Acute Myeloid Leukemia(AML).pptx
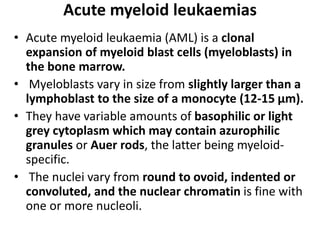
- 1. Acute myeloid leukaemias • Acute myeloid leukaemia (AML) is a clonal expansion of myeloid blast cells (myeloblasts) in the bone marrow. • Myeloblasts vary in size from slightly larger than a lymphoblast to the size of a monocyte (12-15 μm). • They have variable amounts of basophilic or light grey cytoplasm which may contain azurophilic granules or Auer rods, the latter being myeloid- specific. • The nuclei vary from round to ovoid, indented or convoluted, and the nuclear chromatin is fine with one or more nucleoli.
- 3. Acute Myeloid Leukemia(AML) CLINICAL PRESENTATION Symptoms • Increasing fatigue or decreased exercise tolerance (anemia) • Excess bleeding or bleeding from unusual sites (DIC, thrombocytopenia) • Fevers or recurrent infections (neutropenia) • Headache, vision changes, nonfocal neurologic abnormalities (CNS leukemia or bleed) • Early satiety (splenomegaly)
- 4. Physical Examination • Performance status (prognostic factor) • Ecchymosis and oozing from IV sites (DIC, possible acute promyelocytic leukemia) • Fever and tachycardia (signs of infection) • Papilledema, retinal infiltrates, cranial nerve abnormalities (CNS leukemia) • Poor dentition, dental abscesses
- 5. Physical Examination • Gum hypertrophy (leukemic infiltration, most common in monocytic leukemia) • Skin infiltration or nodules (leukemia infiltration, most common in monocytic leukemia) • Lymphadenopathy, splenomegaly, hepatomegaly • Back pain, lower extremity weakness [spinal granulocytic sarcoma, most likely in t(8;21) patients]
- 6. Physical Findings • Fever, splenomegaly, hepatomegaly, lymphadenopathy, sternal tenderness, and evidence of infection and hemorrhage are often found at diagnosis. • Significant GI bleeding, intrapulmonary hemorrhage, or intracranial hemorrhage occurs most often in APL. • Bleeding associated with coagulopathy may also occur in monocytic AML and with extreme degrees of leukocytosis or thrombocytopenia in other morphologic subtypes.
- 7. Physical Findings • Retinal hemorrhages are detected in 15% of patients. • Infiltration of the gingivae, skin, soft tissues, or meninges with leukemic blasts at diagnosis is characteristic of the monocytic subtypes and those with 11q23 chromosomal abnormalities.
- 8. Laboratory and Radiologic Studies • CBC with manual differential cell count • Chemistry tests (electrolytes, creatinine, BUN, calcium, phosphorus, uric acid, hepatic enzymes, bilirubin, LDH, amylase, lipase) • Clotting studies (prothrombin time, partial thromboplastin time, fibrinogen, d-dimer) • Viral serologies (CMV, HSV-1, varicella-zoster) • RBC type and screen
- 9. • HLA typing for potential allogeneic HSCT • Bone marrow aspirate and biopsy (morphology, cytogenetics, flow cytometry, molecular studies for NPM1 and CEBPA mutations and FLT3-ITD) • Cryopreservation of viable leukemia cells • Myocardial function (echocardiogram or MUGA scan) • PA and lateral chest radiograph • Placement of central venous access device
- 10. Interventions for Specific Patients • Dental evaluation (for those with poor dentition) • Lumbar puncture (for those with symptoms of CNS involvement) • Screening spine MRI (for patients with back pain, lower extremity weakness, paresthesias) • Social work referral for patient and family psychosocial support
- 11. Hematologic Findings • Anemia is usually present at diagnosis and can be severe. • The anemia is usually normocytic normochromic. • Decreased erythropoiesis often results in a reduced reticulocyte count, and red blood cell (RBC) survival is decreased by accelerated destruction. • Active blood loss also contributes to the anemia.
