to know how to behave. And, she was very humble with our staff, with the OR nurses.” Reigniting Her Dream During her month at the institute in 2013, she met another podiatrist, Duane Ehredt Jr., who was completing his residency training in foot and reconstructive rear foot/ankle surgery under Canales. The two started dating and were later engaged. It was Ehredt who encouraged Gebeshian to give gymnastics another shot. They made a plan, and after graduating from Wake Forest in 2014, Gebe- shian returned to Cleveland. Through the guidance of Canales and Moceanu, Gebeshian started training at Gymnastics World in nearby Broadview Heights, a facility where Canales and Moceanu trained during their gymnastics careers, and where their children now train. With no job lined up, no coach to coach her, and no place to live, Gebe- shian nevertheless followed through with her commitment to Ehredt, and was on her way to make her Olympic dream a reality. Reconnecting with Canales and Moceanu wasn’t the only bit of good fortune to come Gebeshian’s way. When interviewing for a job at Cleveland Clinic, she told PA James Nahrstedt up front that gymnastics was her first priority, but that she’d bust her tail to succeed at work, too. Rather than finding that off-putting, the message impressed Nahrstedt, PA coordinator for Cleveland Clinic’s surgery department. Gebeshian’s up-front statement was“a huge positive, because I was looking for somebody pretty motivated,”he says. It helped, too, that the demanding schedule he quickly had to fill perfectly suited her needs: weekly 24-hour and 16-hour shifts. “I knew she’d be very disciplined. I was impressed,”Nahrstedt says.“When I’m interviewing for employees, I’m thinking: Who can I train to work for me, who will fit in well with the group? It was a positive to have someone dedicated to their routine and what they wanted to accomplish. It was a great fit.” Gymnast by Day, PA by Night Gebeshian stays fit, training up to four days a week, up to 20 hours total. But that’s“very minimal,”she says—far less time than most elite gymnasts devote to training. So, she adds,“I try to be as efficient as possible.” Armenia doesn’t contribute toward her training and transportation expenses. “I’ve done it all on my own,”she says, down to planning workouts on spreadsheets soon after returning home from those long shifts in the OR. Gebeshian did recently receive help from a volunteer gymnastics coach, Levon Karakhanyan, an Armenian-American. A childhood friend, choreographer Nicole Langevin, plotted her floor routine at a discounted rate, and Langevin’s husband, Darek Leiner, condensed three hours of Gebeshian’s preferred music into a 90-second arrangement in dubstep style to accompany her floor routine for Rio. When Gebeshian was a child, she looked up to Langevin, who was a fellow gymnast at the Massachusetts Gymnastics Center (MGC) outside Boston. They reconnected in 2015 as Rio became real. Turns out that Langevin had also admired Gebeshian, who is seven years her junior. PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 20
- 23. COVER STORY, continued “I remember looking over one day and seeing this muscle-bound 10-year-old doing things like a‘double-back’flip that I’d just learned,”says Langevin.“I realized that I should watch her for a few years. I knew she’d do great things.” Gebeshian’s father, Hagop, had an inkling, too. When his daughter was five, he brought her to the local YMCA“to keep her busy,”he says, but was told that she merited more advanced gymnastics instruction. That led them to MGC, where, through age 18, she trained five days a week. Only after she won state championships and earned a Division I athletic scholarship to gymnastics powerhouse the University of Iowa, did her father grasp her Olympic potential. To Armenia With Love Hagop will accompany his daughter on the nearly 5,000-mile trip to Rio from Boston, nearly the distance he covered when he immigrated to Boston from Lebanon many years ago. That’s where he was born, in the Bekaa Valley town of Anjar—an Armenian-majority area settled by refugees from the Turkish genocide against Armenians in 1915. In Anjar, there is a memorial to Musa Dagh, a mountain in southern Turkey where Hagop’s parents, who survived the massacre, had lived. Hagop has told Houry about the family’s roots there and further back in time, in Arme- nia proper, but she’d like to learn more. She’s traveled twice to Armenia, and she joined St. Gregory of Narek Armenian Orthodox Church soon after settling in Cleveland. She’s gotten involved in several social groups in the church, and the Armenian language, once her mother tongue, is slowly returning. But because of those 24-hour Sunday shifts, Gebeshian can’t attend worship services routinely. Fortunately, Ehredt has found a spiritually fulfilling and enthusiastic community at St. Gregory as well. Gebeshian jokingly calls her fiancé an “Armenian by choice”. “He’s helping bring me back to my culture,”she says.“Now, the opportunity to compete for Armenia has brought me back to my roots. In Cleveland, there’s a great Armenian com- munity that’s supportive of what I’m doing.” “I remember looking over one day and seeing this muscle- bound 10-year-old doing things like a ‘double-back’ flip that I’d just learned. I realized that I should watch her for a few years. I knew she’d do great things.” —Nicole Langevin, owner of Precision Choreography, gymnastic coach and former elite gymnast PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 21
