Samir rafla cardiac arrhythmias for 5th year medical students
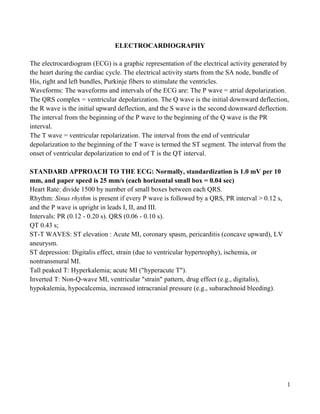
- 1. ELECTROCARDIOGRAPHY The electrocardiogram (ECG) is a graphic representation of the electrical activity generated by the heart during the cardiac cycle. The electrical activity starts from the SA node, bundle of His, right and left bundles, Purkinje fibers to stimulate the ventricles. Waveforms: The waveforms and intervals of the ECG are: The P wave = atrial depolarization. The QRS complex = ventricular depolarization. The Q wave is the initial downward deflection, the R wave is the initial upward deflection, and the S wave is the second downward deflection. The interval from the beginning of the P wave to the beginning of the Q wave is the PR interval. The T wave = ventricular repolarization. The interval from the end of ventricular depolarization to the beginning of the T wave is termed the ST segment. The interval from the onset of ventricular depolarization to end of T is the QT interval. STANDARD APPROACH TO THE ECG: Normally, standardization is 1.0 mV per 10 mm, and paper speed is 25 mm/s (each horizontal small box = 0.04 sec) Heart Rate: divide 1500 by number of small boxes between each QRS. Rhythm: Sinus rhythm is present if every P wave is followed by a QRS, PR interval > 0.12 s, and the P wave is upright in leads I, II, and III. Intervals: PR (0.12 - 0.20 s). QRS (0.06 - 0.10 s). QT 0.43 s; ST-T WAVES: ST elevation : Acute MI, coronary spasm, pericarditis (concave upward), LV aneurysm. ST depression: Digitalis effect, strain (due to ventricular hypertrophy), ischemia, or nontransmural MI. Tall peaked T: Hyperkalemia; acute MI ("hyperacute T"). Inverted T: Non-Q-wave MI, ventricular "strain" pattern, drug effect (e.g., digitalis), hypokalemia, hypocalcemia, increased intracranial pressure (e.g., subarachnoid bleeding). 1
- 2. Fig 1: The magnified ECG wave is presented with the principal time intervals indicated. Fig 2: The pathways of Conduction 2
- 3. CARDIAC ARRHYTHMIAS An arrhythmia is any disturbance in the normal sequence of impulse generation and conduction in the heart. Anatomy of the conduction system: The conduction system of the heart consists of the sinus node, internodal tracts, atrioventricular node (AVN), bundle of His, bundle branches (right and left), and Purkinje fibers. General considerations: Normal cardiac impulses arise from the automatic (pacemaking) cells of the sinus node and are conducted through the atria to the AV junction then the HisPurkinje system to the ventricular muscle. Normally the sinus node discharges at a rate of 60100/min. Mechanisms of arrhythmias A- Disturbance of impulse formation: may result from either: 1- Disturbed normal automaticity: 2- Triggered activity: Myocardial damage can result in oscillations (afterdepolarizations) at the end of the action potential. These oscillations may reach threshold potential and produce an arrhythmia. B- Disturbance of Impulse conduction: 1- Reentry: A wave of depolarization may be forced to travel in one direction around a ring of cardiac tissue. The majority of paroxysmal tachycardias are produced by this mechanism. Classification of arrhythmia: Clinical classification: - Rapid, regular. Sinus tachycardia, supraventricular tachycardia, atrial flutter, ventricular tachycardia. - Rapid, irregular. Sinus arrhythmia, multiple ectopic beats whether atrial or ventricular, atrial fibrillation. - Slow, regular. Sinus bradycardia, nodal rhythm, complete heart block. - Slow, irregular. Slow atrial fibrillation. Anatomical classification: it stratifies arrhythmia according to the site of origin; SA node, atrial, AV node, abnormal pathways, bundles and ventricular. 3
- 4. Mechanismal classification: This depends on the pathogenesis of the arrhythmia. It is divided into disturbance in the formation of the impulse, propagation of the impulse or combined. SPECIFIC ARRHYTHMIAS Sinus node Sinus tachycardia Cardiac impulses arise in the sinus node at a rate more than 100/min. Etiology: A- Physiological: Infancy, childhood, exercise and excitement. B- Pharmacological: Sympathomimetic drugs such as epinephrine and isoproterenol. Parasympatholytic drugs such as atropine. Thyroid hormones, nicotine, caffeine, alcohol. C- Pathological: Fever, hypotension, heart failure, pulmonary embolism, hyperkinetic circulatory states as anemia. Treatment: 1- Treatment of the underlying etiology. 