53 a focus 8 oxygenation
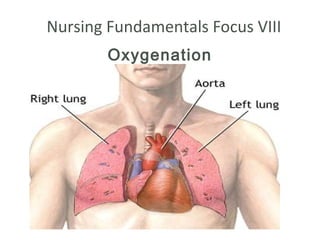
- 1. Nursing Fundamentals Focus VIII Oxygenation
- 2. Objectives • List and discuss the major body structures. • Discuss functions responsible for proper oxygenation • Describe factors that may alter ones O2 balance. • Identify the behaviors indicating negative O2 balance. • Review the common diagnostic tests medically prescribed in order to determine the client’s oxygenation status. • Explain the major purpose of the tests and the related nursing responsibilities.
- 3. Staggering statistics • Pulmonary Diseases • Lung CA - • TB – • Pneumonia – • Chronic Airflow Limitation (formerly COPD) –
- 4. Staggering statistics • Cardiovascular Diseases – # 1 killer • HTN – 65 million • Artheriosclerosis • Arteriosclerosis • Stroke • Hypercholesterolemia • 107 million - a risk factor for CVD • AMI – 7.5 Million per year, 460,000 die • Americans paid 393.5 billion in 2005 for CVD related medical costs
- 6. Process of Breathing •Inspiration • Air flows into lungs •Expiration • Air flows out of lungs
- 7. Normal Oxygenation Process • Cardiovascular:
- 8. Normal Oxygenation Process • Systemic:
- 10. Inspiration • Diaphragm and intercostal muscles contract • Thoracic cavity size increases • Volume of lungs increases • Intrapulmonary pressure decreases • Air rushes into the lungs to equalize pressure
- 11. Expiration • Diaphragm and intercostal muscles relax • Lung volume decreases • Intrapulmonary pressure rises • Air is expelled
- 12. Gas Exchange • Occurs after the alveoli are ventilated • Pressure differences (gradient) on each side of the respiratory membranes affect diffusion • Alveoli: • PO2 100mmHg • PCO2 40mmHg • Venous blood: • PO2 60mmHg • PCO2 45mmHg • O2 diffusion from alveoli pulmonary blood vessels • CO2 diffusion from pulmonary blood vessels alveoli
- 13. Adequate O2 Balance • Maintenance of adequate O2 balance Gas Exchange
- 14. Oxygen Transport • Transported from the lungs to the tissues • 97% of O2 combines with RBC Hgb oxyhemoglobin carried to tissues • Remaining O2 is dissolved and transported in plasma and cells (PO2)
- 15. Normal Oxygenation Process • Cell environment / O2 carrying capacity: • O2 Carrying capacity of blood is expressed by: • Red blood cells (#) • Hematocrit • % of blood that is RBCs • Men 40-54% • Women 37-50% • Hemoglobin
- 18. Carbon Dioxide Transport • Must be transported from tissues lungs • Continually produced in the process of cell metabolism • 65% – carried inside RBCs as bicarbonate (HCO3-) • 30% – combines with Hgb carbhemoglobin • 5% – transported in plasma as carbonic acid (H 2CO3)
- 19. Factors that Influence Respiratory Function • Age • Environment • Lifestyle • Health status • Medications • Stress
- 20. Common Manifestations of Impaired Respiratory Function •Hypoxia •Altered breathing patterns •Obstructed or partially obstructed airway
- 21. Hypoxia • Condition of insufficient oxygen anywhere in the body • Rapid pulse • Rapid, shallow respirations and dyspnea • Increased restlessness or lightheadedness • Flaring of nares • Substernal or intercostal retractions • Cyanosis
- 22. Abnormal Respiratory Patterns • Tachypnea (rapid rate) • Bradypnea (abnormally slow rate) • Apnea (cessation of breathing) • Kussmaul’s breathing • Cheyne-Stokes respirations • Biot’s respirations
- 24. Alterations in Ease of Breathing • Orthopnea • Dyspnea
- 25. Obstructed or Partially Obstructed Airway • Partial obstruction • low-pitched snoring during inhalation • Complete obstruction • extreme inspiratory effort with no chest movement
- 26. Adequate O2 Balance Example of Obstructive Disease: Asthma •
- 27. Adequate O2 Balance Example of Restrictive Disease: Hemothorax •
- 29. Inadequate O2 Balance • Behaviors of Negative O2 balance • Hypoventilation or hyperventilation • Stridor, audible sounds with respiration, wheezing, coughing • Hypoxia • Change in mental status • Change vital signs • Cyanosis • Decrease in GI motility • Change in renal function • Hypercapnia