- 24. COVER STORY, continued HILLEL KUTTLER is a Baltimore-based freelance writer and editor who has written about PAs and healthcare for many years. He can be reached by email. So, too, is Cleveland Clinic. After qualifying for Rio, Gebeshian was rec- ognized and asked to stand at a meeting, and she was recruited to sign autographs at an Olympic-themed office picnic. Just before she departed for Rio on August 1, the hospital held a cake reception send-off in her honor and will host a watch party during her competition. “To be a PA and an Olympian—that’s kind of cool,”Nahrstedt says of Gebeshian. He adds that some of the qualities she exhibits at work serve her well as an athlete, too.“She’s very task-oriented and pays attention to all the little things. She’s got a very dedicated skill set, and is very good with patients.” He says that“it’ll be extra special”to watch the Olympics on television, knowing that his colleague will be competing. For Moceanu,“with Houry on the radar, I’ll watch to see how she does, because I have a personal rela- tionship with her.” Gebeshian is rightly proud of her accomplishment, acknowledging the obvious in stating,“Not everyone can say they’re an Olympian.” But, like the PA in scrubs who ushers patients into parenthood, the jumping, running, swinging, reaching gymnast plans to cheer on fellow Olympic athletes after her own competitions end. “I’m really looking forward to soaking in the entire experience,”she says. “I want to watch people make their dreams come true.” If you are interested in joining Gebeshian as she embarks on her Olympic journey, follow her on social media via Facebook, YouTube and @HouryGebeshian on Instagram and Twitter. Contact her via email if you’d like to contribute to her GoFundMe campaign. PHOTOCOURTESYOFHOURYGEBESHIAN Gebeshian with children at Woodward Camp for elite athletes. PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 22
- 25. Answering the Call to Provide Care at Olympics BY JENNIFER WALKER PA Judith James sees volunteering to provide emer- gency care to athletes, spectators and staff during the Rio 2016 Olympics and Paralympics as a natural fit for her. She has an international background, having grown up in Seoul, Korea, where her parents worked for the U.S. Army. And she likes the pace and variety of cases that come with emergency medicine, which is why she is a noct- urnist at the East Carolina Heart Institute at Vidant Medi- cal Center in Greenville, N.C. Emergency medical services will be by far the dominant type of care provided during the Olympic Games.The Games are expected to attract an estimated 500,000 tour- ists and 70,000 volunteers from around the world to see 10,500 athletes from the 200 member nations of the Inter- national Olympic Committee (IOC). And the Paralympics is nearly as diverse, hosting athletes from 170 countries. A 2013 graduate of the South College PA program in Knoxville, Tenn., James has had a lifelong interest in sports. So when she saw the IOC Medical and Scientific Commission’s call to become one of a select group of healthcare volunteers, she applied to be among the 5,000 providers who play a key role in one of the world’s big- gest—and oldest—sporting events. After a lengthy appli- cation process, the IOC selected James to be part of the emergency medical services team. “To have the honor of caring for our athletes and to know that I am being allowed to make that kind of contri- bution is just overwhelming,”James says. Also, with 42 sports at the Olympics and 23 at the Paralympics,“the opportunity to maybe take in the Games is pretty excit- ing,”she added. She joins many other PAs who have provided care at other Summer and Winter Olympics, either as members of IOC medical services or for Team USA. In Rio, healthcare volunteers will staff medical stations inside and outside the competition facilities as well as the Olympic Village, which will be home to most of the ath- letes. Selected candidates receive exclusive training for PA Judith James PHOTOCOURTESYOFJUDITHJAMES PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 23
- 26. “To have the honor of caring for our athletes and to know that I am being allowed to make that kind of contribution is just overwhelming.” —PA Judith James the position, and the IOC will provide them with a certificate of participa- tion as well as cover their food and travel costs in Rio on work days. Planning and coordinating medical services for the Games is a daunting undertaking and it starts years before the Olympic torch is lit. Organizers have to consider the day-to-day medical needs of half a million people; plan for large-scale emergencies and disasters, like the bombing that took place at the 1996 Atlanta Olympics; and integrate their medical services with those of the local public health agencies and hospitals, as well as the medical communication and medical transportation systems. “In addition to forming a valuable relations network with professionals from all over the world, the practical lessons learned from close involve- ment in this kind of really complex undertaking represents a unique opportunity for personal and professional growth,”said Adriano Valadão in a press release. Valadão is responsible for recruitment in the IOC’s Rio 2016 Medical Services Department. The application process took at least nine months. First, James filled out an online application. Then, she went through a group online interview with four other potential volunteers. Several weeks later, a physician inter- viewed her by phone, asking her questions about her credentialing and her work, and finally the IOC called her references. About three months after that, she was accepted as a medical services volunteer in November 2015.