Presentation1.pptx. ultrasound examination of the ankle joint.
- 1. Ultrasound examination of the ankle joint. Dr/ ABD ALLAH NAZEER. MD.
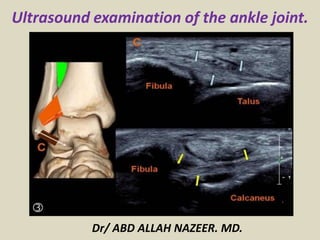
- 2. ULTRASOUND OF THE ANKLE – Normal. Lateral Ankle Peroneus longus and brevis tendons. Calcaneo-fibula ligament. Anterior Talo-Fibula ligament Peroneus tendons scan plane. Peroneus longus and brevis tendons. Transverse at the medial malleolus.
- 3. Scan plane for the Peroneus Brevis insertion to the base of the 5th metatarsal. Peroneus brevis insertion onto the base of the 5th metatarsal.
- 4. Calcaneo fibula ligament scan plane. Calcaneo-fibular ligament.
- 5. ATFL scan plane. Anterior Talo-fibula ligament (ATFL).
- 6. Ultrasound of the Peroneus Longus tendon insertion. The insertion is to the lateral edge of the 1st cuneiform, with some fibers extending to the base of the 1st metatarsal.
- 7. Anterior Ankle Tibio-fibula ligament Extensor Digitorum tendon(s) Extensor Hallucis Longus Tibialis anterior Extensor retinaculum Tibio fibula ligament scan plane. Normal Tibio fibula ligament.
- 8. Scan plane for the extensor digitorum tendon of the foot. Extensor digitorum tendon. There is a common tendon until the level of the extensor retinaculum at the anterior ankle crease. After this, the tendon divides to the 4 lateral toes. (The big toe has it's own tendon - the extensor hallucis).
- 9. Extensor hallucis scan plane Longitudinal extensor hallucis longus tendon.
- 10. Tibialis Anterior scan plane. Longitudinal Tibialis Anterior tendon.
- 11. Medial Ankle Tibialis Posterior tendon Flexor Digitorum tendon Flexor Hallucis Longus tendon Deltoid ligament Posterior tibial nerve Scan plane to see Tibialis Posterior, Flexor Digitorum and Flexor Hallucis Longus (you may need to adjust the probe posteriorly to view the deeper FHL). Tibialis posterior, flexor Digitorum and flexor Hallucis longus tendons (known as "Tom, Dick & Harry"). If including the neurovascular bundle - Tom Dick And Very Nervous Harry.
- 12. Deltoid Ligament scan plane: Use plenty of gel and have the probe tip overlie the malleolar tip. Because of it's obliquity, you cannot readily see all aspects of the ligament.
- 13. Posterior Ankle Achilles tendon Retrocalcaneal (Kager's) fat-pad Scan plane for the Achilles tendon. Normal Achilles tendon longitudinal panorama.
- 26. ULTRASOUND OF THE ANKLE PROTOCOL ROLE OF ULTRASOUND Ultrasound is essentially used for the external structures of the ankle. Ultrasound is a valuable diagnostic tool in assessing the following indications; Muscular, tendinous and ligamentous damage (chronic and acute) Bursitis Joint effusion Vascular pathology Haematomas Soft tissue masses such as ganglia, lipomas Classification of a mass e.g. solid, cystic, mixed Post surgical complications e.g abscess, edema Guidance of injection, aspiration or biopsy Relationship of normal anatomy and pathology to each other Some bony pathology. LIMITATIONS It is recognised that ultrasound cannot adequately assess the deltoid ligament, the ankle mortice and some inter-tarsal ligaments. EQUIPMENT SELECTION AND TECHNIQUE Use of a high resolution, (8-15MHZ)small footprint probe , is essential when assessing the superficial structures of the ankle. Careful scanning technique to avoid anisotropy (and possible misdiagnosis) Beam steering or compounding can help to overcome anisotropy in linear structures such as tendons. Good colour / power / Doppler capabilities when assessing vessels or vascularity of a structure. Be prepared to change frequency output of probe (or probes) to adequately assess both superficial and deeper structures.
