Ovarian tumors
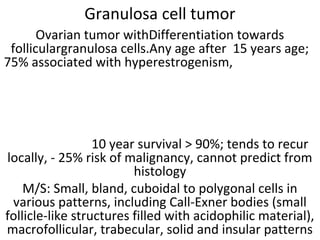
- 1. Granulosa cell tumor Ovarian tumor withDifferentiation towards folliculargranulosa cells.Any age after 15 years age; 75% associated with hyperestrogenism, 10 year survival > 90%; tends to recur locally, - 25% risk of malignancy, cannot predict from histology M/S: Small, bland, cuboidal to polygonal cells in various patterns, including Call-Exner bodies (small follicle-like structures filled with acidophilic material), macrofollicular, trabecular, solid and insular patterns
- 2. Malignant Theca tumor • Malignant thecomas are extremly rare. Thecomas having mitosis more than 4/10 hpf and one ormore of atypia, necrosis, rupture or adhesions is regarded as having malignant potential . In this case, there are sheets of round to spindle cells with ill-defined pale often vacuolated cytoplasm. The nuclei vary from round to spindle shape with moderate atypia and mitotic activity (arrow) is more than 4 per high power field. Hence, it has been classified as a malignant thecoma.
- 3. Benign serous tumors • Includes cystadenoma, cystadenofibroma, adenofibroma, papillary cystadenoma, papillary cystadenofibroma, papillary adenofibroma • The term used depends on the relative amount of fibrous stroma, but distinctions are often arbitrary • Benign; 10-20% bilateral; most are partially or completely cystic; > 1 cm in size (< 1 cm signifies a cortical inclusion cyst or endosalpingiosis)
- 4. Simple serous cyst • Usually small, uni- to multi-locular cysts lined by a single layer of tall, columnar, ciliated cells resembling normal tubal epithelium or cuboidal non-ciliated epithelium resembling ovarian surface epithelium • Stroma contains spindly fibroblasts
- 5. Paillary serous cystadenoma • A case of papillary Serous cystadenoma Ovary showing papillary processes lined by a single layer of tubal type columnar epithelium with cilia and rounded nuclei. The stroma is edematous to fibrous. There is no atypia or mitotic activity.
- 6. Serous cystadenofibroma • Serous Cystadenofibroma ovary showing a lining of a single layer of cuboidal cells with uniform basal nuclei. The stroma is myxoid to fibrous. There is no nuclear atypia or epithelial stratification. Few hypocellular edematous papillary projections can be seen in the lumen.
- 7. adenofibroma • Adenofibroma: entirely solid appearing; if surface papillary projections are prominent, designate as surface papillary serous adenofibroma
- 8. Borderline serous papillary tumor Serous tumors of low malignant potential, characterized by broad, branching papillae (hierarchical branching) focally covered by stratified epithelium with mild to moderate atypia with few mitoses Younger women, often pregnant.10% have microinvasion, but rarely has malignant behavior. Bilateral in 25%.patiets with borderline tumors may have peritoneal implants. Which may be noninvasive and have no influence on prognosis or implants may be invasive which are associated with tumor recurrence or transition to invasive carcinoma. Borderline serous papillary tumor ovary showing branching papillae of multiple lengths with edematous connective tissue cores. The papillae are lined by ciliated columnar epithelium with eosinophilic cytoplasm, round or oval nuclei showing mild to moderate atypia and cellular stratification. Mitotic figures are easily seen. There is no stromal invasion.
- 9. Serous cystadenocarcinoma • Papillary serous carcinoma, Ovary- Low Grade malignant tumors showing irregularly branching papillae without much stroma lined by columnar cells with scant eosinophilic cytoplasm, moderate degree of pleomrphism with round to oval nuclei. Psammoma bodies (concentrically laminated calcified concretions) can be seen. There are two distinct types of ovarian serous carcinoma, low grade and high grade High grade serous carcinoma exhibits moderate to marked nuclear atypia and greater than 12 mitoses per 10 high power fields. Necrosis and multinucleate cells are often present.
- 10. High grade serous adenocarcinoma,ov High grade: Branching papillary fronds, slit-like fenestrations, glandular complexity, moderate to marked nuclear atypia with marked pleomorphism, prominent nucleoli, stratification, frequent mitoses, stromal invasion (irregular or destructive infiltration by small glands or sheets of cells) • Variable psammoma bodies (calcium concretions with concentric laminations, may be intracellular due to autophagocytosis). Stroma may be fibrous, edematous, myxoid, or desmoplastic • A case of High Grade Serous Carcinoma showing marked necrosis. The tumor cells are arranged in microcystic pattern. There is marked nuclear atypia and mitosis (arrow) more than 12 mitoses per 10 high power fields can be seen.