“I was over the moon that I was selected,”she says. As an Olympic volunteer, James had to take about six online courses that covered such topics as integrity, diversity and the history of the Games. Then, in February, she received her official placement: She will be a Field of Play member, providing emergency medical services at a few ven- ues around the Olympic campus. James wants others to know that exciting opportunities like this do exist for PAs.“If you work hard, if you’re a great provider, and if you place your patients first, the sky’s the limit,”she says. JENNIFER WALKER is a Baltimore-based freelance writer and a regular contributor to PA Professional. She can be reached by email. PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 24
- 27. We get you the perfect job because we get you. A great PA job is only great if it fits your goals, needs, and lifestyle. Our recruiters take the time to develop job searches based on your criteria, ensuring it’s the job that’s just right for you. 866.928.2469 | comphealth.com/pajobs Trusted clinical answers. The latest medical findings. And the best recommendations for your patients. AAPA members, save up to $165 on your subscription – and earn AAPA Category 1 CME credit! Get your discount on this crucial clinical resource today. aapa.org/up2date Make the right decisions at the point of care with UpToDate.
- 28. Learning to Lead PAs Taking Their Place at the Table BY STEVEN LANE, MA, MPP PA HEATHER HYLTON ENCOUNTERED A MAJOR BARRIER in her first weeks on the job as the lead PA for the Department of Medicine at Memorial Sloan Kettering Cancer Center in New York, in 2012. “When I first arrived, PAs were not able to prescribe chemotherapy, which poses a clinical practice issue in a hospital that specializes in the treatment of patients with can- cer,”she said.“There was no reason for this related to the PA practice act for our state; it was a matter that needed to be addressed as we expanded the PA program in our department in order to make care for our patients seamless.”This issue led to the creation of a task force to examine the issue and resulted in the development of a basic and ongo- ing competency standard for PAs and NPs alike who wanted to be credentialed to pre- scribe chemo. “Now there is a standardized process for PAs and NPs in our organization,” she says. PHOTOBYSPENCERSELVIDGE PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 26
- 29. This issue of preparation for leadership is a major component of AAPA’s 2016-2020 Strategic Plan, approved by the Board of Directors in Febru- ary—“Equip PAs for expanded opportunities in healthcare”is one of the plan’s four strategic commitments to the profession. And AAPA has put considerable resources toward addressing this important issue through the launch of the Center for Healthcare Leadership and Management, which was set up to help institutions optimally recruit, utilize and retain their PAs and nurse practitioners (NPs), and to help PAs gain the tools they need to advance into leadership and management positions. PA Professional spoke to a number of PA clinical leaders for their per- spectives on the issues faced by PAs in large institutions and the successes and challenges they have encountered in their roles. (This story is the eighth in PA Professional’s series of strategic plan–related articles; you can read the other seven in the PA Pro archives.) A Place at the Table Most importantly, having a PA in a leadership position in their institution gives PAs an advocate at the highest levels and a voice in the decisions that affect them. “That’s the most important thing—having a voice at the table,”says Amanda Reynado, lead PA at Ben Taub General Hospital, part of the famed Texas Medical Center in Houston.“We are all aware of the need for PA leadership. There needs to be a lead PA for every department to voice con- cerns and represent PAs. Everybody is busy but it’s extremely important that PA practice is not overlooked—which it easily can be.” Advocating for PAs, and educating others about PA practice, is perhaps the biggest part of what PA leaders do every day. The barriers to optimal PA practice typically arise not from any ill will, PA leaders say, but most often simply from ignorance or inertia. “There is just a lack of education—people don’t know what the rules are,”says PA Deb Yolin, a former CHLM adviser who is now an associate medical director at a large Boston health system. Many PA leaders have similar stories to Hylton’s. Often, they were the first occupants of a newly created position and had to blaze a trail for themselves and other PAs. Ron Byerly, PA director for the Geisinger Health System in Pennsylvania, recalls the situation for PAs being“a bit disorganized and chaotic,”when he took up his current role in 2009.“All the PAs were managed by individual departments back then, and departmental managers’knowledge of and interest in PA management and scope of practice varied significantly,”he says. At that point, Geisinger leadership“saw a need to increase the num- bers of its PAs and NPs to fulfill its plans for growth, and realized they needed some people with experience to help guide that growth.”Byerly was one of those people. Learning to Swim A recurring theme among PAs who have taken on leadership and manage- ment roles is a sense of being thrown in to the deep end and having to figure it out as they went along. The role involves many skills that are not PA Heather Hylton PA Amanda Reynado PA Deb Yolin PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 27