- 27. SCANNING TECHNIQUE LATERAL ANKLE Patient sits on the side of a raised bed with foot resting on the Sonographers knee for support. Alternatively, the patient may sit or lie supine on bed with their foot flat. Peroneus longus and brevis tendons: Begin in transverse, posterior to the lateral malleolus. The two tendons are easily seen with the peroneus brevis closest to the bone. Follow them proximally to the muscle and distally with particular attention to the insertion of the peroneus brevis tendon onto the base of the 5th metatarsal. Calcaneo-fibular ligament: With the probe diagonally under the malleolus, angled from the fibula to the heel, you will see the peroneus tendons in transverse and the calcaneo-fibula ligament underlying them. ANTERIOR ANKLE Patient positioned as above. Anterior talo-fibula ligament (ATFL): Place the heel of the probe on the anterior aspect of the distal fibula and rotate the toe of the probe towards the 2nd toe. The ligament should be readily visible as a 2cm long, 3mm thick tight fibrillar structure. Tibio-Fibula ligament (TFL): From the ATAF, further rotate the toe of the probe until just above the horizontal. The TFL has a similar appearance to the ATAF. Extensor tendons: In transverse across the anterior ankle crease, you will see, from lateral to medial, the extensor digitorum, extensor hallucis and tibialis anterior tendons. By independently mobilizing each of the toes and watching the tendons glide, you can identify which is which and exclude tendon rupture The overlying extensor retinaculum should also be observed.
- 28. MEDIAL ANKLE Patient positioned as above. Tibialis posterior, flexor digitorum and flexor hallucis longus tendons: Assess the tendons along their length in longitudinal and transverse. Pay particular attention to the insertion of the Tibialis Posterior tendon with caution not to mistake the often present accessory ossicle, for an avulsed fragment. Begin diagonally under the medial malleolus with the toe of the probe on the malleolus. You will see the tibialis posterior and flexor digitorum tendons in transverse. Slide the probe postero-inferiorly and you will see the flexor hallucis longus tendon deeper against the calcaneum. The deltoid ligament: Is poorly assessed with ultrasound. Posterior tibial nerve: The neurovascular bundle is easily seen posterior to the medial malleolus POSTERIOR ANKLE Patient positioned prone with the feet off the end of the bed. Achilles tendon: Perform a survey scan ,in transverse, from the calcaneum up to the musculo-tendinous junction (of both medial and lateral gastrocnemii). Rotate into longitudinal and examine for thickening and integrity. At the same time assess the retrocalcaneal (Kager's) fat pad. The calf muscles and plantaris tendon should also be assessed as clinically indicated.
- 29. An ankle series should include the following minimum images; Peroneus tendons - long, trans + peroneus brevis insertion Calcaneo-fibular ligament Anterior talo-fibula ligament Tibio-Fibula ligament Extensor digitorum tendon Extensor hallucis longus tendon Tibialis anterior tendon Tibialis posterior tendon Flexor digitorum tendon Flexor hallucis longus Achilles tendon and retro calcaneal bursa Document the normal anatomy. Any pathology found in 2 planes(ligament tears or thickening, synovial bulging/cysts, joint effusion, gross bony changes), including measurements and any vascularity.
- 30. MAIN INDICATIONS OFTHE ANKLE ULTRASONOGRAPHIC STUDY Tendon pathology of the different compartments of the ankle. • Evaluation of ligament injuries. • Bone and joint disorders (synovitis, chondral and osteochondral lesions, occult fractures) • Retroachilles and preachilles bursitis. • Characterization of tumors (accessory muscles, ganglia, neurogenic tumours, soft tissue abscesses, etc.) • Localization of foreign bodies. ABNORMALITIES OF TENDONS Tendon injuries include tenosynovitis, tendinosis, rupture and instability.
- 31. POSTERIOR COMPARTMENT ACHILLES TENDINOPATHY Can be classified as tendinosis and paratendinitis. The isolated paratendinitis shows intratendinous normal structure, exist paratendinitis spill, shown irregularities in the edges of the tendon, adhesions and scarring associated paratendon and a heterogeneous aspect preachilles fat pad. In the tendinosis there is in swelling of the tendon, usually bilateral, and textural heterogeneity intratendinous focal hypoechoic areas. TEAR OF ACHILLES The rupture site is located generally between the 2 and 6 cm from the insertion into the calcaneous, in the called critical zone of relative hypovascularity. In ultrasound, complete rupture of the Achilles tendon is seen as a focal defect between the broken ends of the tendon. In the acute phase ends are contiguous, but the defect may be filled by the anechoic or hypoechoic hematoma. In most cases paratendon remains intact as a envelope straight echogenic contouring breakage. As a sign associated can exist distortion of the fibrillar configuration and loss of parallelism of the tendon fibers. Other signs are indicative fat herniation into the defect, better visualization of the plantar tendon and the existence of a posterior acoustic shadowing at the site of the tear (useful sign to differentiate partial thickness tears).