- 11. Benign mucinous tumor Includes cystadenoma, cystadenofibroma and adenofibroma (rare). Lesions are a spectrum of benign lesions with varying amounts of cysts, glands, and stroma - the distinction is arbitrary. 5% bilateral. Associations: carcinoid tumors in same ovary, dermoid cyst, Brenner tumor, endocervical adenocarcinoma; rarely with Zollinger-Ellison syndrome. Gross: Smooth surface with multiple cystic spaces, variable amounts of solid areas. Unilocular cysts are almost always benign. Filled with translucent viscous fluid. M/S: Tall, columnar, nonciliated cells, basal nuclei, abundant intracellular mucin. Usually endocervical type; also intestinal type (picket fence architecture with Paneth cells) or mixed. Stroma may be fibrous or mimic ovarian stroma. May have microscopic rupture of cysts with inflammatory reaction including histocytes and necrosis. Small bland papillae may be present, and mild, focal cytologic atypia may be present
- 12. Borderline Mucinous tumor • Borderline mucinous tumor ovary is also known as atypical proliferative mucinous tumor of ovary or mucinous ovarian tumor of low malignant potential. 85% are intestinal type; 15% are endocervical type. 40-50% tumors are bilateral. • Classification: cllassified into 3 types:1. Borderline with atypia: grade 1 nuclei and papillae with cords. 2. Borderline with intraepithelial carcinoma: grade 2/3 nuclei, 4+ layers or cribriform or stroma-free papillary growth pattern. 3. Borderline with microinvasion: invasive glands usually accompanied by desmoplastic reaction In this case, The atypical epithelium is represented by tall columnar mucus secreting cells forming papillae and infoldings. Focally, Goblet cells (double arrow) are seen indicating intestinal type epithelium. The atypical epithelial lining cells are stratified in two or three layers (arrow) with moderate nuclear atypia. Focal cribriform architecture is seen (circle). Thick clear mucinous material fills the lumen
- 13. Mucinous adenocarcinoma ovary 77% of ovarian mucinous carcinomas are metastases, 23% are ovarian primaries Of the ovarian primaries, most arise in a benign or borderline tumor; only 5-10% are pure Features favoring primary ovarian carcinoma vs. metastasis are: unilateral, "expansile" pattern of invasion, complex papillary pattern, size > 10 cm, smooth external surface, microscopic cystic glands, necrotic luminal debris, mural nodules and accompanying teratoma, adenofibroma, endometriosis or Brenner tumor .Stromal invasion > 10 mm2 distinguishes these tumors from borderline tumors. Two types of invasion - expansile or infiltrative:Expansile tum ors are usually stage I and behave "benign“. Infiltrative tumors may demonstrate malignant behavior and cause death even if stage I Present case--Ovary showing cysts lined with a mixture of goblet cells and tall, columnar intestinal- type epithelium. There is cellular stratification with atypia. The malignant glands (circle) can be seen lying within the fibrous stroma.
- 14. Enddddometroid ca ovary • Endometroid Ovarian Carcinoma constitutes 10- 25% of primary ovarian carcinomas. 15-30% of patients have synchronous endometrial hyperplasia or carcinoma; these tumors are often well differentiated with squamous metaplasia.Stromal invasion is defined as confluent glandular growth, stromal disappearance or obvious stromal invasion. In this case, Crowded, back-to-back glands lined by tall columnar epithelium resembling endometrial epithelium with hyperchromatic nucleus are seen. There is squamous metaplasia (arrow).
- 15. Clear cell adenocarcinoma ovary • Ovarian clear cell adenocarcinomas account for 5% of all ovarian malignancies. Here, neoplastic tumor cells are arranged in nests and glands. Clear cells are typically polyhedral with distinct cell membranes, central to eccentric rounded or slightly angular nuclei, and abundant clear cytoplasm. Hobnail cells can be seen. Stroma is fibrous. Numerous intracytoplasmic hyaline globules (arrow) can be seen. The cytoplasm of clear cells contains abundant glycogen which is Periodic acid-Schiff (PAS) positive, diastase digestion resistant. Microcalcifications are seen in 10-30% of cases
- 16. Primary sq. cell ca ovary Squamous cell carcinoma of ovary can be pure arising denovo or may represent extreme expression of squamous metaplasia in endometriosis, endometrioid carcinomas, transformation of ovarian teratomas and HPV related transformation Pure SCC and those arising from endometriosis are included in surface epithelial tumor by WHO Classification SCC arising in dermoid cyst are included in germ cell tumor by WHO Poor prognosis. The stage of the tumor and its grade correlate best with overall survival Microscopy: Can be well to poorly differentiated Well-differentiated form- SCC will show squamous maturation, keratin formation and intracellular bridging Poorly differentiated form- few normal squamous features may be identifiable. Present case of SCC of ovary did not have any association with endometriotic cyst or mature teratoma.