2- Propranolol. Sinus Bradycardia Cardiac impulses arise in the sinus node at a rate less than 60/min. Etiology: A- Physiologic: Athletes, sleep, and carotid sinus compression. B- Pharmacologic: Digitalis, propranolol, verapamil and diltiazem. C- Pathologic: Convalescence from infections, hypothyroidism, obstructive jaundice, rapid rise of the intracranial tension, hypothermia and myocardial infarction (particularly inferior wall infarction). Treatment: 1- Treatment of the underlying etiology is usually all that is needed. 2- If the patient is hemodynamically compromised, Atropine 0.6 – 1.0 mg IV may be given and repeated every 3 hours (maximum 2.5 mg in two hours). 4
- 5. Sinus Arrhythmia Cardiac impulse arises in the sinus node with alternating periods of slowing and acceleration. The condition is common in young age and has no pathological significance. Respiratory sinus arrhythmia: The heart rate increases with inspiration and slows with expiration. The inspiratory increase is secondary to the increased venous return. FIG 3. Normal intracardiac electrograms. SICK SINUS SYNDROME This term is applied to a syndrome encompassing a number of sinus nodal abnormalities that include: 1- persistent spontaneous sinus bradycardia not caused by drugs, and inappropriate for the physiological circumstance, 2- apparent sinus arrest or exit block, 3- combinations of SA and AV conduction disturbances, or 4- alternation of paroxysms of rapid regular or irregular atrial tachyarrhythmias and periods of slow atrial and ventricular rates (bradycardia-tachycardia syndrome). 5
- 6. PREMATURE BEATS (EXTRASYSTOLES) These are cardiac impulses of ectopic origin occurring earlier than expected in the prevailing rhythm. The ectopic focus may be: 1- Atrial resulting in atrial premature beat. 2- AV junctional (arising from bundle of His) resulting in AV junctional premature beat. 3Ventricular resulting in ventricular premature beat. Etiology: A- Physiological: Emotions, exercise and fatigue. B- Pharmacological: Coffee, alcohol, tobacco, catecholamines, digitalis and hypoxia. C- Pathological: Various infections, digestive disturbances, hyperthyroidism and all cardiovascular disorders. SUPRAVENTRICULAR TACHYARRHYTHMIAS All tachyarrhythmias that originate above the bifurcation of the bundle of His are classified as supraventricular arrhythmias. The atrial rate must be 100 or more beats per minute for a diagnosis. SVTs may be separated into three groups based on duration: brief paroxysms, persistent, and chronic (permanent). Arrhythmias that are paroxysmal in onset and offset (e.g., paroxysmal SVT due to AV nodal reentry or WPW syndrome, paroxysmal atrial fibrillation, paroxysmal atrial flutter) tend to be recurrent and of short duration; i.e., seconds to hours. Persistent tachycardias (e.g., sinus tachycardia, ectopic atrial tachycardia (nonparoxysmal), multifocal atrial tachycardia, longer episodes of PSVT or atrial flutter or fibrillation) may persist for days or weeks. Longstanding or chronic SVTs (chronic atrial flutter, chronic atrial fibrillation) do not revert if untreated, often fail to revert even with attempted treatment, and if reverted will frequently recur despite therapy. Supraventricular tachyarrhythmias include; atrial tachycardia, atrial flutter, atrial fibrillation and nodal tachycardia. ATRIAL FLUTTER 6
- 7. Atrial flutter is a rapid regular atrial tachyarrhythmia that is less common than the PSVTs or atrial fibrillation. It is observed infrequently in normal individuals, but may occur at any age in the presence of underlying atrial abnormalities such as those secondary to mitral valve disease, congenital heart disease, cardiomyopathies, and, less frequently, coronary artery disease. Untreated atrial flutter usually has atrial rates between 240 and 340 per minute, commonly very close to 300 per minute. The ventricular rate in atrial flutter is usually a defined fraction of the atrial rate 2: 1 conduction generating a ventricular rate of 150 per minute and 4:1 conduction at 75 per minute. The mechanism of the atrial activity is macroreentry. Clinically, atrial flutter may occur in brief, persistent, or chronic forms, and therapeutic approaches are influenced by the clinical pattern. Electrocardiographic Features Atrial flutter generates a defined pattern of atrial activity in the ECG. Classically, a