Periradicular Diseases
- 1. Presented by R.Senthil Kumar PERIRADICULAR DISEASES
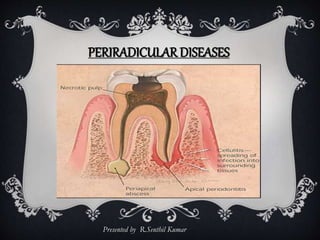
- 2. INTRODUCTION Periradicular diseases are the diseases affecting the Periradicular tissues which comprises of cementum, periodontal ligament & alveolar process. Because of inter-relationship between pulp and Periradicular tissues, pulpal inflammation can cause inflammatory changes in periodontal ligament even before the pulp becomes totally necrotic.
- 3. NORMAL PERIRADICULAR TISSUES Cementum Periodontal ligament Alveolar process
- 4. CEMENTUM Bone like calcified tissue that covers the roots of teeth. Derived from mesenchymal cells of dental follicle that differentiate into cementoblasts. Cementoblasts deposit a matrix – CEMENTOID that is incrementally calcified and produces two types of cementum 1. acellular cementum 2. cellular cementum
- 5. ACELLULAR CEMENTUM CELLULAR CEMENTUM AC cementocytes
- 6. Acellular cementum is deposited first against the dentin forming the cementodentinal junction, it covers the cervical and middle thirds of the root. The cellular cementum is usually deposited on the acellular cementum in the apical third of the root and alternates with layers of acellular cementum. The cellular cementum is deposited at a greater rate thereby entraps cementoblasts in the matrix. These entrapped cells are called CEMENTOCYTES. These cementocytes lie in crypts called lacunae, they communicate to adjacent lacunae through canaliculi, that serve as pathways of nutrients. Because cementum is avascular, its nutrients come from the PDL, as incremental layers of cementum are deposited, the PDL may be further displaced, and some cementocytes may die as a result and may leave empty lacunae.
- 7. Thickness of cementum at CEJ – 20 to 50 micrometer at Apical third – 20 to 150 micrometer Greater thickness at apex is due to continuous deposition of cementum during eruptive life of tooth to preserve its height in the occlusal plane. This continuous deposition also forms the mature apical foramen and an average deviation of the apical foramen of 0.2 to 0.5mm from the center of the root apex. The fibers of periodontal ligament occur between Cementoblasts embedded into the cementum called SHARPEY’s FIBRES.
- 8. FUNCTIONS OF CEMENTUM Preserve height of tooth in the occlusal plane Repair of root fractures & resorption Closing of immature roots by apexification procedure Protective function – more resistant to resorption than bone due to its avascular nature Sealing of accessory and lateral canals after RCT.
- 9. PERIODONTAL LIGAMENT The periodontal ligament is a dense, fibrous connective tissue that occupies the space between the cementum and the alveolar bone. COMPOSITION Fiber bundles Cells Ground substance Interstitial tissue Blood &lymph vessels Nerves
- 10. PRINCIPAL FIBER GROUPS A. Trans-septal group B. Alveolar crest group C. Horizontal group D. Oblique group E. Apical group F. Inter-radicular group Periodontal fibers are the principal structural components of the PDL.
- 11. ACTIVE CELLS OF PERIODONTAL LIGAMENT 1. Fibroblast 2. Cementoblasts 3. Osteoblast 4. Osteoclast 5.Cementoclasts. OTHER CELLS 6. undifferentiated mesenchymal cells 7. epithelial rests of Malassez 8. mast cells 9. macrophages
- 12. FUNCTIONS OF PERIODONTAL LIGAMENT Attach the tooth to its alveolar socket To suspend the tooth in its socket To protect tooth & alveolar socket from masticatory injuries To transform vertical masticatory stresses into tension on the alveolar bone Proprioception – which gives information on movement and position in space. It triggers protective reflex mechanism & localization of areas of inflammation in the periodontal ligament.
- 13. ALVEOLAR PROCESS Alveolar bone proper bundle bone – SHARPEY’s FIBERS are embedded in it lamellated bone Supporting alveolar bone
- 14. ALVEOLAR BONE PROPER The alveolar bone proper is the bone that lines the alveolus or the bony sockets that house the roots of the teeth. Because the peripheral sharpey’s fibers may be calcified, and because lamellae are almost indistinct, this bone is thick and has a more radiopaque appearance in radiographs than cancellous bone or PDL spaces – called LAMINA DURA.