- 12. Hematologic Findings • The median presenting leukocyte count is about 15,000/μL. • Between 25 and 40% of patients have counts <5000/μL, and 20% have counts >100,000/μL. • Fewer than 5% have no detectable leukemic cells in the blood. • The morphology of the malignant cell varies in different subsets. • In AML, the cytoplasm often contains primary (nonspecific) granules, and the nucleus shows fine, lacy chromatin with one or more nucleoli characteristic of immature cells. • Abnormal rod-shaped granules called Auer rods are not uniformly present, but when they are, myeloid lineage is virtually certain.
- 13. Hematologic Findings • Poor neutrophil function may be noted functionally by impaired phagocytosis and migration and morphologically by abnormal lobulation and deficient granulation. • Platelet counts <100,000/μL are found at diagnosis in 75% of patients, and about 25% have counts <25,000/μL. • Both morphologic and functional platelet abnormalities can be observed, including large and bizarre shapes with abnormal granulation and inability of platelets to aggregate or adhere normally to one another.
- 14. Pretreatment Evaluation • Once the diagnosis of AML is suspected, a rapid evaluation and initiation of appropriate therapy should follow. • Initial studies should evaluate the overall functional integrity of the major organ systems, including the cardiovascular, pulmonary, hepatic, and renal systems. • Factors that have prognostic significance, either for achieving CR or for predicting the duration of CR, should also be assessed before initiating treatment, including cytogenetics and molecular markers. • Leukemic cells should be obtained from all patients and cryopreserved for future use as new tests and therapeutics become available. • All patients should be evaluated for infection.
- 15. Pretreatment Evaluation • Most patients are anemic and thrombocytopenic at presentation. • Replacement of the appropriate blood components, if necessary, should begin promptly. • About 50% of patients have a mild to moderate elevation of serum uric acid at presentation, while Only 10% have marked elevations, but renal precipitation of uric acid results in the nephropathy, a serious but uncommon complication. • Initiation of chemotherapy may aggravate hyperuricemia, and patients are usually started immediately on allopurinol and hydration at diagnosis.
- 16. Pretreatment Evaluation • Rasburicase (recombinanturic oxidase) is also useful for treating uric acid nephropathy and often can normalize the serum uric acid level within hours with a single dose of treatment. • The presence of high concentrations of lysozyme, a marker for monocytic differentiation, may be etiologic in renal tubular dysfunction, which could worsen other renal problems that arise during the initial phases of therapy.
- 17. TREATMENT of AML • Treatment of the newly diagnosed patient with AML is usually divided into two phases, • Induction and • Postremission management The initial goal is to induce CR. Once CR is obtained, • further therapy must be used to prolong survival and achieve cure. • The initial induction treatment and subsequent postremission therapy are often chosen based on the patient’s age.
- 18. • Intensifying therapy with traditional chemotherapy agents such as cytarabine and anthracyclines in younger patients (<60 years) appears to increase the cure rate of AML. • In older patients, the benefit of intensive therapy is controversial; novel approaches for selecting patients predicted to be responsive to treatment and new therapies are being pursued.
- 19. INDUCTION CHEMOTHERAPY • The most commonly used CR induction regimens (for patients other than those with APL) consist of combination chemotherapy with cytarabine and an anthracycline (e.g., daunorubicin, idarubicin, mitoxantrone). • Cytarabine is a cell cycle S-phase–specific antimetabolite that becomes phosphorylated intracellularly to an active triphosphate form that interferes with DNA synthesis. • Anthracyclines are DNA intercalators. Their primary mode of action is thought to be inhibition of topoisomerase II, leading to DNA breaks.