- 30. typically taught in PA school, such as scheduling, managing staff, developing policy, working with senior administrators, and staff development. “I have learned so much; a key part of this learning has been collaboration with colleagues both within my organization and across the country, many of whom I have met through AAPA. It’s been tremendous,”says Hylton, now director of PA services for the Department of Medicine at Memorial Sloan Kettering.“As a leader, you need to first learn and embrace an institution’s culture and how it gets work done. This is essential to effectively driving change.” “My first year was very challenging,”agrees PA Cragin Greene, PA fellowship director and lead PA for the Carolinas HealthCare System in Charlotte, N.C.“I was not equipped to be in that role. I had to be manager of up to 60 people; I had never done that before. The biggest challenge was project management, which I had not done in PA school. But I picked it up as I went along.” “Most PA leaders that I know are in the same boat,”adds Rey- nado.“It’s sink or swim. Over the first six months it was a very sharp learning curve. I had to learn hospital policy, hiring, budget, metrics, without a lot of training. I had no MBA or MPH; I had just proven myself as a leader among other PAs.” Enter CHLM It is these issues— helping employers, optimizing PA practice, and helping individual PAs take on leadership roles—that CHLM was established to address. Approved by the AAPA Board in 2015, CHLM has found a strong demand for its services, with the number of engagements increasing four- fold in its second year of operation and its advisers already starting to book up for much of FY2017. Ultimately, PAs and patients alike should benefit from the CHLM’s work. “Not only are we making the lives of PAs and NPs better, but it trickles down to patients,”saysYolin.“It all comes down to patients getting better care. And allowing PAs and NPs to function at the top of their licenses helps them provide better care. And it slows down turnover. If you have a PA who has been at that hospital for 15 years he or she will function very highly.” AAPA's CHLM is changing the way employers see PAs and the way PAs see themselves. PA Ron Byerly PA Cragin Greene PHOTOSCOURTESYOFPASPICTURED PHOTOBYSPENCERSELVIDGE PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 28
- 31. And CHLM can also help an institution’s financial bottom line. “The work we do at CHLM touches on the areas critical to improving access and providing efficient care while maintaining the highest stan- dards of patient safety and quality. Consistently, there are client requests for assistance with recruitment and retention, staffing models and under- standing billing and reimbursement,”says Yolin.“Everyone is being asked to do more with less but we see a lot of wasted resource utilization—work that is duplicated because staffing models have not been evaluated to ensure that each healthcare professional is working to the top of his/her education, competence and licensure.” Working Hand in Hand With the Provider Team CHLM works with both PAs and NPs, and of course with physicians, admin- istrators and hospital staff.“The work we do advising hospitals and systems on ideal provider utilization really supports the team approach,”says Amy Noecker, CHLM managing director.“There is a wide range of workplace environments in which PAs and NPs work and it can even vary between departments at a single hospital. Sometimes a client would like us to focus solely on the PA practice environment, but often we are asked to take a comprehensive look at the entire provider team and how it is operating together.” In many institutions, PAs are combined with NPs in departments with names like the Center for Advanced Practice, and PAs and NPs are often known collectively by such names as“advanced practice providers.”And while this kind of terminology is at odds with the optimal recognition of PAs (and AAPA’s position on nomenclature), it often reflects a reality that PAs and NPs need to work together to improve patient access and quality outcomes. “Whenever you get more than 50 PAs and NPs working together, people want to group us together,”notes PA Todd Pickard, director of PA practice at MD Anderson Cancer Center in Houston and a founding member of PAAMS who was elected to the AAPA Board in May.“It can be very effective to have a single governance structure for PAs and NPs, and it can be empowering to work in collaboration and create recognition for the entire group so that you can effect meaningful change in your system.” “Absolutely we need to work together with NPs,”Greene agrees.“Espe- cially at a large institution. We need to work with NPs, we need to combine forces. NPs have always been good at organizing and we can learn a lot from them.” “I count myself fortunate that my NP counterpart is someone I have known and respected a long time,”says Byerly.“We are much more the same than we are different. Relying on similarities and not arguing about differences can really get you to the point where you can solve problems and provide solutions to leadership.” Moving Into Leadership PA leaders advise PAs who are looking to move into leadership roles to start by seeking out opportunities at their institutions to sit on committees or workgroups. “Don’t be afraid of it,”says Greene.“Your job in school is to learn about medicine and you can’t move up unless you are good clinically so you need to keep doing that. But as your career progresses you need to recog- nize that there are people on the ground creating the way care is delivered. PAs need to be at those tables making decisions. At some point someone will say,‘We are getting a work group together to deal with problem X,’and you have to say yes to those opportunities.” Amy Noecker PA Todd Pickard PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 29