- 17. Brenner tumor • Benign Brenner Tumor Ovary:Derived from ovarian surface epithelium and metaplasia; similar to Walthard nests, 6% bilateral • Microscopy: Solid and cystic nests of urothelium-like cells surrounded by abundant dense, fibrous stroma • Epithelial cells have sharp outlines. Cells are uniform, polygonal with pale cytoplasm, small but distinct nucleoli, often grooved nuclei (similar to granulosa cell tumors) • Frequent microcysts within epithelial nests • Metaplastic - with prominent cystic formation, accompanied by florid mucinous changes similar to cystitis glandularis • Proliferating - with papillary pattern and low grade nuclear atypia resembling low grade urothelial carcinoma of bladder • Present case shows marked mucinous metaplasia
- 18. Malignant Brenner tumor • Malignant Brenner tumour is a very rare malignancy and closely resembles transitional cell carcinoma of urinary bladder with squamous and undifferentiated variants. Transitional cell carcinoma, however, may • also occur as primary tumor of ovary and only presence or absence of areas with benign or borderline Brenner tumour differentiates the two. In this case, the malignant cells are arranged in nests and sheets, inflitrating and replacing the fibrous stroma. The tumour cells are displaying moderate degree of anaplasia, hyperchromatic nuclei with high mitotic activity. Areas of benign brenner tumor with characteristic coffee bean nuclei are marked with an arrow.
- 19. Transitional cell ca ovary Transitional cell carcinoma (TCC) of ovary is a rare tumor, accounting for only 1% of surface epithelial carcinomas. It has been described as a primary ovarian carcinoma in which definite urothelial features are present but no benign, metaplastic and/or proliferating Brenner tumor can be identified. In this case, broad blunt papillae with fibrovascular cores lined by stratified and highly atypical transitional cells with round or oblong nucleus having prominent nucleoli can be seen. There are punched out microspaces and areas of necrosis. Mitotic activity is high. Some Authors are of view that Ovarian transitional cell carcinoma represents a poorly differentiated form of high-grade serous carcinomas ovary.
- 20. Undifferentiated ca ovary Undifferentiated carcinomas are characterized by a patternless solid, sheet-like growth of tumor cells, with an aggressive clinical course There are no nests, papillae, glands, trabeculae or spindled patterns, no squamous or mucinous metaplasia, and no/minimal neuroendocrine differentiationIf areas of a differentiated component are found, the tumor is . called dedifferentiated carcinoma. Gross : Large tan- brown, fleshy adnexal masses with areas of necrosis, mostly with ovarian surface involvement m/s: Sheets of dyshesive round to ovoid cells, frequently resembling large cell lymphoma, separated by delicate fibrovascular septa No evidence of gland formation, trabecular or nested growth pattern May have foci of spindling / keratinization / necrosis. Vascular invasion in 20%. Frequent mitoses and apoptosis; mitotic rate of 5 to 50 per 10 high power fields
- 21. Krukenberg tumor • Krukenberg tumor is a metastatic signet ring cell adenocarcinoma of the ovary, accounting for 1% to 2% of all ovarian tumors. Stomach is the primary site in most cases (70%). Carcinomas of colon, appendix and breast (mainly invasive lobular carcinoma) are the next most common primary sites. Microscopically, Krukenberg tumor has 2 components: epithelial and stromal.The epithelial component is composed of mucin-laden signet ring cells with eccentric hyperchromatic nuclei. The signet ring cells can be single, clustered, nested, or they can be arranged in tubules, acini, trabeculae, or cords. The intracytoplasmic mucins of the signet ring cells are neutral and acidic, they stain with mucicarmine, PAS and Alcian blue stains. The mesenchymal component of Krukenberg tumor is of ovarian stromal origin and is composed of plump and spindle-shaped cells. In this case, the above mentioned features are seen.