- 20. INDUCTION CHEMOTHERAPY • In younger adults (age <60 years), cytarabine is used either at standard dose (100–200 mg/m2) administered as a continuous intravenous infusion for 7 days or higher dose (2 g/m2) administered intravenously every 12 h for 6 days. • With standard-dose cytarabine, anthracycline therapy generally consists of daunorubicin (60– 90 mg/m2) or idarubicin (12 mg/m2) intravenously on days 1, 2, and 3. • Other agents can be added (i.e., cladribine) when 60 mg/m2 of daunorubicin is used.
- 21. INDUCTION CHEMOTHERAPY • High-dose cytarabine-based regimens have also been shown to induce high CR rates. • When given in high doses, higher intracellular levels of cytarabine may be achieved, thereby saturating the cytarabine-inactivating enzymes and increasing the intracellular levels of 1-β-d- arabinofuranylcytosine-triphosphate, the active metabolite incorporated into DNA. • Thus, higher doses of cytarabine may increase the inhibition of DNA synthesis and thereby overcome resistance to standard-dose cytarabine. • With high-dose cytarabine, daunorubicin 60 mg/m2 or idarubicin 12 mg/m2 is generally used.
- 22. INDUCTION CHEMOTHERAPY • The hematologic toxicity of high-dose cytarabine- based induction regimens has typically been greater than that associated with 7 and 3 regimens. • Toxicity with high-dose cytarabine also includes pulmonary toxicity and significant and occasionally irreversible cerebellar toxicity.
- 23. • All patients treated with high-dose cytarabine must be closely monitored for cerebellar toxicity. • Full cerebellar testing should be performed before each dose, and further high dose cytarabine should be withheld if evidence of cerebellar toxicity develops. • This toxicity occurs more commonly in patients with renal impairment and in those older than age 60 years. • The increased toxicity observed with high-dose cytarabine has limited the use of this therapy in older AML patients.
- 24. Target Agents • Incorporation of novel and molecular targeting agents into these regimens is currently under investigation. • Trials with tyrosine kinase inhibitors are ongoing. • Patients with CBF AML may benefit from the combination of gemtuzumab ozogamicin, a monoclonal CD33 antibody linked to the cytotoxic agent calicheamicin, with induction and consolidation chemotherapies. • This agent, initially approved for older patients with relapsed disease, has been withdrawn at the request of the U.S. FDA due to concerns about the toxicity, including myelosuppression, infusion toxicity, and venoocclusive disease. • However, the aforementioned recent results are encouraging and support the reintroduction of this agent into the therapeutic armamentarium for AML.
- 25. • In older patients (age ≥60 years), the outcome is generally poor likely due to a higher induction treatment–related mortality rate and frequency of resistant disease, especially in patients with prior hematologic disorders (MDS or myeloproliferative syndromes) or who have received chemotherapy treatment for another malignancy or harbor cytogenetic and genetic abnormalities that adversely impact on clinical outcome.
- 26. • Alternatively, older patients can be also treated with the 7 and 3 regimen with standard-dose cytarabine and idarubicin (12 mg/m2), daunorubicin (45–90 mg/m2), or mitoxantrone (12 mg/ m2). • For patients older than 65 years, higher dose daunorubicin (90 mg/m2) has not shown benefit due to the increased toxicity and is not recommended. • The combination of gemtuzumab ozogamicin with chemotherapy reduces the risk of relapse for patients age 50–70 years with previously untreated AML.
- 27. • Finally, older patients may be considered for single-agent therapies with clofarabine or hypomethylating agents (i.e., 5-azacitidine or decitabine), oftenly used for patients unfit for more intensive therapies • After one cycle of the 7 and 3 chemotherapy induction regimen, if persistence of leukemia is documented, the patient is usually retreated with the same agents (cytarabine and the anthracycline) for 5 and 2 days, respectively.
- 28. POSTREMISSION THERAPY • Induction of a durable first CR is critical to long- term disease free survival in AML. • However, without further therapy, virtually all patients experience relapse. • Thus, postremission therapy is designed to eradicate residual leukemic cells to prevent relapse and prolong survival. • The type of post remission therapy in AML is often based on age and cytogenetic and molecular risk.