- 32. STEVEN LANE, MA, MPP, is senior strategic writer for AAPA and an editor for PA Professional. Contact him via email or 571-319-4364. Resources for Current and Aspiring PA Clinical Leaders In addition to its advisory services for healthcare institutions, AAPA’s Center for Leadership and Management (CHLM) offers leadership and management training for PAs, both through customized on-site train- ing and national events. Upcoming events include: Executive Leadership Conference November 2-5, 2016 – Winston-Salem, N.C. Annual CHLM Symposium May 18, 2017 – Las Vegas, Nev. To join the AAPA special interest group PA Administrators, Managers and Super- visors and its associated Huddle group, contact Todd Pickard. For PAs in institutions without a PA leadership position, who are trying to develop one, it is important to marshal data effectively, Byerly says. “First and foremost, you have to prove with facts and data that [a PA leadership role] will be beneficial to the hospital and practice. You have to make the case to senior leadership. Have a clear and expert under- standing of your state’s practice act. Show them you can truly step in with expert advice.” State chapters are also a good place to start, Reynado adds.“Do some research and educate yourself on state legislation. Know specifics about practice in your state. State chapters can be very helpful with questions.” PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 30
- 33. Ready for your dream job? Welcome to PA JobSource. Your ultimate PA career resource. The only place to find thousands of PA jobs in every setting and specialty, get your resume reviewed by experts and create customizable job alerts sent straight to your inbox. And it’s all free. Why look anywhere else? Start searching for your dream job today. aapa.org/jobs NEW FROM AAPA!
- 34. Offering Students a Glimpse of the Future 2016 Preceptor of the Year: PA Maureen Barrett BY DAVE ANDREWS B uying a pair of jeans without trying them on—a bit risky. Purchas- ing a car without taking it for a test drive—slightly dangerous. Deciding on a career before experiencing what it has to offer— potentially disastrous. Choosing the right career path is among the most critical decisions in a person’s life, and no one knows this better than PA Maureen Barrett, St. Luke’s University Health Network’s chief surgical PA, and the recipient of AAPA’s 2016 Preceptor of the Year Award. For more than 30 years, Barrett has not only worked hard to advance her own career, but she’s also helped countless students identify their passions and go on to become highly successful, extremely satisfied PAs. “Back when I was an undergrad at King’s [College in Wilkes-Barre, Pa.], I wasn’t exactly sure what I wanted to do, but I always knew it’d be some- thing in healthcare,”Barrett said.“Lucky for me, we had a PA program and it was easy to go speak with administrators to learn more about what it meant to be a PA.” Through those visits, Barrett was inspired by how diverse and instru- mental the role of a PA could be. Now, as part of her role as chair of the PA Maureen Barrett is a preceptor's preceptor. PHOTOCOURTESYOFMAUREENBARRETT PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 32
- 35. PRECEPTOR, continued department of advanced practice at St. Luke’s, she is focused on instilling a similar enthusiasm among the next generation of PAs. St. Luke’s expansive network of hospitals and outpatient facilities is an attractive prospect for college students to shadow PAs, and rotate through all of the major specialties. It became an even more desirable destination once Barrett and a team of her St. Luke’s colleagues revamped the PA Observer Program to create a more refined and comprehensive experience for students looking for a real-world glimpse into the life of a PA. “The impact this program has on these students is tremendous,”she said.“They develop a real sense of purpose and genuine excitement about their future career. With those who choose to go the PA route, we get to see them progress and develop what will surely be a life-long relationship with their career, which is always very special to witness.” Barrett is quick to acknowledge that guiding a program of this nature is not some- thing she can do on her own; it requires a team effort. Throughout all stages of the pro- gram—including application reviews, student orientations and volunteer assign- ments—she works closely with several departments across the St. Luke’s network to ensure the program runs smoothly. This kind of collaboration is key because Barrett is continually juggling numerous administrative demands along with heading up a department. But no matter how chal- lenging her schedule might be, she does all she can to make time for the students. “It’s amazing how vested she is in the [PA] profession and the development of these students,”said Georgina Winfield, director of volunteer services at St. Luke’s.“Whether a student is passionate about healthcare or decides to pursue a different path, Maureen will take the time to give them honest, objective, thoughtful advice.” “Her capacity to be so sincere is a rare characteristic, especially in someone at her level,”Winfield added. Barrett receives her award from then AAPA President-elect Josanne Pagel at AAPA Conference 2016 in San Antonio in May. PHOTOBYSPENCERSELVIDGE PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 33