- 15. The alveolar bone proper can also be referred to as CRIBRIFORM PLATE.
- 16. LESIONS OF ENDODONTIC ORIGIN Microbial • Dental caries Trauma • Accidental • Instrumentation • Traumatic occlusion Chemical irritation ETIOLOGY LESIONS OF NONENDODONTIC ORIGIN Periapical cemental dysplasia Cementoblastoma Odontogenic cysts Central giant cell granuloma
- 17. PERIAPICAL CYST
- 18. ACUTE APICAL PERIODONTITIS Incipient exudative and mild symptomatic inflammatory reactions It may be primary or initial if it starts in a healthy periodontium It may be secondary or exacerbating response in a preexisting chronic lesion. This form is also referred to as periapical flare-up, or phoenix abscess or recrudescent abscess.
- 19. Clinical features: intense short lived host response such as • Pain on chewing • Tooth elevated from socket • Tenderness to pressure Radiographic features: widening of periodontal ligament space caused by edema with accumulation of inflammatory exudate in the connective tissue of apical periodontal ligament
- 20. HISTOPATHOLOGY CHANGES Hyperemia, vascular congestion, edema of PDL Extravasation of neutrophils chemotaxis bacterial products(LPS) complement factor C5a repair Radiographical changes: undetectable, since the integrity of hard tissues has not been disturbed If some non infectious but irritating agents have induced inflammation, the lesion may subside and healing occurs.
- 21. IN CASE OF INFECTION Hyperemia, vascular congestion, edema of PDL Extravasation of neutrophils chemotaxis bacterial products(LPS) complement factor C5a Phagocytosis and release of leulotrienes and prostaglandins Osteoclast activation
- 22. When infection is involved, the neutrophils not only kill the microorganisms but also release leukotrienes & prostaglandins. LTB4 attracts more neutrophils and macrophages , and activates osteoclasts and bone resorption occurs. Neutrophils die in great numbers and releases enzymes from their “suicide bags”, causing destruction of extracellular matrices & cells in the “battle zone” preventing the spread of infection and the battle becomes a protracted war. Radiographically periapical widening of periodontal ligament space is detectable now.
- 23. DIAGNOSIS & TREATMENT Pain on percussion is classical diagnostic feature Pulp may be vital or nonvital Radiographic findings Treatment consist of determining the cause and releiving symptoms In case of nonvital tooth, root canal treatment.
- 24. PERIAPICAL ABSCESS The periapical abscess is an acute or chronic suppurative process of periapical region Acute periapical abscess is an advanced exudative and severely symptomatic inflammatory response of the periapical tissues. It is caused by steady increase of inflammatory exudate(edema), leukocyte infiltration, and suppuration.
- 26. CLINICAL FEATURES Tenderness on percussion, extrusion of tooth from socket Tooth might be slightly mobile Swelling of alveolar mucosa Loss of sleep due to pain Slight rise in temperature (99 – 100 degree F) in mild cases Severe cases it may reach (102 – 103 degree F)
- 27. DIAGNOSIS Clinical features Tooth does not respond to EPT , cold test TREATMENT Root canal treatment if swelling is extensive , incision and drainage
- 28. CHRONIC PERIAPICAL ABSCESS Longstanding low-grade inflammatory reaction of periapical connective tissues to pulp irritants Characterized by the formation of parulis (gumboil) and an active pus formation draining through the stoma of a sinus tract. It may be sequela of an acute abscess or may arise from a periapical granuloma. The sinus tract is usually lined with granulomatous tissue but may be lined with stratified squamous epithelium
- 29. HISTOPATHOLOGY Vascular congestion results in regional anoxia and cell breakdown(autolysis). Neutrophils increase in number , releasing their proteolytic ferments to form the pus core. Intensity of pain increases as pus formation adds to periapical pressure and the pus seeks a pathway of least resistance through trabecular spaces.