- 37. Nursing Responsibilities • Determine adequacy of cardiopulmonary function: • Nursing assessment • HEART • Respiratory assessment • PMH • LIFESTYLE
- 38. HEART • Have client describe • specific location, onset and duration of the problem • Explore associated signs and symptoms • Ask - activities that worsen or ease the problem • Rate the severity of discomfort or incapacity • Talk - treatments or interventions used to alleviate the problem and their effectiveness
- 39. Heart Problems Artheroscleosis = Coronary Artery Disease (CAD)
- 40. Nursing Measures to Promote Respiratory Function • Ensure a patent airway • Positioning • Encourage deep breathing, coughing • Ensure adequate hydration
- 41. Nursing Responsibilities • Physical Assessment: • Lung auscultation and breathing pattern • Abdominal assessment • Urine output • Skin and mucous membranes • Heart sounds • Circulation • Edema • DVT
- 42. Lung sounds • Diminished or absent • Crackles course and fine • discontinuous course bubbling • fine crackling sound at the middle or end of inspiration • Rhonchi • a continuous sonorous sound • Wheezes • high pitch musical sounds • Pleural friction rub • grating rubbing, sound
- 43. Common Tests and Nursing Responsibilities •Measure adequacy of ventilation and gas exchange • Complete Blood Count (CBC) phlebotomy • Arterial Blood Gases (ABG) arterial puncture • Pulmonary Function Tests preparation by teaching
- 44. Common Tests and Nursing Responsibilities •Tests to determine abnormal cell growth or infection in respiratory system: • Sputum culture • growing microorganisms from sputum • Throat culture • growth of microorganisms from throat material
- 45. Common Tests and Nursing Responsibilities • Tests to visualize structures of respiratory system: • Bronchoscopy • Chest radiographs
- 47. Common Tests and Nursing Responsibilities Thorancentesis
- 48. Nursing Responsibilities • Medications • Incentive spirometry • Chest PT • Postural drainage • Oxygen therapy • Artificial airways • Airway suctioning • Chest tubes
- 49. Basic Nursing Interventions • Airway Maintenance: • Facilitate effective coughing • Suctioning airways • Liquefying and mobilizing sputum
- 50. Basic Nursing Interventions • Maintenance and promotion of proper lung expansion: Re-expanding collapsed lungs - Closed Chest Tube Drainage
- 51. Chest Tubes
- 52. Basic Nursing Interventions • Improving Activity Tolerance: • Determine etiology • Assess appropriateness of activity level • When appropriate gradually increase activity • Ensure the client changes position slowly • Observe for symptoms of intolerance • Syncope with activity • refer to MD • Perform ROM exercises with activity intolerance if is immobile
- 53. Basic Nursing Interventions • Mobilization of Pulmonary Secretions • Auscultate breath sounds, monitor respiratory patterns, monitor ABG’s • Position client to optimize respiration • Pulmonary toileting • Incentive spirometry • Suctioning
- 56. Basic Nursing Interventions • Mobilization of Pulmonary Secretions • Encourage activity and ambulation as tolerated • Encourage increased fluid intake • Chest physiotherapy • O2 • Medications as ordered
- 57. Basic Nursing Interventions • O2 Therapy: • Low flow • High flow • Humidification • Nasal cannula • Simple mask • Nonrebreathing mask • Partial rebreathing
- 58. Basic Nursing Interventions • Effective Breathing Techniques • Position for maximal respiratory function • Pursed lip breathing • Diaphragmatic or abdominal breathing
- 59. Basic Nursing Interventions Stress and anxiety reduction: • Remove pertinent cause of anxiety at that moment - help client gain control over respiration - reassure client not in immediate danger • Chronic clients • exacerbations and remissions • goal is to reduce general level of anxiety • learn to control episodes of anxiety to improve quality of life • desensitization program • guided mastery