- 36. Building trust with her colleagues as well as the students is something that comes very naturally to Barrett. In a large system like St. Luke’s, she’s faced various challenges to balance the educational needs of all students. Her ability to build and maintain strong relationships over the years with the St. Luke’s leadership has been critical in helping her maintain the PA student rotations and support program expansion opportunities moving forward. “On my very first day in the [PA Observer] program, I met Maureen and was immediately impressed by how passionate and encouraging she was,” said PA Brie Marks at KidsPeace Children’s Hospital.“I don’t know where she found the time, but she’s someone who, if you put in the effort, she will give that back to you and then some.” Barrett continues to be steadfast in her efforts—throughout the St. Luke’s University Health Network and across the Eastern Pennsylvania region—to advocate on behalf of PAs. She lectures frequently at partner universities, attending symposiums, and participating with the Pennsylva- nia Society of PAs with a determination to keep advancing the profession. “Clinicians and patients alike are beginning to realize when they see a PA, they’re looking at the future of healthcare,”Barrett said.“The PA may very well be their main provider one day. So now is the time for us to culti- vate the skills of that next generation to ensure we always deliver only the highest level of patient care.” PRECEPTOR, continued Barrett helps PA students better identify their medical passions. PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 34 DAVE ANDREWS is a communications and public relations professional specializing in the improvement of healthcare delivery. He is a regular contributor to PA Professional. Contact him by email.
- 37. Whether you’re in the halls of a hospital, the office or the subway, there’s one place you can find CME to keep you clinically current. Explore all Learning Central has to offer – more than 350 activities, including Self- Assessment and Performance Improvement CME (PI- CME) plus JAAPA post-tests. Many activities are free or discounted to members. The Latest Featured CME like Online Orthopaedic CME PANCE/PANRE Prep with trusted resources like AAPA PANCE/PANRE Review PI-CME with AAPA PI Builder Self-Assessment CME with AAPA General Practice Self- Assessment LEARN HERE aapa.org/LearningCentral Learning Central. Connect learning with life.
- 38. PROFESSIONALPRACTICE Common Contract Negotiation Mistakes How to Avoid Them and Advance Your Career B Y J E N N I F E R A N N E H O H M A N C ontract negotiation matters! Here are some pointers on mistakes that are easy to make when in negotia- tions with a new employer. Accepting an Offer Before You’ve Negotiated It This is a common, and understandable error made fre- quently by new graduates. In fairness, navigating the gray area between“You’re Hired!”and“Yes, I’ll take the job!”can be slippery and confusing for more experienced PAs as well. During the interview, inquire as to whether you will be offered a written contract and if there will be an opportunity to review and if necessary negotiate its terms. By clarifying this issue at the outset, you signal that you intend to negoti- ate and reserve the right to give conditional, rather than automatic acceptance of an offer (pending contract negotiation). Not Knowing Your Negotiation Priorities and Alternatives Since negotiation is a dance of requirements and compro- mise on both sides, it’s critically important to know what your priority issues are and which you’d be willing to give ground on. Most PA contracts offer a variety of topics where negotiation can occur. Salary is just one piece of your com- pensation package—other areas for negotiation can include: ■ Start date ■ Vacation and paid holidays ■ Dues and memberships ■ Relocation expenses ■ Sign on bonuses ■ Medical and dental benefits coverage ■ Paid life, disability, or other insurance coverage ■ Retirement plans ■ Location/practice sites ■ Bonuses ■ CME ■ Shares in the practice JENNIFER ANNE HOHMAN is the founder and principal of PA Career Coach, a service dedicated to helping PAs create rewarding, healthy and patient-centered careers. Contact her via email. PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 36