sawtooth pattern is identifiable in leads II, 111, and aVF. A narrow QRS complex tachycardia at a rate of 150 per minute should always lead to the consideration of atrial flutter. Carotid sinus massage will not interrupt atrial flutter but nonetheless may be very helpful in distinguishing flutter from other mechanisms, impairment of AV nodal conduction causes an abrupt change from a rate of 150 per minute to 75 per minute or less. The unmasking of hidden flutter waves at the slower ventricular rate will make the diagnosis evident. Management of atrial flutter: - If the patient is hemodynamically compromised, D.C. cardioversion using low energies (around 50 joules) should be instituted. - For many years, standard treatment consisted of administering a Class IA antiarrhythmic agent (i.e., quinidine, procainamide, or disopyramide). However, recent studies indicate that the type IC antiarrhythmic drugs, flecainide and propafenone, are as effective, if not more effective than Class IA drugs. Class III antiarrhythmic agents (i.e., amiodarone, sotalol) may also be quite effective. In general, atrial flutter is quite difficult to suppress completely with drug therapy. 7
- 8. - The ventricular rate is slowed by digitalis and/or propranolol or verapamil before antiarrhythmics are instituted to avoid very rapid rates associated with drug induced 1:1 AV conduction. - At present, catheter ablation provides the best hope of cure. FIG 4. A 12-lead ECG of a typical case of type 1 atrial flutter. FIG 5. Atrial flutter with AV block varying between 2: 1 and 4: 1. AV Nodal Reentrant Tachycardia 8
- 9. Electrocardiographic Features PSVT due to AV nodal reentry is characterized by an abrupt onset and termination and usually has a narrow QRS complex without clearly discernable P waves. The rate is commonly in the range of 150 to 250 per minute (commonly 180 to 200 bpm in adults) and with a regular rhythm. Management of PSVT Due to AV Nodal Reentry The acute attack: Management depends on the underlying heart disease and how well the tachycardia is tolerated. For some patients, rest, reassurance, and sedation may be all that are required to abort the attack. Vagal maneuvers serve as the first line of therapy. Table: Simple procedures to terminate paroxysmal SVT - Carotid sinus massage: If effective the rhythm is abruptly stopped; occasionally only moderate slowing occurs - Cold water splash on face (to mimic the diving reflex) - Performance of Valsalva's maneuver (often effective) Intravenous adenosine, Ca channel blockers (verapamil), digoxin or B-blockers are the choices for managing the acute episodes. Adenosine, 6 mg given intravenously, followed by one or two 6-mg boluses if necessary, is effective and safe for acute treatment. A 5-mg bolus of verapamil, followed by one or two additional 5-mg boluses 10 min apart if the initial dose does not convert the arrhythmia, has been an effective regimen in up to 90 percent of patients with PSVT due to AV node reentry. Intravenous digoxin, 0.5 mg infused over 10 min and repeated if necessary may convert the arrhythmia. An additional 0.25 mg every 4 h to a maximum dose of 1.5 mg in 24 h may be used. The class IA antiarrhythmic agents, which appear to depress conduction in the fast pathway, may be tried if other drugs fail. DC cardioversion: Consider DC cardioversion before digitalis or a beta blocker is administered. Radiofrequency catheter ablation: Should be considered early in the management of patients with symptomatic recurrent episodes of AV node reentry. 9
- 10. PSVT Due to Accessory Pathways (The Wolff-Parkinson-White Syndrome) Preexcited AV Node-Dependent Tachycardias Preexcitation Syndrome ELECTROCARDIOGRAPHIC RECOGNITION: Three basic features typify the ECG abnormalities of patients with the usual form of WPW syndrome caused by an AV connection: (1) P-R interval less than 120 msec during sinus rhythm; (2) QRS complex duration exceeding 120 msec with a slurred, slowly rising onset of the QRS in some leads (delta wave) and usually a normal terminal QRS portion; and (3) Secondary ST-T wave changes that are generally directed opposite to the major delta and QRS vectors. The most common tachycardia is characterized by a normal QRS, by ventricular rates of 150 to 250 beats/min and by sudden onset and termination. The prognosis is excellent in patients without tachycardia or an associated