- 22. dysgerminoma Less than 1% of ovarian malignancies. Counterpart of testicular seminoma. Usually young patients <30. 5% associated with gonadal dysgenesis androgen insensitivity or pseudohermaphroditism .Metastasize to opposite ovary, retroperitoneal nodes and peritoneal cavity. Rarely transforms to yolk sac tumor Survival: 95%. Mixture with choriocarcinoma, yolk sac or embryonal carcinoma worsens prognosis. 15% bilateral. Solid, nodular, small to huge and gray-pink (resembles cerebral cortex). Hemorrhage and necrosis common . M/S. Nests of tumor cells separated by fibrous stroma infiltated with T lymphocytes. Large vesicular cells with well defined cell borders, cleared cytoplasm containing glycogen and central nuclei. 1+ prominent nucleoli; occasional granulomas. May have syncytiotrophoblastic cells with raised beta HCG. May have abortive yolk sac elements with increased serum AFP Early carcinomatous differentiation: 30+ mitoses per 10 high power fields, may worsen prognosis
- 23. Yolk sac tumor Yolk sac tumor (also known as endodermal sinus tumor) of the ovary is a malignant germ cell neoplasm. It often occurs in pure form but is also frequently found as a component of mixed malignant germ cell tumors. The most common ("typical") pattern consists of papillary projections, each of which contains a central blood vessel, surrounded by a thick layer of basement membrane material, and then covered by a layer of embryonic epithelial cells with clear or eosinophilic cytoplasm; this structure is referred to as a Schiller-Duval body. Another frequently encountered feature is hyaline globules, which are eosinophilic, PAS-positive, diastase-resistant globules. Histology reveals a wide range of patterns (microcystic, endodermal sinus, solid, alveolar-glandular, papillary, macrocystic, hepatoid, primitive endodermal). In this case, predominantly microcystic pattern is seen. In the lower half, ciliated pseudostratified columnar epithelial lining of dermoid cyst is seen.
- 24. Mature teratoma Tumors arise from a single germ cell after first meiotic division. Mature if only contains adult tissues.If skin tissue predominant, called dermoid cyst. Usually teenage women (solid) or children (cystic). Excellent prognosis, even if peritoneal implants are present. May rupture into peritoneal cavity causing foreign body reaction that simulates metastatic carcinoma or miliary tuberculosis. Cystic tumors may contain squamous cell carcinoma, carcinoid tumor or adenocarcinoma. Gliomatosis peritonei: peritoneal implants exclusively composed of mature glial tissue; benign if all tissue is mature and other teratomatous elements are absent. Gross ; Solid or cystic. Cystic content may contain greasy material composed of keratin, hair and teeth. Micro Description: Ectodermal structures in 100%, mesodermal in 93% and endodermal in 71%. Skin and glial tissue common . Still considered mature if microscopic foci of immature tissue. A case of mature teratoma ovary showing mature, well-differentiated tissue elements from all three embryologic germ layers (ectoderm, mesoderm, endoderm).
- 25. Struma ovarii • Rare monodermal teratoma composed predominantly of mature thyroid tissue. May show pathologic changes of thyroid gland including hyperfunctioning; malignancies are usually papillary thyroid carcinoma. Associated with mucinous cystadenoma, Brenner tumor, carcinoid tumor and dermoid cyst Gross ; Resembles red-brown thyroid tissue but usually multilocular cystic; usually unilateral Micro ; Thyroid follicles with colloid; other teratomatous elements may be present. Rarely has solid or pseudotubular patterns, microfollicles, abundant eosinophilic cytoplasm, abundant clear cytoplasm or minimal thyroid follicles • A case of Struma ovarii showing predominantly mature thyroid tissue consisting of acini of various sizes lined by a single layer of columnar or flattened epithelium. The acini contain eosinophilic, PAS positive colloid.Struma ovarii is a specialized or monodermal teratoma predominantly composed of mature thyroid tissue. Thyroid tissue must comprise more than 50 percent of the overall tissue to be classified as a struma ovarii.
- 26. Sq cell ca in dermoid cyst • Mature cystic teratoma is a common benign adnexal tumour in females. Malignant transformation in a mature cystic teratoma of the ovary is rare, occurring in only 1-2% of cases. The most common malignancy is squamous cell carcinoma, which consists of about 75% of malignant transformations. In this case, squamous cell carcinoma arising from the lining of the cyst on left side of section can be seen. The tumor cells are showing moderate pleomorphism, abundant eosinophilic cytoplasm, roud to oval hyperchromatic nuclei, 0-1 prominent nucleoli. High mitotic activity (arrow), tumor giant cells (double arrow) and keratin pearls (circle) are seen.