- 29. POSTREMISSION THERAPY • For younger patients, most studies include intensive chemotherapy and allogeneic or autologous hematopoietic stem cell transplantation (HSCT). • In the postremission setting, high-dose cytarabine for three to four cycles is more effective than standard- dose cytarabine. • The Cancer and Leukemia Group B (CALGB), for example, compared the duration of CR in patients randomly assigned after remission to four cycles of high (3 g/m2, every 12 h on days 1, 3, and 5), intermediate (400 mg/m2 for 5 days by continuous infusion), or standard (100 mg/m2 per day for 5 days by continuous infusion) doses of cytarabine. • A dose-response effect for cytarabine in patients with AML who were age ≤60 years was demonstrated.
- 30. POSTREMISSION THERAPY • High-dose cytarabine significantly prolonged CR and increased the fraction cured in patients with favorable [t(8;21) and inv(16)] and normal cytogenetics, but it had no significant effect on patients with other abnormal karyotypes. • As discussed, high-dose cytarabine has increased toxicity in older patients. • Therefore, in this age group, for patients without CBF AML, exploration of attenuated chemotherapy regimens has been pursued. • However, because the outcome of older patients is poor, allogeneic HSCT, when feasible, should be strongly considered.
- 31. POSTREMISSION THERAPY Postremission therapy is also a setting for introduction of new agents • Autologous HSCT preceded by one to two cycles of high-dose cytarabine is also an option for intensive consolidation therapy. • Autologous HSCT has been generally applied to AML patients in the context of a clinical trial or when the risk of repetitive intensive chemotherapy represents a higher risk than the autologous HSCT (e.g., in patients with severe platelet alloimmunization) or when other factors including patient age, comorbid conditions, and fertility are considered.
- 32. POSTREMISSION THERAPY • Allogeneic HSCT is used in patients age <70–75 years with a human leukocyte antigen (HLA)- compatible donor who have high risk cytogenetics. • Selected high-risk patients are also considered for alternative donor transplants (e.g., mismatched unrelated, haploidentical related, and unrelated umbilical cord donors). • For older patients, exploration of reduced- intensity allogeneic HSCT has been pursued.
- 33. POSTREMISSION THERAPY • Trials comparing intensive chemotherapy and autologous and allogeneic HSCT have shown improved duration of remission with allogeneic HSCT compared to autologous HSCT or chemotherapy alone. • In fact, relapse following allogeneic HSCT occurs in only a small fraction of patients, but treatment- related toxicity is relatively high; complications include venoocclusive disease, graft-versus-host disease (GVHD), and infections. • Autologous HSCT can be administered in young and older patients and uses the same preparative regimens. • Patients subsequently receive their own stem cells collected while in remission.
- 34. POSTREMISSION THERAPY • The toxicity is relatively low with autologous HSCT (5% mortality rate), but the relapse rate is higher than with allogeneic HSCT, due to the absence of the graft-versus leukemia (GVL) effect seen with allogeneic HSCT and possible contamination of the autologous stem cells with residual tumor cells.
- 35. • Patients with the favorable CBF AML [i.e., t(8;21), inv(16), or t(16;16)] are treated with repetitive doses of high-dose cytarabine, which offers a high frequency of cure without the morbidity of transplant. • Among AML patients with t(8;21) and inv(16), those with KIT mutations, who have a worse prognosis, may be considered for novel investigational studies, including tyrosine kinase inhibitors. • The inclusion of gemtuzumab ozogamicin in induction and consolidation chemotherapy-based treatment has been reported to be beneficial in this subset of patients.
- 36. • For patients in morphologic CR, immunophenotyping to detect minute populations of blasts or sensitive molecular assays (e.g., reverse transcriptase polymerase chain reaction [RT-PCR]) to detect AML-associated molecular abnormalities (e.g., NPM1 mutation, the CBF AML RUNX1/RUNX1T1 and CBFB/MYH11 transcripts, the APL PML/RARA transcript), and the less sensitive metaphase cytogenetics or interphase cytogenetics by fluorescence in situ hybridization (FISH) to detect AML-associated cytogenetic aberrations, can be performed to assess whether clinically meaningful minimal residual disease.