- 32. Complete rupture of the Achilles tendon with focal defect between the ends of the tendon and posterior acoustic shadowing at the site of the tear, useful sign to differentiate partial thickness tears.
- 33. Patient with psoriasis which identifies tendinosis and Achilles tendon swelling bilateral and textural heterogeneity with intratendinous focal hypoechoic areas.
- 34. Ultrasound and radiological correlation calcified Achilles enthesitis. Calcaneal spur as associated finding.
- 35. Discreetly thickened right Achilles tendon at its insertion, combining linear hyperechoic and hypoechoic areas on small breaks intrasubstance and calcifications of the enthesis.
- 36. Fat herniation into the defect by complete tear of the Achilles tendon.
- 37. Complete tear of the Achilles tendon with retraction of ends and integrity thin plantaris tendon.
- 38. Tendinosis versus partial tear of Achilles tendon.
- 39. •PREACHILLES AND RETROACHILLES BURSITIS Although bursitis can occur in isolation, often are related and systemic inflammatory diseases. In the ultrasound examination the distended retrocalcaneal and preachilles appears are a hypoechoic structure shaped coma, interposed between the Achilles tendon and the posterosuperior aspect of the calcaneous. Care must be taken not to confuse it with the fatty space Kager containing oval lobules of hyperechoic fat. When bursitis is a manifestation of synovitis is appreciated hypervascular area with Doppler ultrasound. In the retroachilles bursitis exists thickening and collection of fluid in the subcutaneous tissue superficial to the tendon retrocalcaneal portion.
- 40. Bursitis preachilles with typical morphology, appreciating accumulation of fluid in a "coma" between the anterior portion of the Achilles tendon and the calcaneous.
- 41. Bursitis preachílea that associated synovitis, showing hyperemia with increased Doppler flow.
- 42. Rheumatoid arthritis with retrocalcaneal bursitis (*1) and calcaneal erosions (*2)
- 43. ACCESSORY NAVICULAR BONE In the distal insertion site may exist TP 2 types of bones accessories: Accessory navicular bone type I (os tibiale externum): size between the 2 and 6 mm, can be contained within the TP and being positioned immediately proximal posteromedial to the navicular bone. It generally produces symptoms and should not be confused with a tendon calcification or avulsion fracture. Type II accessory navicular bone: is an accessory ossification centre of the navicular bone with size between 9 and 12 mm triangular shaped and articulated through a synchondrosis of the posterior and medial navicular bone. It insertion site of some fibers of TP and is associated with a syndrome of pain and increased incidence of tendon rupture caused by abnormal overloads. Osteoarthritic changes may underlie this synchondrosis which mimic tendon pathology.
- 44. Accessory navicular bone within the posterior tibial tendon, as anatomical variant.
- 45. ANTERIOR COMPARTMENT The tendons of the anterior ankle, compared with the rest of the ankle tendons are rarely affected by disease. The anterior tibial tendon is the most prone to abnormalities, like tendinopathy, tenosynovitis and its place between the most frequent rupture is extensor retinaculum and insertion into the first cuneiform and the base of the first metatarsal. Sometimes the retracted tendon stump causes a nodule on the anteromedial aspect of the distal portion of the leg, making clinically confused with a tumour or cyst.
- 46. Distal insertion tendinopathy of the anterior tibial tendon with increased vascularity
- 47. Tenosynovitis of the anterior tibial tendon with effusion.
- 48. Anterior tibial tendon tenosynovitis with intratendinous ruptures.
- 49. Anterior tibial tendon rupture with retraction of the tendon.
- 50. Tenosynovitis of the extensor digitorum tendons with a synovial effusion.
- 51. Tenosynovitis of the extensor digitorum tendon with hypervascularized thickened tendon and synovium and synovial fluid.
- 52. Rheumatoid arthritis with tenosynovitis of the extensor digitorum and peroneal tendons.
- 53. Thickening of the extensor hallucis longus tendon caused by osteosynthesis material.
- 54. Multicystic non vascularized intramuscular mass in the extensor digitorum brevis muscle.