- 30. Unless drainage is established the exudative inflammatory response may spread diffusely, creating peripheral areas of cellulitis. Incisors – swelling of lip Maxillary canines – ala of nose Maxillary premolars – swelling of eyelid The soft vestibular tissues overlying root end may become inflamed and painful to palpation. The more intense pain occurs as the pus penetrates the outer plate of bone and begin to raise the periosteum. Once the periosteum and mucosa are ruptured, the pain subscides and will not return unless the drainage is blocked.
- 31. DIAGNOSIS Discoloration of tooth Asymptomatic, or mildly painful Presence of sinus tract Tooth does not react to electric or thermal pulp tests Radiograph with Gutta – percha cone into sinus tract TREATMENT : root canal treatment
- 32. PHOENIX ABSCESS Diagnosis is based on the acute symptoms plus radiographic examination, which reveals a large periapical radiolucency. An acute periapical exacerbation that arises from a previously existing chronic lesion as the granulomatous zone becomes infected. This is the painful phase of chronic periapical abscess cycle. When the sinus tract is blocked with coagulum or proliferating epithelium over the stoma, drainage ceases, periapical pressure increases, and the tooth becomes mildly tender to percussion.
- 33. The inflammation may now spread to soft tissues adjacent to the sinus tract stoma. The pressure causes the tissues to baloon outward – parulis develops. Symptoms, when present, are generally mild and of low intensity.
- 34. CHRONIC APICAL PERIODONTITIS Also known as dental or periapical granuloma. Localized mass of granulation tissue formed in periapical region in response to the infection from the root canals. It is the most common of all sequelae of pulpitis or acute apical periodontitis.
- 35. CLINICAL FEATURES The involved tooth is usually nonvital Most of the cases are asymptomatic Slightly tender to percussion and may produce a dull sound The patient may complain about mild pain on chewing of solid food There is usually no perforation of overlying bone and mucosa unless the lesion undergoes an acute exacerbation (phoenix abscess)
- 36. Zones of well established granuloma as described by Dr.W.E.FISH Zone I : zone of necrosis/infection presence of necrotic pulp in root canal results in the diffusion of toxic material into the periapex. (antigens, exotoxins, endotoxins, bacterial enzymes, chemotactic factors) Zone II : zone of contamination or exudative inflammatory zone the toxicity of the root canal irritants is reduced by the fluid and cellular exudative activity in this zone. This reduction in toxicity stimulates osteoclastic resorption of contaminated periapical bone. Radiographic widened apical periodontal space becomes evident now. (liquefaction necrosis, PMNs, macrophages)
- 37. Zone III : zone of irritation or granulomatous zone or proliferative inflammatory zone the gap is opened in bone surrounding the lesion, will ultimately be filled with granulomatous tissue to form this zone. Viable microorganisms are absent. (proliferating fibroblasts, capillary budding, lymphocytes, plasma cells, macrophages, collagen) Zone IV : zone of stimulation or secondary proliferative zone or zone of encapsulation at the periphery of granulomatous zone the toxicity of root canal irritants become so diluted and diminished that the irritants act as a stimulus to fibroblast and osteoblast in that area. A wall of collagen fibers is laid to encapsulate the granulomatous tissue.