- 37. • Minimal residual disease (MRD) is present at sequential time points during or after treatment. • Detection of MRD may be a reliable discriminator between patients who will continue in CR and those who are destined to experience disease recurrence and therefore require early therapeutic intervention before clinical relapse occurs. • Although assessment of MRD in bone marrow and/or blood during CR is routinely used in the clinic to anticipate clinical relapse and initiate timely salvage treatment for APL patients, for other cytogenetic and molecular subtypes of AML, this is an area of current investigation.
- 38. • Adequate and prompt blood bank support is critical to therapy of AML. • Platelet transfusions should be given as needed to maintain a platelet count ≥10,000/μL. • The platelet count should be kept at higher levels in febrile patients and during episodes of active bleeding or DIC. • Patients with poor post transfusion platelet count increments may benefit from administration of platelets from HLAmatched donors. • RBC transfusions should be administered to keep the hemoglobin level >80 g/L (8 g/dL) in the absence of active bleeding, DIC, or congestive heart failure, which require higher hemoglobin levels.
- 39. • Blood products leukodepleted by filtration should be used to avert or delay alloimmunization as well as febrile reactions. • Blood products should also be irradiated to prevent transfusion-associated GVHD. • Cytomegalovirus (CMV)-negative blood products should be used for CMV-seronegative patients who are potential candidates for allogeneic HSCT. •
- 40. • Neutropenia (neutrophils <500/μL or <1000/μL and predicted to decline to <500/μL over the next 48 h) can be part of the initial presentation and/or a side effect of the chemotherapy treatment in AML patients. • Thus, infectious complications remain the major cause of morbidity and death during induction and postremission chemotherapy for AML. • Antibacterial (i.e., quinolones) and antifungal (i.e., posaconazole) prophylaxis in the absence of fever is likely to be beneficial. • For patients who are herpes simplex virus or varicellazoster seropositive, antiviral prophylaxis should be initiated (e.g., acyclovir, valacyclovir).
- 41. • Fever develops in most patients with AML, but infections are documented in only half of febrile patients. • Early initiation of empirical broad-spectrum antibacterial and antifungal antibiotics has significantly reduced the number of patients dying of infectious complications. • An antibiotic regimen adequate to treat gram- negative organisms should be instituted at the onset of fever in a neutropenic patient after clinical evaluation, including a detailed physical examination with inspection of the indwelling catheter exit site and a perirectal examination, as well as procurement of cultures and radiographs aimed at documenting the source of fever.
- 42. • Acceptable regimens for empiric antibiotic therapy include monotherapy with imipenem-cilastatin, meropenem, piperacillin/ tazobactam, or an extended-spectrum antipseudomonal cephalosporin (cefepime or ceftazidime). • Combination of an aminoglycoside with an antipseudomonal penicillin (e.g., piperacillin) or an aminoglycoside in combination with an extended-spectrum antipseudomonal cephalosporin should be considered in complicated or resistant cases. • Empirical vancomycin should be added in neutropenic patients with catheter-related infections, blood cultures positive for gram-positive bacteria before final identification and susceptibility testing, hypotension or shock or known colonization with penicillin/cephalosporin-resistant pneumococci or methicillin-resistant Staphylococcus aureus..
- 43. • In special situations where decreased susceptibility to vancomycin, vancomycin- resistant organisms, or vancomycin toxicity is documented, other options including linezolid, daptomycin, and quinupristin/ dalfopristin need to be considered.
