value based healthcare
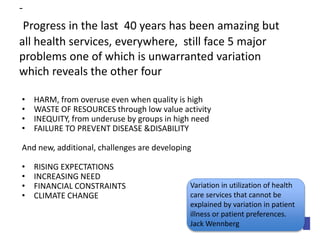
- 1. - Progress in the last 40 years has been amazing but all health services, everywhere, still face 5 major problems one of which is unwarranted variation which reveals the other four • HARM, from overuse even when quality is high • WASTE OF RESOURCES through low value activity • INEQUITY, from underuse by groups in high need • FAILURE TO PREVENT DISEASE &DISABILITY And new, additional, challenges are developing • RISING EXPECTATIONS • INCREASING NEED • FINANCIAL CONSTRAINTS • CLIMATE CHANGE Variation in utilization of health care services that cannot be explained by variation in patient illness or patient preferences. Jack Wennberg
- 2. More of the same is not the answer , not even better quality, safer, greener cheaper of the same run by more tightly regulated and inspected bureaucracies we need to design, plan and build a new paradigm to adapt to the challenge of complexity – “the dynamic state between chaos and order” Kieran Sweeney (2006)
- 5. The Healthcare Archipelago GENERAL MENTAL PRACTICE HEALTH COMMUNITY HOSPITAL SERVICES SERVICES
- 6. JURISDICTIONS INSTITUTIONS PROFESSIONS REGULATORS AND INSPECTORS
- 7. • Is the service for people with seizures & epilepsy better in Adelaide than the service in Melbourne? • Who is responsible for the pelvic pain service for people in North Adelaide? • How many liver disease service s are there in South Australia and how many should there be? • Which service for frail elderly people in Auckland provides the best value? • How many services are there for people with MusculoSkeletal Disease in South Australia, and which gives best value? • Is the variation in outcome for heart failure in the South Australia services increasing or decreasing? • Who is responsible for publishing the Annual Report on care for people with Parkinson’s disease in North Adelaide? • Is the service the people in our population with atrial fibrillation below the minimal acceptable standard of high quality, ie in the top quartile in the middle of the range (a-b) BetterValueHealthcare
- 8. Population healthcare focuses primarily on populations defined by a common need which may be a symptom such as breathlessness, a condition such as arthritis or a common characteristic such as frailty in old age, not on institutions , or specialties or technologies. Its aim is to maximise value and equity for those populations and the individuals within them
- 10. Allocative efficiency Cancer Respiratory Gastro-intestinal Between Programme Marginal Analysis and reallocation is a Board responsibility with public involvement ; the aim is optimal allocation ie you cannot get more value by shifting a single £ from one budget to another
- 11. Cancer Respiratory Gastro-intestinal Between Programme Marginal Analysis and reallocation is a commissioner responsibility with public involvement Mental Health
- 12. Cancers Respiratory Gastro-intestinal Mental Health Many people have more than one problem ; GP’s are skilled in managing complexity
- 13. Medically Unexplained Physical Symptoms Homeless people Children Older People With four or more diagnoses
- 14. Cancers Gastro-instestinal Respiratory Obesity Liver Gastro Intestinal Within Programme, Between System Marginal analysis is a clinician responsibility
- 15. Cancers MSK RA OA/Joints Porosis Respiratory
- 17. Technical Value (Efficiency) = Outcomes / Costs Outcome= Benefit (EBM +Quality) – Harm (Safety ) Costs (Money + time + Carbon)
- 18. Added value from doing things right (quality improvement) Higher Value Higher Value High Value Lower Value Lower Value THE INSTITUTIONAL APPROACH
- 19. After a certain level of investment, health gain may start to decline Benefits Harms Investment of resources Benefits - harm Point of optimality 1. Reduce lower or negative value activities
- 20. Cancers Respiratory Gastro-instestinal Apnoea Asthma COPD (Chronic Obstructive Pulmonary Disease) Triple Drug Therapy O2 Smoking cessation Rehabilitation Within System Marginal Analysis is a clinician responsibility with patient involvement
- 21. Cancers MSK RA OA/Joints Porosis Replacement MRI Arthro /washout Respiratory
- 22. Hellish Decisions in Healthcare All people with the condition People receiving the specialist service People who would benefit most from the specialist service 3. See the right patients
- 23. High Value Innovation + Disinvestment from Lower Value Interventions
- 25. Evidence, Derived from the study of groups of patients The values this patient places on the problem that matter most to them, and on benefits & harms of the options Choice Decision The clinical and social condition of this patient; other diagnoses, risk factors and their genetic profile Personalised and Patient Centred Care
- 26. “By patient values we mean the unique preferences, concerns and expectations each patient brings to a clinical encounter and which must be integrated into clinical decisions if they are to serve the patient.” Source: Straus, S.E., Richardson, W.S., Glasziou, P., Haynes, R.B. Evidence-Based Medicine. (2000) How to practice and teach EBM. (3rd Edition). Elsevier Churchill Livingstone. (p.1).