- 55. LATERAL COMPARTMENT TENOSYNOVITIS OF THE PERONEAL TENDONS The main sign of ultrasound is the presence of liquid inside the common synovial sheath, whereas usually tendinous morphology is preserved We must differentiate tenosynovitis of a spill within the common peroneal sheath secondary to a tear of calcaneofibular ligament (PCL). The ultrasound diagnosis is the detection of the tendons in a lateral plane relative to the distal portion of the lateral malleolus, instead of behind it. The dynamic exploration foot dorsiflexion as both eversion may help identify cases of intermittent subluxation. In long-standing disease can be observed fusiform thickening of the peroneal tendons at the tip of the malleolus. The complete tears of the peroneus brevis tendon (PC) and peroneus longus (PL) are rare, occurring in the area of the lateral malleolus or midfoot. Seen in patients with ankle sprains or history of chronic instability, especially if they suffer widespread diseases (RA, DM,) or treated with corticosteroids. The peroneal tendon ruptures causing the inability to eversion of the foot and cavus foot varus.
- 56. Important thickening of both peroneal tendons (longus and brevis) associated with moderate amount of fluid and thickening of the synovial sheath.
- 57. Discreet amount of fluid in the common sheath of the peroneal tendons associated with disorganization and a heterogeneous appearance peroneus brevis tendon related to longitudinal rupture.
- 58. Peroneal tenosynovitis and osteosynthesis
- 59. Tenosynovitis of the peroneal tendons and an intratendinous rupture of the short peroneal tendon.
- 60. Intratendinous rupture and cyst in the peroneus brevis tendon.
- 61. Peroneus quartus with an accessory muscle next to the peroneus longus and brevis tendons.
- 62. Tumor next to the peroneal tendons that proved to be a benign fibrous mass.
- 63. MEDIAL COMPARTMENT ANOMALIES POSTERIOR TIBIAL TENDON (TP) It is the most frequently injured in this compartment, with ruptures in asymptomatic middle-aged obese women as a result of widespread disease (RA, seronegative Spondyloarthropathy) or associated with bone fractures. It causes a gradual collapse of the medial longitudinal arch with hindfoot valgus deformity and excessive forefoot pronation. The presence of small vessels in inflammatory diseases intratendinosis can simulate a fissuration tendon, confusion can be ignored using colour Doppler. Another possible diagnostic difficulty is when the undamaged tendon flexor digitorum longus (FLD) moves back and simulates the TP unbroken, but it is smaller and in this case we only see in the groove retromalleolar 1 only tendon. Ultrasound has also proven to be an effective resource for identifying alterations associated tendon tenosynovitis serosa and hypertrophic. Subluxation and dislocation anteriorly and medial TP relative to internal malleolus is rare and valued sonographically placing the foot in dorsiflexion with forced supination.
- 64. Thickening, moderate amount of fluid surrounding, calcifications and hyperemia affecting the sheath and the posterior tibial tendon related to chronic tenosynovitis in patient affects rheumatoid arthritis.
- 65. Thickening, moderate amount of surrounding fluid, and calcifications (arrow) affecting the posterior tibial tendon related to chronic tenosynovitis in patient affects rheumatoid arthritis.
- 66. Tenosynovitis of the posterior tibial tendon caused by a bony ridge at the insertion of the retinaculum. The retinaculum is thickened and the tendon subluxates.
- 67. Psoriatic arthritis. Ankle. Grayscale examination. Posterior tibial tendon on longitudinal (a) and transverse (b) scan. Marked tendon sheath widening with homogeneous anechoic aspect (asterisks) of the content indicating an exudative tenosynovitis. Note as the normal fibrillar echotexture is conserved. Hand. Flexor tendons of second finger. The volar longitudinal (c) and transverse scan (d) shows a tendon sheath widening with signs of synovial proliferation, presence of intense power Doppler signal surrounding the tendon, and micro interruption of the margin (arrow). e Wrist. Extensor carpi ulnaris tendon (sixth compartment of the extensor tendons; ecu) on lateral longitudinal (e) and transverse (f) scan. Chronic tenosynovitis with clear areas of low of echogenicity and loss of the continuity of tendon fibrils indicative of partial tendon tear (arrows). Moreover, note the presence of power Doppler signal within the interruption indicating still activity of the inflammatory process. g Dactylitis. Volar longitudinal scan using the “extended view” technique, showing proliferative tenosynovitis of the finger flexor tendon (circle), exudative synovitis of both proximal and distal interphalangeal joint (white asterisks) and edema of the peritendinous tissue (black asterisks). TP posterior tibial tendon, mm medial malleolus, DP distal phalanx, mp middle phalanx, cu cubital bone, ft flexor tendons.