- 44. • Caspofungin (or a similar echinocandin), voriconazole, or liposomal amphotericin B should be considered for antifungal treatment if fever persists for 4–7 days following initiation of empiric antibiotic therapy. • Amphotericin B, Although liposomal formulations have improved the toxicity profile, its use has been limited to situations with high risk of or documented mold infections. • Caspofungin has been approved for empiric antifungal treatment. • Voriconazole has also been shown to be equivalent in efficacy and less toxic than amphotericin B. • Antibacterial and antifungal should be continued until patients are no longer neutropenic, regardless of whether a specific source has been found for the fever.
- 45. • Recombinant hematopoietic growth factors have been incorporated into clinical trials in AML,to lower the infection rate after chemotherapy. • Both G-CSF and granulocyte-macrophage colony-stimulating factor (GM-CSF) have reduced the median time to neutrophil recovery. • This accelerated rate of neutrophil recovery, however, has not generally translated into significant reductions in infection rates or shortened hospitalizations.
- 46. • In most randomized studies, both G-CSF and GM-CSF have failed to improve the CR rate, disease-free survival, or overall survival. • Although receptors for both G-CSF and GM-CSF are present on AML blasts, therapeutic efficacy is neither enhanced nor inhibited by these agents.
- 47. TREATMENT FOR REFRACTORY OR RELAPSED AML • With the 7 and 3 regimen, 65–75% of younger and 50– 60% of older patients with primary AML achieve CR. • Two-thirds achieve CR after a single course of therapy, and one-third require two courses. • Of patients who do not achieve CR, approximately 50% have a drug resistant leukemia, and 50% do not achieve CR because of fatal complications of bone marrow aplasia or impaired recovery of normal stem cells. • Because these patients are usually not cured even if they achieve second CR with salvage chemotherapy, allogeneic HSCT is a necessary therapeutic step.
- 48. • In patients who relapse after achieving CR, the length of first CR is predictive of response to salvage chemotherapy treatment; patients with longer first CR (>12 months) generally relapse with drug-sensitive disease and have a higher chance of attaining a CR, even with the same chemotherapeutic agents used for first remission induction. • Whether initial CR was achieved with one or two courses of chemotherapy and the type of postremission therapy may also predict achievement of second CR. • Similar to patients with refractory disease, patients with relapsed disease are rarely cured by the salvage chemotherapy treatments. • Therefore, patients who eventually achieve a second CR and are eligible for allogeneic HSCT should be transplanted.
- 49. Target therapy • In addition to kinase inhibitors for FLT3- and KIT- mutated AML, other compounds targeting the aberrant activity of mutant proteins (e.g., IDH2 inhibitors) or biologic mechanisms deregulating epigenetics (e.g., histone deacetylase and DNA methyltransferase inhibitors), • cell proliferation (e.g., farnesyl transferase inhibitors), • protein synthesis (e.g., aminopeptide inhibitors) and • folding (e.g., heat shock protein inhibitors), and ubiquitination, or
- 50. • with novel cytotoxic mechanisms (e.g., clofarabine, sapacitabine), are being tested in clinical trials. • Furthermore, approaches with antibodies targeting commonly expressed leukemia blasts (e.g., CD33) or leukemia initiating cells (e.g., CD123) and immunomodulatory agents (e.g., lenalidomide) are also under investigation.
- 51. TREATMENT OF ACUTE PROMYELOCYTIC LEUKEMIA • APL is a highly curable subtype of AML, and approximately 85% of these patients achieve long-term survival with current approaches. • APL has long been shown to be responsive to cytarabine and daunorubicin, but previously patients treated with these drugs alone frequently died from DIC induced by the release of granule components by the chemotherapy-treated leukemia cells. • However, the prognosis of APL patients has changed dramatically from adverse to favorable with the introduction of tretinoin, an oral drug that induces the differentiation of leukemic cells bearing the t(15;17), where disruption of the RARA gene encoding a retinoid acid receptor occurs.