- 60. Administration of Prescribed Medications • Expectorants • Vasoconstrictors • Mucolytics • Bronchodilators • Cough suppressants • Corticosteroids • Antihistamines • Antibiotics
- 61. Basic Nursing Interventions • Physical Exercise health teaching Activity and rest -- a priority ! Activity stimulates respiratory function Rest conserves energy and reduces metabolic demand • MD’s treatment plan • guidelines for activity • may simply call for activity as tolerate. • prioritize activities • arrange need items conveniently • Provide emotional support and encouragement • gradually increase activity • Simplify daily life • Work at a steady state • Conserve energy
- 62. Adequate O2 Balance • Behaviors of Negative O2 balance Cardio Vascular Disease • Arterial • Venous: • Impaired tissue perfusion
- 63. Adequate O2 Balance • Behaviors of Negative O2 balance CV • Restlessness, dizziness, syncope, bradycardia, decreased urine • cold and clammy skin, cyanosis, slow capillary refill • Decreased cardiac output
- 64. Common Tests and Nursing Responsibilities Tests to determine adequacy of cardiovascular • function: • CBC • Lipid profile • Coagulation studies • EKG/ECG • Angiography
- 65. Basic Nursing Interventions Cardiovascular •Diet • Modify risk factors •Exercise •Co morbidities • Preventing vasoconstriction •Positioning •Cold temperatures •Nicotine
- 66. Basic Nursing Interventions • Cardiovascular •Risk DVT •Position changes - Prevent •Early ambulation complications •Obstruction removal •Bypass surgery • Promoting rest •Schedule rest periods •Assistance with ADL’s •Monitor Vitals with activity •Place items, i.e. call light, water pitcher, strategically •Quiet environment, decrease stimuli
- 67. Basic Nursing Interventions - Position semi to high Cardiovascular fowlers-> decrease venous • Positioning to improve return and preload, decease preload-> decreases risk of CO heart congestion - • Avoiding Valsalva • Teach client to avoid valsalva maneuver maneuver - Hold breath while turning or moving in bed-> assist - Bearing down during BM-> stool softeners and diet
- 68. Basic Nursing Interventions Cardiovascular •Avoid appetite suppressants, cold • Avoid stimulants meds, coffee, tea, chocolate • Maintaining fluid balance •Assess fluid status, monitor I&O, assess breath sounds, JVD, pitting edema in dependent areas, fluid and NA+ restriction, daily Wgt with diuretic therapy, electrolyte monitoring-> MD
- 69. Basic Nursing Interventions • Administer O2 Cardiovascular • Educate client • Increase O2 supply NO SMOKING! • Position to facilitate breathing
- 70. Administration of Prescribed Medications • Anti coagulants • Vasodilator Medications • Inotropic Medications • Anti Dysrhythmics • Anti hypertensives
- 71. Basic Nursing Interventions • Dietary control • Assess nutritional status • Consider a dietician referral to assess nutritional needs related to clients • Chronicity of CAL and CAD and nutrition
- 72. Basic Nursing Interventions • Weight control • Evaluate the client’s physiological status in relation to condition • More than body requirements • Less than body requirements
Notas do Editor
- Major body structures: Upper RS: mouth, nose, pharynx, larynx Lower RS: trachea, bronchial tree: primary R/L bronchi, bronchioles, terminal bronchioles, alveolar ducts, alveoli Inspiration: diaphragm & intercostal muscles contract, volume increase, intraplumonary pressure decreases, air in Expiration: diaphragm & intercostal muscles relax, volume decreases, intrapulmonary pressure increases, air expelled Meanwhile, intrapleural pressure maintained negative relative to Patm to create suction to maintain pleura adherence Normal breathing: tidal volume 500 mL Strenuous activity or with some diseases, 1500 mL using accessory muscles Lung compliance: tissue expansibility/stretchability, like a balloon, gets progressively easier decreases with aging: atelectasis risk (collapsed portion of lung) FOR INSPIRATION Lung recoil: continual tendency to collapse away from chest wall FOR EXPIRATION Alveolar fluid has surface tension which makes it alveoli resistant to expansion Surfactant counteracts the surface tension to allow for expansion