- 38. Kronfeld pointed that granuloma is not an environment where bacteria live but one in which they are destroyed . He compared bacteria in root canal (zone I) with an army entrenched “behind high and inaccessible mountains” Apical foramen serving as “mountain passes” The exudative and granulomatous tissue represents a mobilized army defending the “plains”- the periapex from the invaders. If only a few invaders enter the plain through the mountain pass, they are destroyed by defenders (leucocytes) A mass attack of invaders results in a major battle, analogous to acute inflammation (zone II). Once complete elimination of invaders is established, the defending army withdraws, the local destruction created by the battle is repaired (zone III), and the environment returns to its normal pattern. K RONFE L D’ S MOUNTAIN PASS CONCE PT
- 39. GRANULOMATOUS TISSUE Healing function – by the new capillaries and young fibroblasts Defence function – resistance to infection augmented by presence of • Lymphocytes • Plasma cells – antibody synthesis, Russell bodies • Undifferentiated cells – pluripotent cells • Histiocytes – scavengers Foam cells – macrophages ingested fatty material, releases lipid material and needles or crystals of cholesterol are found. Islands of epithelium may be present
- 40. Dunlap and Barker described a condition seen in occasional periapical granulomas and described it as “giant-cell hyalin angiopathy” – a foreign body type reaction. This consist of collection of • Inflammatory cell infiltration • Collection of foreign body type giant cells • Presence of ring like structures known as RHUSTON BODIES, composed of an eosinophilic material resembling hyalinized collagen. There may also be seen fragments of foreign material, sometimes resembling vegetable matter such as legumes, which suggested the use of the term “pulse granuloma”
- 41. RADIOGRAPHIC FEATURES Earliest change is thickening of periodontal ligament at root apex As proliferation continues a radiolucent area is seen attached to the apex with loss of lamina dura The term “periapical rarefying osteitis” is used to describe this appearance of loss of lamina dura and periapical bone. The radiolucency may vary in extent. Greater than 1.5cm in diameter is usually considered to have evolved into a cyst
- 42. The periphery appears as a diffuse blending of radiolucent area with bone – rapidly expanding Thin radiopaque line or zone of sclerotic bone may be seen outlining the lesion – slow progressive one of long standing that has probably not undergone an acute exacerbation Some degree of root resorption is occasionally observed RADIOGRAPHIC FEATURES
- 43. DIAGNOSIS Asymptomatic Radiographic examination Tooth does not respond to thermal or electric pulp tests Patient may give a history of pulpalgia that subsided Exact diagnosis can be made only by histologic examination TREATMENT : Root canal therapy
- 44. PERIAPICAL CYST A periapical cyst is a chronic inflammatory response of the periapex that develops from chronic lesions with pre-existing granulomatous tissue It is characterized by central fluid filled epithelium-lined cavity surrounded by granulomatous tissue and peripheral fibrous encapsulation Generally considered as a direct sequel to chronic apical periodontitis, But not every lesion develops into a cyst. Incidence of cysts among apical periodontitis lesion varies from 6%-55%. Radicular cysts are divided into 2 categories : • Epithelial lining completely enclosing the cavity – True cyst • Epithelial lined cavities that are open to root canals – Bay cyst now it is called as - periapical pocket cyst
- 45. The process of true cyst formation has been discussed as occuring in 3 stages: First phase : the dormant cell rests of malassez are beleived to proliferate, probably under influence of growth factors released by various cells in the lesion. the epithelial cells undergo mitosis and proliferate in all direction simultaneously; thus a ball of epithelial cells is formed. Shear compares this to the MORULA STAGE in the early embryo. the nutrition source is enhanced by the projection of chronically inflamed connective tissue into the ball of cells from all directions. CYST FORMATION
- 46. Second phase : the epithelium lined cavity is formed. nutritional deficiency theory – the central cells of epithelial have inadequate supply of nutrition and consequently undergo necrosis and liquefaction degeneration. intercellular fluid (edema) appears, giving the cells a sponge like characteristics. A definite central cavity develops containing degenerating epithelial cells, infiltrating leukocytes attracted by the necrotic products. the space between the cells increase and soon complete separation of central epithelial cells occurs.
- 47. Abscess theory , postulates that the proliferating epithelium surrounds an abscess formed by tissue necrosis and lysis because of the inherent nature of epithelial cells to cover exposed connective tissue surfaces Third phase : the cyst growth occurs The cyst wall acts as a semipermeable membrane, protein in the dead cells in the cyst cavity increases osmotic pressure, and attracts the fluid from surrounding granulomatous tissue. The cyst grows by attracting fluid into cystic lumen as more and more epithelial cells die and contribute to continued increase in osmotic pressure of the cystic cavity. this growth causes pressure on capillaries in the surrounding connective tissue , producing an ischemia, which favors cell death and the cycle is repeated.
- 48. the fact that the apical pocket cyst grows eliminates osmotic pressure as a potential factor in the development of cyst. Recent attention have shifted in favour of finding a molecular basis for the cystogenesis. Prostaglandins produced by neutrophils in cystic lumen and IL-1-beta produced by T-lymphocytes and macrophages in the extra epithelial areas – can activate osteoclasts , leading to bone resorption. the presence of effector molecules MMP-1 and MMP-2 also have been reported in human periapical cysts.