- 27. After a certain level of investment the health gain may start to decline; the point of optimality Benefits Investment of resources Harms Benefits - harm
- 28. As the rate of intervention in the population increases, the balance of benefit and harm also changes for the individual patient BENEFIT HARM Necessary appropriate inappropriate futile High value Low value Negative Value
- 29. LOW VALUE (BUREAUCRACY BASED CARE) HIGH VALUE (PERSONALISED & POPULATION BASED) Deliver Care through Integrated, Population-based Systems Develop clinical focus on populations Personalise Care & Decision - making DIGITAL KNOWLEDGE Change the Culture to a collaborative culture
- 30. The Healthcare Archipelago GENERAL MENTAL PRACTICE HEALTH COMMUNITY HOSPITAL SERVICES SERVICES
- 31. Chaos…..….Complexity……...Order Person aged 87, 5 diagnoses 8 prescriptions, cared for by Daughter with alcoholic husband Man aged 67 with Dukes A colorectal ca. Man aged 23, Potts# Football woman aged 45 invited for cervical screening Man aged 57 with Psychosis, drug dependence, and severe epilepsy woman aged 73, webuser, with T2 Diabetes, STEMI, high blood pressure, homeopathy woman aged 67 painful hip & mild depression
- 32. Complex Adaptive Systems • “Certain nonlinear systems … are commonly described as being Complex, because their behavior is defined to a large extent by local interactions between their components. When such systems are capable of evolution they are also known as Complex Adaptive Systems.” • Source: Rihani, S (2002) Complex Systems Theory and Development Practice. Understanding non-linear realities. Zed Books Ltd. (p.7).
- 33. SELF CARE INFORMAL CARE GENERALIST SPECIALIST SUPER SPECIALIST
- 34. This is an example of a national service set up as a system
- 37. LOW VALUE (BUREAUCRACY BASED CARE) HIGH VALUE (PERSONALISED & POPULATION HEALTHCARE) Deliver Care through Population-based Systems Develop clinical focus on populations How to achieve high value through Population and Personalised care
- 38. Dr Jones is a respiratory physician in the Derby Hospital Trust and last year she saw 346 people with COPD and provided evidence based, patient centred care, and to improve effectiveness, productivity and safety
- 39. Dr Jones estimated that there are 1000 people with COPD in South Derbyshire and a population based audit showed that there were 100 people who were not referred who would benefit from the knowledge of her team
- 40. Dr Jones is given 1 day a week for Population Respiratory Health and the co-ordinator of the South Derbyshire COPD Network and Service has responsibility, authority and resources for Working with Public Health to reduce smoking Network development Quality of patient information Professional development of generalists, and pharmacists Production of the Annual Report of the service She is keen to improve her performance from being 27th out of the 106 COPD services, and of greater importance, 6th out of the 23 services in the prosperous counties
- 43. • Is the service for people with seizures & epilepsy better in Adelaide than the service in Melbourne? • Who is responsible for the pelvic pain service for people in North Adelaide? • How many liver disease service s are there in South Australia and how many should there be? • Which service for frail elderly people in Auckland provides the best value? • How many services are there for people with MusculoSkeletal Disease in South Australia, and which gives best value? • Is the variation in outcome for heart failure in the South Australia services increasing or decreasing? • Who is responsible for publishing the Annual Report on care for people with Parkinson’s disease in North Adelaide? • Is the service the people in our population with atrial fibrillation below the minimal acceptable standard of high quality, ie in the top quartile in the middle of the range (a-b) BetterValueHealthcare