cardiac anomaly. For most patients with recurrent tachycardia the prognosis is good but sudden death occurs rarely. Termination of the acute episode of reciprocating (using accessory pathway) tachycardia should be approached as for AV nodal reentry. After vagal maneuvers, adenosine followed by verapamil is the initial treatment of choice. In many patients, particularly those with a very rapid ventricular response, electrical cardioversion is the initial treatment of choice. Oral administration of two drugs, such as quinidine and propranolol or procainamide and verapamil, to decrease conduction capabilities in both limbs of the reentrant circuit, can be beneficial. Class IC drugs and amiodarone, which prolong refractoriness in both the accessory pathway and the AV node, can be effective. ELECTRICAL ABLATION: Ablation of the accessory pathway is advisable for: - patients with frequent symptomatic arrhythmias that are not fully controlled by drugs, or - With rapid AV conduction over the accessory pathway during atrial flutter or fibrillation and in whom significant slowing of the ventricular response during tachycardia cannot be obtained by drug therapy. 10
- 11. Atrial Fibrillation The arrhythmia is characterized by wavelets propagating in different directions and causing disorganized atrial depolarizations without effective atrial contraction. Electrical activity of the atrium can be detected on ECG as small irregular baseline undulations, called f waves, at a rate of 350 to 600 beats/min. The ventricular response is grossly irregular (irregular irregularity) and is usually between 100 and 160 beats/min. It is a common arrhythmia, occurring in 5 – 10 % of individuals over 65 years of age. It also occurs in a paroxysmal form in younger patients. The hemodynamic consequences of atrial fibrillation are due to two factors: (1) The loss of atrial systole may impair ventricular function in the noncompliant ventricle [e.g., aortic stenosis, left ventricular hypertrophy (LVH)] or the dilated ventricle with systolic dysfunction, and (2) A rapid ventricular rate will encroach upon the diastolic filling period of the left ventricle and the diastolic flow time of the coronary arteries. (3) The risk of embolism and stroke is a long-term concern of special importance. Atrial fibrillation may occur in paroxysmal, persistent, and chronic patterns. Clinical expression of atrial fibrillation: Definition Duration - Paroxysmal Minutes/hours - Short-lasting Seconds --<1 hour - Long-lasting >1 hour; -- < 48 hours - Persistent Two days -- weeks - Permanent (Chronic) Months / years Table: Causes of atrial fibrillation With structural heart disease - Rheumatic mitral valve disease - Ischemic heart disease - Hypertension 11
- 12. - Cardiomyopathy: - Dilated, Hypertrophic Atrial septal defect, - Constrictive pericarditis, Myocarditis Without structural heart disease - Alcohol - Thyrotoxicosis - Acute pericarditis - Pulmonary embolism - Sick sinus syndrome, Lone atrial fibrillation 12
- 13. FIG 6. ECG tracings from AV node-dependent and AV node-independent tachycardias. Panel A shows a narrow ORS complex tachycardia with a 1 : 1 AV relationship in a patient with an AV nodal reentrant tachycardia. Panel B shows classic atrial flutter persisting despite 2:1 AV block. Negative retrograde P waves are seen in ECG leads 11, Ill, and aVF. ECG indicates electrocardiogram; and AV, atrioventricular. FIG 7. General scheme to select antiarrhythmic drug therapy for the prevention of atrial fibrillation. See text for details. HPB, hypertension; CHF, congestive heart failure; CAD, coronary artery disease; CR, controlled release; AF, atrial fibrillation. 13
- 14. FIG 8. Protocol for the ACUTE (Assessment of Cardioversion Using Transesophageal Echocardiography) study. Patients with atrial fibrillation were randomised to the conventional approach or to the TEE-guided group. LA, left atrial; LAA, left atrial appendage. Clinical picture Onset and offset are sudden in paroxysmal cases. Symptoms: Paroxysmal AF produces symptoms similar to those of supraventricular tachycardia. Established AF (persisting for more than two weeks) is better tolerated than the paroxysmal variety. Congestive heart failure may occur if the attack is prolonged, the ventricular rate is very rapid, or the underlying heart disease is severe. Signs: 1- Arterial pulse: a- Rate is usually 100-150/min. Slower rates may be encountered in old age and in patients receiving digitalis or beta-blockers. b- Rhythm shows marked (irregular) irregularity. c- Force is irregular. d- Pulsus deficit: The radial pulse rate is less than the cardiac rate counted at the apex beat. This is due to inability of the week ventricular contractions following short diastolic periods to open the aortic valve. 