- 39. PROFESSIONAL PRACTICE | continued Not Having a Strategy for Discussing Salary It’s a mistake to go into an interview without a practiced, tactical response to the question of“What are your salary expectations?”Anticipate being put on the spot with this question! When asked, try to defer discussing your salary target by asking what salary range they have determined for the position. It also helps to state that you are interested in the entirety of the compensation package, benefits included, in considering salary. What you’ll need in your back pocket: your salary range goals, based on your research (the AAPA Salary Report being an excellent, in-depth resource) for when it comes time to state what you want. Not Framing Negotiations in Terms of Mutual Benefit It really helps my clients to deal with the stress and contentiousness of negotiating to frame the process as a collaborative one, intended to create a long-lasting employment relationship. Some questions to consider:“How can we create a contract whose clarity and mutual benefit reflect the sort of practice team we want to have?”and“How can we look creatively for solutions to areas where we disagree?”will help you craft a mutually ben- eficial contract and employment relationship (if the employer is interested in doing so; not all are). Key to this process is understanding what the employer wants and needs from the agreement. What are their bottom line requirements and negotiable areas? The fact is, failing to hash out differences now makes them harder to have them resolved once you are hired. Not Knowing Your Deal-Breakers Before the negotiations start, know what would not be acceptable to you in terms of compensation/benefits and common PA contract trouble spots: non-compete clauses, malpractice coverage, restrictions on your ability to volunteer or work for another employer part-time. One of the most valu- able aspects of the negotiation process is the insight it affords you into the values and quality of employer before you’ve committed to working for them. Sometimes even your best efforts to negotiate will fail and it is best to move on. Failing to Document Your Negotiations Getting the details of your negotiations down on paper—on the final, signed draft of the employment agreement—is essential! So often there are discrepancies between what is stated in discussions and what ends up in a contract. The time to fix this is before you’ve started working for a new employer. So many PA’s I’ve spoken to over the years have been told that offer/contract discrepancies would be“taken care of”only to find, a year or more later, that excuses were still being made to avoid reconciling them. Sometimes this becomes the reason a client is looking for a new position. Use your just-hired leverage to avoid this scenario at the outset. I hope these suggestions will help readers to feel more empowered and prepared to establish positive employment terms with employers! If you have any contract negotiation stories or lessons learned you’d like to share, please write me at pacareercoach@gmail.com. PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 37
- 40. REFLECTIONS Walking It Off Lifelong Lessons on the Appalachian Trail B Y D A V I D PA U L K , PA - C , E D D , D FA A PA A little over a year ago, in April of 2015, I was—along with my able colleagues—building a new PA program at Mary Baldwin College in Fishersville, Va. We were writ- ing hundreds of pages of documents for accreditation, attend- ing to thousands of details. And I was drowning. No, more like killing myself, with a regimen of Mountain Dews, Rice Crispy Treats, four hours of sleep a night, and nothing that resembled exercise by any stretch of the word. The awful diet and lack of exercise, coupled with chronic sleep deprivation and over- whelming stress eventually put me in a hospital with chest pain and a healthy fear that this was the big one. Seven years earlier, in 2008, I had suffered a traumatic brain injury secondary to barotrauma off the coast of Mexico, rendering me unable to talk (at least coherently) or walk (at least normally). I could not walk through April of that year, or even say the word,“April.”My mis- use of my body, and lack of sleep, also resulted in a return of some of my earlier brain injury symptoms, including dysfunc- tional balance, slurred words and cognitive dissonance. April has been tough on me at times. I didn’t die (hopefully that’s obvious), but I did receive a wake- up call in the form of an awful pained look on the face of Sarah, my wife. Her look, as I went through the cardiovascular workups, was painfully reminiscent of my recovery from the brain injury as she and my family suffered through my various disabilities, which, unfortunately, included an inability to speak coherently, DAVID PAULK, PA-C, EdD, DFAAPA, is director of the PA program at Mary Baldwin College in Staunton, Va., a well-known speaker on child maltreatment and a keen hiker. PHOTOCOURTESYOFDAVIDPAULK Paulk and his dog, Abe, on the Appalachian Trail PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 38
- 41. REFLECTIONS | continued or even walk without falling down. She looked at me through her lovely green eyes with a resignation that said nothing she could do would save me from my own slow, self-inflicted demise. Did I say wake-up call? No, this was the mother of all wake-up calls. So I started walking. And walking some more. Which led me to hiking, and then hiking some more. I’d love to tell you that this wakeup call was all I needed and that after that my wife, and my life, were extraordinarily happy. But pro- foundly changing a life is tough, to say the least, and frequently, those around you bear the brunt. Yet, she endured—a testament to her infinite patience and love. We live approximately 15 minutes from Shenandoah National Park, which contains more than 500 miles of beautiful trails, including a section of the storied Appalachian Trail. More than 50 pounds melted away as I walked. I felt better. My moods improved. Yet, still, something was missing. Something else needed to be done. I suppose that’s when I got the idea to hike the length of Shenandoah National Park. That’s 107.1 miles (if you believe the maps) between Front Royal and Rockfish Gap, Va. I’m a member of the local National Alliance on Mental Illness (NAMI) board of directors and we decided to use my walk as a fundraiser for much-needed resources for those in our community (click here to donate). It became apparent to me that I needed more than just hiking to train for this, so I enlisted a faculty member’s husband, who I affectionately call“Attila,”due to his remarkable ability to make every high-intensity“core”workout session feel like a call to the cardiac gods to shuffle me off this mortal coil. I decided I would set off the first Saturday in April from Front Royal, and, with my best friend, a 105-pound Chesapeake Bay Retriever,“Abe,”I would reclaim April as we walked south. We set out April 2, Abe carrying a 10-pound pack loaded with his food and water, and me carrying a 62-pound pack (yeah, I know, too much) loaded with dehydrated meals, water, shelter, sleeping bag, clothing, first aid, antibiotics, stove, cookware, bear spray, knives, etc. The first clue that we were not going to have the relatively flat trails I had been training on hit me squarely as we climbed 2,000 feet within the first few miles on rocky, twisting trails. We had walked approximately six miles or so, when the wind picked up to more than 60 mph (67 mph according to a Park Ranger) with wind-chill temperatures near zero. We “I am, for the most part, responsible for the joys and triumphs as well as the sadness and failures in my life, whether in my role as a PA, a PA educator, a husband, a father or a friend. On the trail, your fear and needs manifest in decidedly uncomplicated fashion. Where is water? Where will I sleep? More simply, perhaps, where will I place my foot, how will I climb, and descend the mountain before me?” —PA David Paulk PHOTOCOURTESYOFDAVIDPAULK PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 39
- 42. REFLECTIONS | continued hunkered down after draining the last of our water (I had not yet mastered the art of maintenance drinking), cooked our meal, and collapsed in the tent with the wind sounding like a flock of 747 birds taking off just outside our flimsy shel- ter. Sleep was impossible, as we both shivered and listened to trees, very big trees, drop to the forest floor, seemingly right outside the tent. Dawn revealed snow, and cold, and winds of only around 30-50 mph. The experience of the first night made it imperative, in my mind, that we spend the next night in one of the shelters maintained by the Potomac Appalachian Trail Club. These three-sided structures are placed approximately every 10 miles through the park. My mis- read of the map, however, led us to walk 20.7 miles to Pass Mountain Hut, which, in my exhausted brain, was supposed to be only a 10-mile walk. And only two days had passed. This long second day led me to understand several things: mountains have upsides and downsides—both pose challenges, gazing up too much can crush the spirit and trip the feet, and I’m capable of, well, much. I met some wonderful people on this cold second night, and friends for life were formed. Abe liked them also. They helped me with pack adjustments, I divested myself of weight, and eventually, I got down to around 50 lb. (I know—still too much). We still stay in touch. The abject aloneness of my trek would, at times, cause me to reflect on how I found myself in the middle of nowhere desperately wanting a warm bed and a hot meal. Actually, anything warm would suffice. Several times, I thought to myself, I must have been out of my mind to do this thing. Self-imposed insanity, I thought. I came to understand that the toughest obstacles are those we create, whether through fear, fear of losing control, self-imposed stress, deadlines, issues, concerns, etc. My point? I am, for the most part, responsible for the joys and triumphs as well as the sadness and failures in my life, whether in my role as a PA, a PA educator, a husband, a father or a friend. On the trail, your fear and needs manifest in decidedly uncomplicated fashion. Where is water? Where will I sleep? More simply, perhaps, where will I place my foot, how will I climb, and descend the mountain before me? I learned the toughest trail is the few inches between my ears. The best growth also resides there. I’ve learned: 1. I’m capable of way more than I thought I was. 2. Mental and physical health are vitally important. 3. Liking oneself (even for the first time) is a worthwhile endeavor. 4. The little things don’t matter; the big things rarely do. 5. People matter. Relationships matter. Always have, always will. So, we walked off the trail following 10 hard days, both of us 10-15 pounds lighter. A total trip, including side hikes for water, of 113 miles. Over 14,000 total feet of climbs and descents. Record cold temperatures and extremely high winds. All in the shadows of rocks over 1.2 billion years old; towering, majestic trees; budding flora and fauna; and breathtaking pauses at outcrops and vistas made more so by a soaring hawk or a Peregrine falcon examining you with seemingly uninterested, but oh-so-interested eyes. Beauty only fully appreciated by being a part of it, being within it. And, at the end, as I rested beside the road, lighter and exhausted, Sarah arrived to pick me up. Perhaps she saw a change in me. Not sure, but a smile had replaced the pained resignation in those lovely green eyes. Click to watch video on Paulk's adventures on the AT. PA PROFESSIONAL | AUGUST 2016 | AAPA.ORG | 40