- 45. OBJECTIVES FOR AN ASTHMA SYSTEM •To prevent asthma •To diagnose asthma quickly and accurately •To slow the process of the disease by effective and safe treatment •To help the individual afflicted adapt to the challenges •To involve patients, both individually and collectively, in their care BetterValueHealthcare
- 46. •To prevent asthma •To diagnose asthma quickly and accurately •To slow the process of the disease by effective and safe treatment •To help the individual afflicted adapt to the challenges •To involve patients, both individually and collectively, in their care •To make the best use of resources •To mitigate inequity •To promote and support research •To support the development of staff •To report annually to the population served BetterValueHealthcare
- 47. LOW VALUE (BUREAUCRACY BASED CARE) HIGH VALUE (PERSONALISED & POPULATION HEALTHCARE) Deliver Care through Population-based Systems Develop clinical focus on populations Personalise care & decision making How to achieve high value through Population and Personalised care
- 48. Evidence, Derived from the study of groups of patients The values this patient places on the problem that matter most to them, and on benefits & harms of the options Choice Decision The clinical and social condition of this patient; other diagnoses, risk factors and their genetic profile Personalised and Patient Centred Care
- 50. LOW VALUE (BUREAUCRACY BASED CARE) HIGH VALUE (PERSONALISED & POPULATION HEALTHCARE) Deliver Care through Population-based Systems Develop clinical focus on populations Personalise care & decision making Change the Culture to a collaborative culture How to achieve high value through Population and Personalised care
- 51. “The culture of a group can now be defined as a pattern of shared basic assumptions that was learned by a group as it solved its problems of external adaptation and internal integration, that has worked well enough to be considered valid and, therefore, to be taught to new members as the correct way to perceive, think, and feel in relation to those problems.” Source: Schein, E.H. (2004) Organizational Culture and Leadership. John Wiley & Sons Inc. (p.17).
- 52. “Leadership …and a company’s culture are inextricably interwined.” Morgan, J.M. and Liker, J.K. (2006) The Toyota Product Development System BetterValueHealthcare
- 53. ASSESSING THE CULTURE • Observe the artifacts • Read the documents • Speak to informants BetterValueHealthcare
- 54. PrimarySecondaryAcuteCommunityManagerOutpatientHubandSpoke Introduce new language A SYSTEM is a set of activities with a common set of objectives and outcomes; and an annual report. Systems can focus on symptoms, conditions or subgroups of the population (delivered as a service the configuration of which may vary from one population to another ) A NETWORK is a set of individuals and organisations that deliver the system’s objectives (a team is a set of individuals or departments within one organisation) A PATHWAY is the route patients usually follow through the network A PROGRAMME is a set of systems with ha common knowledge base and a common budget BetterValueHealthcare Ban old language
- 55. Introduce new language eg MUDA
- 56. LOW VALUE (BUREAUCRACY BASED CARE) HIGH VALUE (PERSONALISED & POPULATION HEALTHCARE) Deliver Care through Population-based Systems Develop clinical focus on populations Personalise care & decision making DIGITAL KNOWLEDGE Change the Culture to a collaborative culture How to achieve high value through Population and Personalised care
- 57. Map of Medicine - COPD Work like an ant colony; Neither markets nor bureaucracies can solve the challenges of complexity BetterValueHealthcare