2- Neck veins show systolic expansion; no “a” waves are seen. 3- Auscultation reveals varying intensity of S1. 4- Exercise increases the pulse irregularity and deficit. Electrocardiogram: The P waves are replaced by irregular f waves. The QRS complexes are normal in shape but irregularly spaced. Complications of Atrial Fibrillation: 1- Atrial thrombosis due to stagnation of blood in the fibrillating atria. The formed thrombi may embolize in the systemic and pulmonary circulations. Thrombi in left auricle may embolise to brain causing stroke or transient cerebral ischemic attacks; may embolize to retinal artery causing sudden blindness in this eye; or embolize to other systems. Right auricular thrombi will embolize to the lungs causing pulmonary infarctions. 14
- 15. 2- Heart failure due to loss of the atrial contribution to contractility and the cardiac output. 3Tachycardia induced cardiomyopathy. 4- Complications of treatment as bleeding from marevan Treatment of Atrial Fibrillation Pharmacologic Management of Patients with Recurrent Persistent or Permanent AF: - Recurrent Persistent AF: A) Minimal or no symptoms: Anticoagulation and rate control as needed. B) Disabling symptoms in AF: 1- Anticoagulation and rate control 2- Antiarrhythmic drug therapy 3- Electrical cardioversion as needed, continue anticoagulation as needed and therapy to maintain sinus rhythm - Permanent AF: Anticoagulation and rate control as needed. Antiarrhythmic Drug Therapy to Maintain Sinus Rhythm in Patients with Recurrent Paroxysmal or Persistent AF: A) No or minimal heart disease: 1- Flecainide, propafenone, sotalol 2- Amiodarone, dofetilide 3- Disopyramide, procainamide, quinidine 4- Consider non-pharmacological options. B) Heart disease present: a- Heart failure: Amiodarone, dofetilide b- Coronary artery disease: 1- Sotalol 2- Amiodarone, dofetilide 3- Disopyramide, procainamide, quinidine C) Hypertension: With 1- With LVH (septum greater than or equal to 1.4 cm): Amiodarone 2- Without this degree of LVH: - Flecainide, propafenone. - Amiodarone, dofetilide, sotalol - Disopyramide, procainamide. quinidine 15
- 16. Recommended Doses of Drugs Proven Effective for Pharmacologic Cardioversion of AF (Rhythm Control): Drug Route of Admin. And Dosage Amiodarone Oral: 1.2 to 1.8 g /day then 200 to 400 mg /d maintenance. IV: 1.2 g /d IV continuous or in divided doses, then 200 to 400 mg /d maintenance Dofetilide Oral: Creatinine clearance > 60 ml/min: 500 mcg BID Flecainide Oral 200 to 300 mg IV: 1.5 to 3 mg /kg over 10 to 20 min Ibutilide IV: 1 mg over 10 min; repeat 1m when necessary Propafenone Oral: 450 to 600 mg (Rytmonorm) IV: 1.5 to 2 mg per kg over 10 to 20 min Sotalol Tablet 80 mg give up to 3 tablets per day (Betacor) Quinidine Oral: 0.75 to 1.5 g in divided doses over 6 to 12 h usually with a rate-slowing drug. Recommendations for Use of Orally Administered Pharmacological Agents for Heart Rate Control in Patients with AF (Rate Control): Drug Loading dose Maintenance dose Digoxin 0.25 mg PO each 2h; 0.125 to 0.375 mg daily up to 1.5 mg Diltiazem NA 120 to 360 mg daily in divided doses Metoprolol* NA 25 to 100 BID Propranolol NA 80 to 360 mg daily in divided doses Verapamil NA 120 to 360 mg daily in divided doses Amiodarone 600 mg/d for 1 wk 200 or 100 mg daily 400 mg/d for 4 to 6 wk 16
- 17. * Other beta-blockers could be used in appropriate doses Two other drugs not mentioned here: Dronedarone and Vernakalant. TABLE: ANTICOAGULATION OF PATIENTS WITH ATRIAL FIBRILLATION Indications Rheumatic mitral valve disease with recurrent or chronic atrial fibrillation. Dilated cardiomyopathy with recurrent persistent or chronic atrial fibrillation. Prosthetic valves. Prior to (>3 weeks) elective cardioversion of persistent or chronic atrial fibrillation, and also for 3 weeks after cardioversion (because of atrial stunning). Coronary heart disease or hypertensive heart disease with recurrent persistent or chronic atrial fibrillation Atrial fibrillation in thyrotoxicosis (while awaiting long-term control; elective cardioversion) Chronic or persistent lone atrial fibrillation, age >60 years Controversial; or limited data Coronary or hypertensive heart disease with normal left atrial size, after first episode of paroxysmal atrial fibrillation Elective cardioversion of atrial fibrillation of short duration (2-3 days) with normal left atrial size Chronic or persistent lone atrial fibrillation, age <60 years Not indicated Lone atrial fibrillation, short paroxysms (<48 h) Most clinical settings associated with short paroxysms (minutes to hours) Relative contraindications Difficulty controlling prothrombin times Dementia Malignancies, especially associated with bleeding risk Prior major bleeding events Uncontrolled hypertension 17
- 18. Question: Give the causes of atrial fibrillation, clinical consequences, and different lines of management. TREATMENT OF CARDIAC ARRHYTHMIAS WITH CATHETER ABLATIVE TECHNIQUES Over the past several years various techniques have been introduced using catheter ablative procedures for patients with cardiac arrhythmias. Radiofrequency ablation destroys tissue by controlled heat production and avoids the need for general anesthesia since pain is minimal. Presently, catheter ablation is used to treat patients with four major tachyarrhythmias: atrial flutter/fibrillation, AV nodal reentry, AV reentry and ventricular tachycardia. VENTRICULAR TACHYCARDIA SPECIFIC FORMS OF VENTRICULAR TACHYCARDIA Duration: Salvo (3-5 impulses) Nonsustained VT: (6 impulses, up to 29 seconds) Sustained VT: (>30 seconds) ELECTROCARDIOGRAPHIC RECOGNITION. Ventricular tachycardia arises distal to the bifurcation of the His bundle, in the specialized conduction system, in ventricular muscle, or in combinations of both tissue types. The electrocardiographic diagnosis of ventricular tachycardia is suggested by the occurrence of a series of three or more bizarrely shaped premature ventricular complexes whose duration exceeds 120 msec, with the ST-T pointing opposite to the major QRS deflection. Depending on the particular type of ventricular tachycardia, the rates range from 70 to 250 beats/min, and the onset can be paroxysmal (sudden) or nonparoxysmal. QRS contours during the ventricular tachycardia can be unchanging (Uniform, monomorphic), can vary randomly (multiform, polymorphic), vary in more or less repetitive manner (Torsade de points), vary in alternate complexes (bi-directional ventricular tachycardia), or vary in a stable but changing contour (i.e., right bundle branch contour changing to left bundle branch contour). Ventricular tachycardia can be sustained, defined arbitrarily as lasting longer than 30 sec or requiring termination because of hemodynamic collapse, or nonsustained (Unsustained), when 18
- 19. it stops spontaneously in less than 30 sec. Most commonly, very premature stimulation is required to initiate ventricular tachycardia electrically. CLINICAL FEATURES. Symptoms occurring during ventricular tachycardia depend on the ventricular rate, duration of tachycardia, the presence and extent of the underlying heart disease, and peripheral vascular disease. Management: Termination of Sustained Ventricular Tachycardia: Ventricular tachycardia that does not cause hemodynamic decompensation can be treated medically to achieve acute termination by administering intravenous lidocaine or procainamide, followed by an infusion of the successful drug. If the arrhythmia does not respond to medical therapy, electrical DC cardioversion can be employed. Ventricular tachycardia that precipitates hypotension, shock, angina, or congestive heart failure or symptoms of cerebral hypoperfusion should be treated promptly with DC cardioversion. Very low energies can terminate ventricular tachycardia, beginning with a synchronized shock of 10 to 50 watt-seconds. Digitalis-induced ventricular tachycardia is best treated pharmacologically. After conversion of the arrhythmia to a normal rhythm, it is essential to institute measures to prevent a recurrence. A search for reversible conditions contributing to the initiation and maintenance of ventricular tachycardia should be made and the conditions corrected if possible. Prevention of Recurrences: This is generally more difficult than is terminating the acute episode, and there is no "right" drug to choose. Although amiodarone is very effective, side effects limit its use. 19