- 68. Tenosynovitis of the posterior tibial (*1) and flexor digitorum longus tendon (*2)
- 69. Tibialis Posterior Tendon rupture.
- 70. Tenosynovitis of the posterior tibial tendon, the flexor digitorum tendon and flexor hallucis longus tendon
- 71. Tenosynovitis of the tendons on the medial side in the left ankle.
- 72. •LIGAMENT INJURIES The ligament partial tear ligament shows a hypoechoic areas swollen with internal focal or diffuse. In the complete ruptures within the substance of the divided ligament rift is observed corresponding to the hematoma hypoechoic, and the free ends of the divided ligament can be and retracted appreciated corrugated, in contrast with normal appearance straight. Grade I: Mild stretching of the ligament, without breakage or instability. Grade II: Partial tearing of the ligament Grade III: Complete tearing. Degrees depending on the severity of the injury and the place of employment.
- 73. LATERAL COMPARTMENT These injuries occur secondary to inversion sprains, with internal rotation of the foot combined with ankle plantar flexion. The anterior talar fibular ligament tears (ATFL) usually occur as isolated involvement (70%) or associated with calcaneal fibular ligament (CFL) (20-40%), but the posterior talar fibular ligament (PTFL) affects only major trauma involving ankle dislocation. ATFL breaks is associated with breakage of the joint capsule and synovial fluid extravasation into the anterolateral soft ankle, whereas the complete tearing of CFL can communicate the ankle joint and synovial sheath peroneal tendons. Rupture of CFL is rarely associated with superior peroneal retinaculum tear. The CFL is tensioned during dorsiflexion pulling on peroneal tendons laterally, so that absence of its displacement is sign of a complete tear. Within a damaged ligament can also observe calcifications that often correspond to fragments of avulsion bone. During the ultrasound can be performed forced maneuvers to detect to joint laxity and ligament injuries. The anterior drawer test is performed with the feet hanging over the edge of the examination table while the forefoot is pulled anteriorly when the foot is in plantar flexion and inversion. This maneuver helps differentiate partial tears (grade II) of the ATFL to complete (grade III), where the anterior displacement of the talus on the tibia open a crack in the substance becoming more visible the ligament injury.
- 74. The sindesmosys sprains are up to 10% of ankle injuries, happening in eversion and pronation movements (like the deltoid ligament injury) and primarily affect the anterior tibiofibular ligament (ATFL), the failure is frequently associated with fracture of the fibula. According to the place of employment are 4 degrees, useful for prognostic evaluation and therapeutic strategy choice. Grade I: stretch or partial tear of the ATFL Grade II: complete tearing but only the ATFL Grade III: complete tear of the ATFL and partial CFL Grade IV: complete tear of the ATFL and CFL. The grade I and II injuries usually scarred without any significant instability, whereas grade III and IV injuries can cause chronic pain and require surgical treatment.
- 75. Thickened but continued ATFL right in relation to the partial rupture.
- 76. Grade 111 sprain of right ATFL.
- 77. Thickened anterior talofibular ligament with calcifications and a partial rupture.
- 78. Thickened tibiofibular ligament after trauma.
- 79. Anterior Talofibular Ligament Partial Tear and Elastography.
- 80. Tibio fibular ligament rupture with bony avulsion.
- 81. Complete rupture of right ATFL.
- 83. Bony avulsion with radiographic evidence as visible calcification in a grade III sprain ATFL.
- 85. Moderately thickened and hypoechoic ATFL.
- 86. Discontinuity of the ATFL with fluid surrounding the torn ends (arrow).
- 87. Thickening and hypoechogenicity of the fibular end of the ligament seen here passing over the subtalar joint which contains a small of fluid.
- 88. Complete disruption to the tibiofibular ligament with bony irregularity of particularly the tibial margin and fluid in the gap.