- 27. Melanoma arising from dermoid cyst • Malignant melanoma may originate from melanocytes in ovarian cystic teratomas (dermoid cysts). The extremely rare primary ovarian melanoma may be differentiated from the more common melanoma metastatic to the ovaries by its unilaterality, the presence of junctional change,associated with teratoid elements, and a detailed history and physical examination to exclude another primary site. Here, the tumor is seen arising from cyst wall The cells are arranged in nests and are pleomorphic oval to spindled cells with hyperchromatic nuclei, prominent nucleoli, and frequent mitosis. The cytoplasm contained abundant brown pigment, melanin.
- 28. Immature teratoma Immature teratoma represents 3% of all teratomas and 1% of all ovarian cancers. An immature teratoma reveals mixtures of mature and immature tissues reminiscent of the developing stages of embryonic tissues. The most common immature element that is present and used for grading is primitive neuroepithelium. Norris grading system : 1: abundant mature tissue, loose mesenchymal tissue with occasional mitoses, immature cartilage and tooth anlage 2: less mature tissue than grade 1, rare foci of neuroepithelium with mitoses, less than 4 low power fields in any one slide 3: little / no mature tissue; numerous neuroepithelial elements merging with cellular stroma occupying more than low power fields micro images.
- 29. Normal histology of F. Tube • Plica: delicate folds of mucosa on inner aspect of tube, most evident in ampulla, merge with fimbriae • Mucosa: consists predominately of single layer of cells including: 1. Ciliated columnar cells (~25%), most abundant in infundibulum and ampulla, estrogen increases production of cilia. 2. Secretory cells (~60%), non-ciliated, contain apical granules and produce tubular fluid, progesterone increases their number while estrogen increases their height and secretory activity 3. Intercalated cells (peg cells, < 10%), which may be inactive secretory cells Muscle Layer: 3 smooth muscle layers: Innermost - obliquely arranged Middle – circular Outermost - longitudinal, extends into fimbriae Serosal surface: mesothelium of visceral peritoneum. May contain Walthard cell rests
- 30. Normal histology of F. Tube • Walthard cell rests (marked in ellipse); sometimes called Walthard cell nests, are a benign cluster of epithelial cells most commonly found in the connective tissue of the Fallopian tubes, but can also be seen in the mesovarium, mesosalpinx and ovarian hilus. They appear as white/yellow cysts or nodules of flat to cuboidal cells with minimal atypia that can reach a size of 2 millimeters. They typically have elliptical nuclei with a long groove (along the major axis) - so called - "coffee bean" nuclei. May be source of Brenner tumors or primary urethelial cell carcinomas (parafallopian tube transitional cell carcinoma).
- 31. Endometriosis fallopian tube • Presence of endometrial tissue within fallopian tube; will cycle with normal endometrium • Typically seen during reproductive years, in 6-10% of women • Also occurs in 20-50% of tubes after ligation, • May be incidental finding, or associated with abdominal/pelvic pain, infertility • Gross; May have red nodules in wall or serosa, may be actual polyp, may have normal gross appearance • Micro; Endometrial glands, endometrial stroma, hemosiderin-laden macrophages: need 2 to make diagnosis
- 32. Salpingitis isthmica nodosa • Salpingitis isthmica nodosa also called diverticulosis of fallopian tube is characterized by nodular thickening of the tunica muscularis of the isthmic portion of the tube enclosing cystically dilated glands leading to complete obliteration of tubal lumen. It is usually bilateral. May be analogous to uterine adenomyosis. Clinical ; Associated with infertility in 50% . May lead to ectopic pregnancy; Gross – Generally well delineated, yellow-white nodular swelling(s) up to 2 cm, usually isthmus, may be inconspicuous . Microscopy: Regularly spaced glands lined by normal appearing tubal epithelium within hypertrophied smooth muscle or surrounding fibrous tissue Glands may be cystically dilated and are true diverticula that communicate with tubal lumen.. Occasionally glands surrounded by endometrial-type stroma No significant atypia, stromal response minimal In this case, regularly spaced glands lined by normal appearing tubal epithelium within hypertrophied smooth muscle can be seen. Few of the glands are cystically dilated.