- 20. Fig 9. Ventricular rhythm disturbances. A, Idioventricular rhythm. B, Multiple ventricular premature complexes (arrows). C, Monomorphic ventricular tachycardia at a rate of 200 beats/min. The QRS complex is wide and p waves are seen to occasionally alter the QRS morphology (arrows), reflecting AV dissociation. D, Polymorphic ventricular tachycardia (torsade de pointes). (Note: the rhythm strip is at half the usual speed). There is QT prolongation and several complexes occur at the peak of the preceding T waves (arrows) with resultant induction of a wide-complex tachycardia that appears to rotate around the base line. E, Ventricular fibrillation. 20
- 21. Fig 10. Electrocardiographic characteristics of right ventricular dysplasia. A: A ventricular tachycardia having a left bundle-branch block QRS morphology and a left axis deviation. B: The electrocardiogram during sinus rhythm in the same patient. Note the inverted T waves across the anterior chest leads. . Fig 11. Typical characteristics of Torsade des Pointes. 21
- 22. Specific Types of Ventricular Tachycardia Torsade de Pointes ELECTROCARDIOGRAPHIC RECOGNITION. The term "torsades de pointes" refers to a ventricular tachycardia characterized by QRS complexes of changing amplitude that appear to twist around the isoelectric line and occur at rates of 200 to 250/min. More recent data suggest that early afterdepolarizations may be responsible for both the long Q-T and the torsades de pointes. CLINICAL FEATURES. While many predisposing factors have been cited, the most common are congenital, severe bradycardia, potassium depletion, and use of class IA and some IC drugs. Clinical features depend on whether the torsades de pointes are due to the acquired or congenital (idiopathic) long Q-T syndrome. In all patients with torsades de pointes, administration of class IA, possibly some class IC, and some class II antiarrhythmic agents can increase the abnormal Q-T interval and worsen the arrhythmia. Class IB drugs can be tried. CONGENITAL LONG QT INTERVAL SYNDROME The congenital long QT interval syndrome, which is present persistently from childhood, is characterized by the presence of long QT intervals and/or prominent U waves on the standard 12-lead ECG. The affected patients are prone to episodes of torsade de pointes, which may cause transient light-headedness or syncope or sudden cardiac death. Arrhythmias may occur at rest, under emotional stress, or with exercise. The two general patterns of the syndrome are the Romano-Ward syndrome, which has an autosomal dominant inheritance pattern, and the Jervell-Lange-Nielson syndrome, which has an autosomal recessive inheritance pattern and is associated with congenital deafness. Drugs that block the sodium channel, such as mexiletine, have been suggested as a possible pharmacologic therapy for this specific variant of the syndrome. ACQUIRED LONG QT INTERVAL SYNDROME The most common causes for acquired long QT interval syndromes are the antiarrhythmic drugs, classically quinidine but also other class IA agents and class III agents. Bradycardia, hypokalemia, and hypomagnesemia contribute to the risk. The class III drugs, particularly sotalol, prolong the QT interval in a dose-dependent pattern. 22
- 23. There is a growing list of other drugs that may prolong the QT interval, and establish susceptibility to torsade de pointes. These include the phenothiazines, certain antibiotics, pentamidine, cocaine, and terfenadine, among others. MANAGEMENT OF CONGENITAL LONG QT INTERVAL SYNDROME Long-term therapy includes B-adrenergic blockade. Placement of an ICD should be considered for patients with resistant arrhythmias. MANAGEMENT OF ACQUIRED LONG QT INTERVAL SYNDROME Treatment is directed at the underlying cause(s), with careful attention to electrolyte and metabolic disturbances and to identifying and reversing or removing iatrogenic factors. Intravenous magnesium sulfate is often effective, especially when torsades de pointes are due to quinidine. Lidocaine also may be beneficial, as may other class IB drugs. These drugs tend to shorten the QT interval in normal myocardium. CARDIOVERSION AND DEFIBRILLATION Differences between cardioversion and defibrillation: Cardioversion Defibrillation Elective Emergency Synchronized Non-synchronized For AF, A. flutter, SVT, VT For V. fibrillation 50, 100, 150, 200 Joules Start by 200 Joules Need sedative first Patient is unconscious VENTRICULAR FLUTTER AND FIBRILLATION MANAGEMENT. Immediate nonsynchronized DC electrical shock using 200 to 360 joules is mandatory treatment for ventricular fibrillation and for ventricular flutter that has caused loss of consciousness. Cardiopulmonary resuscitation is employed only until defibrillation equipment is ready. Time should not be wasted with cardiopulmonary resuscitation maneuvers if electrical defibrillation can be done promptly. Defibrillation requires fewer joules if done early. 23