- 89. MEDIAL COMPARTMENT Because of the low incidence of eversion ankle sprains and the thickness of the deltoid ligament is rarely injured in isolation and when the injury does not usually full thickness. Usually accompanied by lesions of the medial malleolus and lateral displacement of the talus, with consequent widening of the ankle mortise. Ultrasound is useful for differentiating ligament injury of the posterior tibial tendon injury (TP) adjacent, they have similar symptoms. The inability to visualize the deltoid ligament may indicate tear , but this is not considered a reliable sign as its full ultrasound is not always possible.
- 90. Partial medial ligament rupture.
- 91. Thickened heterogeneous abnormal deltoid demonstrating hyperemia.
- 92. Ultrasonogram showing a disrupted deltoid ligament with the probe in the coronal plane. The white arrow indicates the medial malleolus, the blue arrow indicates the talus, and the red arrows indicate the disrupted deltoid ligament (A). Radiograph showing the same injury (B).
- 93. •JOINT AND BONE DISORDERS Ultrasound reliably detect spills mild (> 2 ml) inside of the ankle joint, by exploring the front and rear recess as well as areas of synovial proliferation, and may even display using the colour Doppler hyperemic areas, in arthritis patients. The intraarticular joints are displayed surrounded fluid in one of the recesses of the ankle or subtalar joint. Sonographically diagnosed when changing position to perform flexion and extension. Fracture of the lateral process of the talus is overlooked up to 50% of cases with plain radiography. Ultrasound may suspect the presence of focal cortical disruption, helping further to exclude concomitant ligament injury
- 96. Rheumatoid arthritis with synovial thickening (*1) and erosion of the tibia (*2)
- 97. Infectious arthritis with a pus filled anterior recess of the ankle.
- 98. Arthritis and tenosynovitis of the ankle in a patient with rheumatoid arthritis.
- 99. •TUMOURS Ultrasound can differentiate between a mass complex and solid and a cystic, in addition to verifying the existence of accessory muscles (peroneus fourth, accessory flexor digitorum longus and accessory soleus). As in any other location can be found neoformative soft tissue tumors , inflammatory, infectious, etc. Ganglions of this location are more often symptomatic and larger with multiple partitions branched and lobed edges. Differential diagnosis must be made with tenosynovitis, abscesses, seromas and varicosities. Neurogenic tumours are described as pathognomonic homogeneous hypoechoic oval mass in continuity with a nerve of origin
- 103. Ganglion cysts are non-malignant cystic masses that occur in association with musculoskeletal structures . They are sometimes also simply referred to as ganglia or a ganglion, but should not be confused with the anatomical term ganglion. Ultrasound The vast majority are anechoic to hypoechoic on ultrasound and have well defined margins. Many demonstrate internal septations as well as acoustic enhancement. A synovial cyst is a small, fluid-filled sac or pouch that can develop over a tendon or joint, creating a mass under the skin. Synovial cyst is rare in ankle joint. A synovial cyst may or may not be painful, depending on their size and location.
- 104. Ganglion cyst in the foot with bony erosion between navicular and cuneiform bones
- 106. Anechoic ganglion situated in the sinus tarsi fat between the talus and calcaneous.
- 107. Plantar fasciitis (PF) refers to inflammation of the plantar fascia of the foot. It is considered the most common cause of heel pain. Clinical presentation Pain on the undersurface of the heel on weight bearing is the principal complaint. It can be worse when weight is borne after a period of rest (e.g. in the morning) and eases with walking. Passive dorsiflexion of the toes may exacerbates discomfort. Ultrasound Often the initial imaging modality of choice. Ultrasound typically shows increased thickness of the fascia and a hypoechoic fascia.
- 108. Thickened hypoechoic origin of the plantar fascia which has a convex superior margin.
- 109. Complete avulsion of the plantar fascia from the calcaneal tubercle.
- 110. Plantar fasciitis
- 111. • LOCATING FOREIGN BODIES AND FRACTURES. As in any other location, the ankle area is also subsidiary host foreign whose classification, location and existence can be defined perfectly by ultrasound. Being a focused study to the area of interest and with great resolution for surface structures, can be considered more resolute examination to screen these cases.
- 113. Osseous diseases and fractures | Sonography discovered Medial Malleolus Fracture.
- 114. Ultrasound examination of left ankle. A: Longitudinal sonogram, left ankle, demonstrates a wooden foreign body; B: Transverse view, left ankle. Note the hypervascularity in the inflamed area; C: Corresponding X-ray of left ankle. Note the swelling on the lateral aspect. No foreign body is visible.
- 115. Thank You.