- 33. hydrosalpinx • Hydrosalpinx is defined as dilatation of the ampullary segment of the fallopian tube with associated thinning of adherent fimbriae. Causes:- endometriosis, ovulation induction , pelvic inflammatory disease (e.g chlamydial or gonococcal infection): a hydrosalpinx is most commonly a sequela of adhesions from pelvic inflammatory disease, post hysterectomy (without salpingo-oophorectomy). this is from accumulation of tubal secretions caused by surgical blockage proximally and adhesion- related blockage distally, tubal ligation , tubal malignancy: primary or secondary tumours of the fallopian tubes • On microscopy, there is marked dilatation of the lumen, with flattening of mucosa.
- 34. Ectopic tubal pregnancy Implantation of fertilized egg within fallopian tube , Ampulla (80%), isthmus (12%), fimbriae (5%), cornu (2%) Risk Factors: Tubal damage: due to Infections (PID) or salpingitis , Abdominal/pelvic surgery or tubal ligation, History of previous ectopic pregnancy Smoking as smoking may contribute to decreased tubal motility by damaging ciliated cells Altered tubal motility: due to smoking or hormonal contraception; progesterone-only contraception and progesterone intrauterine devices (IUDs) have been associated with increased risk of ectopic pregnancy; symptoms: abdominal or shoulder pain, cramps, vaginal bleeding, nausea, dizziness; Gross ; Distension of tube with thin or ruptured wall, dusky red serosa and hematosalpinx, possibly with fetal parts identified; Micro ; Intraluminal chorionic villi and extravillous trophoblast (may be degenerated); variable fetal parts; Decidual change in lamina propria in 1/3; mesothelial reactive proliferation Uterus: gestational hyperplasia with Arias-Stella reaction ; Present case-- showing thinned and dilated fallopian tube with Intraluminal chorionic villi (arrow), blood and extravillous trophoblast (double arrow)
- 35. Epithelioid trophoblastic tumor,F. Tube• Microscopy: ETT is composed of nests of uniform mononucleate chorionic type intermediate trophoblastic cells, with eosinophilic or clear cytoplasm, round nuclei, and a well-defined cell membrane. Nests of trophoblastic cells are surrounded by extensive necrosis and a hyaline like matrix, resembling keratin, giving ETT its characteristic “geographic” appearance. Within the center of each tumor nest, there is often a small blood vessel, though overall the tumor lacks significant vascular invasion. Immunoperoxidase staining of the trophoblastic cells is positive for pancytokeratin AE1/AE3, p63, EMA, CD10, inhibin alpha, and Ki67.
- 36. Acute salpingitis Acute inflammation of fallopian tube, most commonly due to chlamydia and gonorrhea Symptoms ; abdominal pain, abnormal smell and color of vaginal discharge, bloating, fever, lower back pain, nausea, vomiting , pain during ovulation, dysmanorrhea, dysprinaia, may develop PID oor may be asymptomatic PID has 3 principal complications: chronic pelvic pain (25%), infertility, ectopic pregnancy (15-50%) Impaired fertility is major concern; infection and inflammation can lead to scarring and adhesions within tubal lumens; May lead to tubule-ovarian abscess, pelvic peritonitis, perihepatitis Gross ; Enlarged, erythematous, edematous, Pyosalpinx , hematosalpinx ; May have fibrinous exudate ;Tubo-ovarian abscess common; Micro ; Marked neutrophilic infiltrate, congestion and edema , Mucosal ulceration, Reactive epithelial changes, Variable abscess formation, variable presence of microorganisms
- 37. pyosalpinx Etiology same as for acute salpingitis .Inflammatiion is severe accompanied by suppuration and pus formationn Gross ;tube dilated and filled with pus A case of pyosalpinx showing dilated fallopian tube, thick wall, denudation of epithelium and pus in the lumen and wall.
- 38. Chronic salpingitis • Chronic Salpingitis may follow prolonged acute suppurative salpingitis or result from repeated bouts of acute salpingitis. During acute salpingitis, fibrin exudation into the lumen results in the plicae adhering to each other. Subsequent healing and organization lead to permanent adhesions between the plicae producing follicular salpingitis. Plasma cells, lymphocytes or both are present in the mucosa. . When the inflammation subsides, the tube becomes distended with an acellular transudate producing a hydrosalpinx. The fimbriae may adhere to the ovary leading to direct involvement of the latter and a tubo- ovarian abscess may result. In the present case, numerous plasma cells (arrow), lymphocytes along with few eosinophils are present within plicae of the fallopian tube. Plasma cells must be present before the diagnosis of chronic salpingitis can be made.