- 49. Histopathologically, an apical true cyst has four major components 1. Cyst cavity 2. Epithelial wall 3. Extraepithelial tissue 4. Collagenous capsule RADIOGRAPHICALLY – periapical raiolucency ,round or oavl with or without sclerotic boundary will be seen 1 Fluid, necrotic tissue, cholesterol clefts, erythrocytes Stratified squamous epithelium Blood vessels , infiltrating cells
- 50. PERIAPICAL POCKET CYST periapical pocket cyst contain an epithelium – lined, pathologic cavity that is open to the root canal of the affected tooth. Initiated by accumulation of neutrophils around apical foramen, in response to bacteria in the apical root canal. Biologically, a pocket cyst constitutes as an extension of infected root canal space into the periapex. an epithelial collar is formed sealing off the infected root canal and microcystic lumen from the apical milieu and rest of the body
- 51. PERIAPICAL POCKET CYST Microorganisms at the apical foramen attract neutrophilic granulocytes into the microlumen by chemotaxis However , the pouchlike lumen, biologically outside the body milieu, acts as a “death trap” for externalized neutrophils. As the necrotic tissue and microbial products accumulate, the saclike lumen enlarges to accommodate the debris. Periapical pocket cysts have much in common with marginal periodontal pockets and hence the name, rather than a biologically meaningless “bay cyst”
- 52. DIAGNOSIS Radiographic examination Tooth does not respond to thermal or electric pulp tests Previous history of pain Exact diagnosis can be made only by histologic examination TREATMENT : • resolution of the cyst following root canal therapy occurs in 80 – 98% of cases • Surgical treatment if a lesion fails to resorb
- 53. CONDENSING OSTEITIS Productive response of periapical bone to a low – grade longstanding pulpal irritation manifested as an increase in density of periapical bone, due to osteoblastic hyperactivity The bony trabeculae increase in thickness, marrow spaces are eliminated or reduced to small tags of fibrous tissue typically found in young persons around the apices of mandibular teeth with large carious lesions and chronically inflamed pulps.
- 54. RADIOGRAPHIC FEATURES Well – circumscribed radiopaque mass of sclerotic bone surrounding and extending below the apex of one or both roots. Intact lamina dura along entire root length periodontal ligament space widening The border of the lesion may be smooth and distinct or appear to blend into the surrounding bone
- 55. APICAL SCAR Apical scar is not an inflammatory lesion, but rather an uncommon pattern of healing of an apical inflammatory lesion It consist of dense collagenous connective tissue in bone at or near the apex of root with a distinctive radiolucent presentation. It represents a form of healing associated with root that has been treated surgically. Perforation of both facial and lingual osseous cortices is believed to result in collagenous rather than osseous healing. Maxillary lateral incisors are the most frequently affected teeth A thorough history will help in diagnosis
- 56. Periradicular periodontitis – Acute Periradicular periodontitis – Chronic Periradicular periodontitis Periradicular abscess – Acute Periradicular abscess – Chronic Periradicular abscess or Suppurative periradicular periodontitis COHEN GROSSMAN 1. Acute periradicular disease (a) Acute Periradicular periodontitis (symptomatic apical periodontitis) • Vital • Nonvital (b) Acute alveolar abscess (c) Acute exacerbation of chronicApical periodontitis ( phoenix abscess ) 2. Chronic periradicular diseases (a) Chronic apical periodontitis • Chronic alveolar abscess • Cystic apical periodontitis (b) Persistent apical periodontitis 3. Condensing osteitis 4. External root resorption 5. Diseases of periradicular tissues of non- endodontic origin CLASSIFICATIN OF PERIRADICULAR DISEASES
- 59. Normal periapical tissues Symptomatic apical periodontitis Asymptomatic apical periodontitis Acute apical abscess Chronic apical abscess Cellulitis Condensing ostietis Apical scar Ingle’s syndrome – alveolar osteoporosis associated with bruxism INGLE’S CLINICAL CLASSIFICATION
- 60. BIBILOGRAPHY Endodontics – INGLE 5th & 6th edition. GROSSMAN’S endodontic practice – 12th edition Pathways of the pulp – cohen . 9th edition Shafer’s textbook of oral pathology. 5th edition Endodontic therapy – weine. 5th edition Principles N Practice of endodontics WALTON&TORABINEJAD. 3rd edition Oral radiology principles add interpretation – White & Goaz 2nd edition Caranza’s clinical periodontology – tenth edition