- 887 Cellular components develop from mother cells aka stem cells, which subsequently differentiate or specialize into red cells, white cells, and platelets. Red blood cells transport oxygen to tissues in oxyhemoglobin, a molecule that forms when oxygen and hemoglobin combine. White cells fight infection and maintain the body ’s Immune function Platelets aka thrombocytes are essential to coagulation or clotting of blood. Plasma is the fluid component of the blood; it carries the cellular elements, electrolytes, protein, glucose, fats bilirubin, and gases Anemia and carbon monoxide poisoning is a physiological factor that decreases the oxygen carrying capacity of blood Carbon monoxide displaces oxygen from hemoglobin which decrease capacity of blood to carry O2
- 893 Chief complaint Use HEART pneumonic H ave client describe the specific location, onset and duration of the problem E xplore associated signs and symptoms, A sk about activities that worsen or ease the problem, R ate the severity of discomfort or incapacity, T alk about treatments or interventions that were used to alleviate the problem and their effectiveness Ask about difficulty breathing with or without activity, cough, hacking, non productive or productive, if productive what color is sputum, amount, pain with breathing? Respiratory risk assessment age, very young and very old at most risk, environment work or travel hx look at possible exposure, lifestyle -> smoking multiple #packs per day By # of years smoked= pack years, family hx, asthma runs in families, or TB in one family member others may be infected, hx of or resp problems CV Ask about meds. HISTORY of HTN, DM Rheumatic Fever, high cholesterol, bleeding tendencies, MI ,PVD, Heart failure, renal failure, hepatic failure. Examples in book anemia produces a deficit of oxygenation of tissues and DM and renal failure accelerate the development of atherosclerosis. LIFESTYLE: smoking, ETOH, diet exercise stress level, fatty diet
- PE: INSPECT CHEST symmetry and presence of pulsations assess PMI point of maximal intensity. It is located at the 5 th intercostals space at the midclavicular line. Any other pulsations not normal! Vs provide baseline Assess heart sounds , at aortic pulmonic tricuspid and mitral areas at erbs point. Note rate and rhythm 60-110, hear irregularities check apical and radial for differences , listen for gallops, murmurs, or friction rubs. Assess lung sounds, breathing pattern, skin and mucus membranes, check for abd distension and diminished bowel sounds this may be associated with a oxygen deficit because of a decrease in lung expansion. Assess peripheral circulation examine carotid arteries and jugulars in the neck Auscultate for bruits, swish, in the carotid, normally silent. 30-45 degree fowlers examine jugulars—distention of the jugulars sign of heart failure or circulatory overload, check simultaneously on each side brachial radial, femoral, pedal, popliteal palpate for differences on each side, note skin color and temp and texture, note edema by pressing areas of edema and noting depth, and time for indentation to disappear Check for positive homan ’s sign – dorsiflex foot and +pain suggests DVT
- The chest tube is placed between the chest wall and the inner lining of the lung for the purpose of drainage of blood, fluid or air and it could be for many reasons Pneumothorax Post thoracotomy Hemothorax Rib fractures Vascular trauma Post heart surgery most modern acute care facilities now use the disposable, pleural drainage system that combines the suction control, drainage collection and water seal in one unit, such as the Pleur-evac illustrated Area 1 adds suction to provide negative pressure Area 2 water seal chamber it prevents air from entering chest tube Area 3 holds drainage from wound area
- Flow meter volume