- 52. Tretinoin • Tretinoin decreases the frequency of DIC but produces another complication called the APL differentiation syndrome. • Occurring within the first 3 weeks of treatment, it is characterized by fever, fluid retention, dyspnea, chest pain, pulmonary infiltrates, pleural and pericardial effusions, and hypoxemia. • The syndrome is related to adhesion of differentiated neoplastic cells to the pulmonary vasculature endothelium. • Glucocorticoids, chemotherapy, and/ or supportive measures can be effective for management of the APL differentiation syndrome. • Temporary discontinuation of tretinoin is necessary in cases of severe APL differentiation syndrome (i.e., patients developing renal failure or requiring admission to the intensive care unit due to respiratory distress). • The mortality rate of this syndrome is about 10%.
- 53. Tretinoin • Tretinoin (45 mg/m2 per day orally until remission is documented) plus concurrent anthracycline-based (i.e., idarubicin or daunorubicin) chemotherapy appears to be among the most effective treatment for APL, leading to CR rates of 90–95%. • The role of cytarabine in APL induction and consolidation is controversial. • The addition of cytarabine, although not demonstrated to increase the CR rate, seemingly decreases the risk for relapse. • Following achievement of CR, patients should receive at least two cycles of anthracycline based chemotherapy.
- 54. • Arsenic trioxide has significant antileukemic activity and is being explored as part of initial treatment in clinical trials of APL. • Patients receiving arsenic trioxide are at risk of APL differentiation syndrome, especially when it is administered during induction or salvage treatment after disease relapse. • In addition, arsenic trioxide may prolong the QT interval, increasing the risk of cardiac arrhythmias.
- 55. • A study compared the gold standard (tretinoin plus chemotherapy) in newly diagnosed non- high-risk APL with a chemotherapy-free combination of tretinoin and arsenic trioxide. • An equivalent outcome was demonstrated between the two arms, and the chemotherapy-free regimen will likely become a new standard for non-high-risk APL patients.
- 56. • Combinations of tretinoin, arsenic trioxide, and/or chemotherapy and/or gemtuzumab ozogamicin have shown favorable responses in high-risk APL patients at diagnosis. • Assessment of residual disease by RT-PCR amplification of the t(15;17) chimeric gene product PML-RARA following the final cycle of chemotherapy is an important step in the management of APL patients. • Disappearance of the signal is associated with long- term disease-free survival; its persistence documented by two consecutive tests performed 2 weeks apart invariably predicts relapse. • Sequential monitoring of RT-PCR for PML-RARA is now considered standard for postremission monitoring of APL, especially in high-risk patients.
- 57. • Patients in molecular, cytogenetic, or clinical relapse should be salvaged with arsenic trioxide with or without tretinoin; it produces meaningful responses in up to 85% of patients and can be followed by autologous or, less frequently, especially if RT-PCR positive for PML- RARA, allogeneic HSCT.
- 58. A. Uniform population of primitive myeloblasts with immature chromatin,nucleoli in some cells, and primary cytoplasmic granules.
- 59. B. Leukemic myeloblast containing an Auer rod.
- 60. C. Promyelocytic leukemia cells with prominent cytoplasmic primary granules.
- 61. D. Peroxidase stain shows dark blue color characteristic of peroxidase in granules in AML.
- 62. Therapy of newly diagnosed acute myeloid leukemia (AML). • For all forms of AML except acute promyelocytic leukemia (APL), standard therapy includes a regimen based on a 7-day continuous infusion of cytarabine (100–200 mg/m2 per day) and a 3-day course of daunorubicin (60–90 mg/m2 per day) with or without additional drugs. Idarubicin (12–13 mg/m2 per day) could be used in place of daunorubicin . • Patients who achieve complete remission (CR) undergo postremission consolidation therapy, including sequential courses of high-dose cytarabine, autologous hematopoietic stem cell transplantation (HSCT), allogeneic HSCT, or novel therapies, based on their predicted risk of relapse (i.e., risk-stratified therapy). • Patients with APL usually receive tretinoin and arsenic trioxide– based regimens with or without anthracycline-based chemotherapy and possibly maintenance with tretinoin.