- 24. The Implantable Cardioverter Defibrillator (ICD) TABLE: GUIDELINES FOR ICD IMPLANTATION 1. ICD indicated A. Cardiac arrest not due to acute ischemia or infarction or reversible causes B. Documented sustained VT with hemodynamic compromise C. Syncope of unknown origin in structural heart disease patients with inducible sustained VT. D. Cardiomyopathy ischemic or non-ischemic with ejection fraction 30% or lower (MADIT II results) II. ICD may be indicated in highly symptomatic long QT interval despite optimal medical therapy. AV HEART BLOCK Heart block is a disturbance of impulse conduction that can be permanent or transient, owing to anatomical or functional impairment. The conduction disturbance is classified by severity in three categories. During first degree heart block, conduction time is prolonged but all impulses are conducted (P-R interval > 0.2 sec.). Second degree heart block occurs in three forms: Mobitz type I (Wenckebach) and type II; and persistent 2:1 block. Type I heart block is characterized by a progressive lengthening of the conduction time until an impulse is not conducted. Type II heart block denotes occasional (Mobitz II) or repetitive sudden block of conduction of an impulse without prior measurable lengthening of conduction time. When no impulses are conducted, complete or third degree block is present. COMPLETE AV BLOCK ELECTROCARDIOGRAPHIC RECOGNITION: Complete AV block occurs when no atrial activity conducts to the ventricles and therefore the atria and ventricles are controlled by independent pacemakers. Thus, complete AV block is one type of complete AV dissociation. The atrial pacemaker can be sinus or ectopic (tachycardia, flutter, or fibrillation). The ventricular focus is usually located just below the region of block, which can be above or below the His bundle bifurcation. Sites of ventricular pacemaker activity that are in, or closer 24
- 25. to the His bundle appear to be more stable and may produce a faster escape rate than those located more distally in the ventricular conduction system. The ventricular rate of acquired complete heart block is less than 40 beats/min but may be faster in congenital complete AV block. The ventricular rhythm, usually regular, can vary owing to premature ventricular complexes, or a shift in the pacemaker site. CLINICAL FEATURES. Complete AV block can result from block at the level of the AV node (usually congenital), within the bundle of His, or distal to it in the Purkinje system (usually acquired). Block proximal to the His bundle generally exhibits normal QRS complexes and rates of 40-60 beats/min because the escape focus that controls the ventricle arises in or near the His bundle. Unusual forms such as paroxysmal AV block or AV block following a period of rapid ventricular rate can occur. Paroxysmal AV block in some instances can be due to hyperresponsiveness of the AV node to vagotonic reflexes. Surgery, electrolyte disturbances, endocarditis, tumors, Chagas' disease, rheumatoid nodules, calcific aortic stenosis, myxedema, polymyositis, infiltrative processes (such as amyloid, sarcoid, or scleroderma). In the adult, drug toxicity, coronary disease, and degenerative processes appear to be the most common causes of AV heart block. MANAGEMENT: Drugs cannot be relied on to increase the heart rate for more than several hours to several days in patients with symptomatic heart block without producing significant side effects. Therefore, temporary or permanent pacemaker insertion is indicated in patients with symptomatic bradyarrhythmias. Vagolytic agents such as atropine (novatropine 15 drops every 8 hours) are useful for patients who have AV nodal disturbances, while catecholamines such as isoproterenol (Allupent syrup 5 ml every 8 hours) can be used transiently to treat patients who have heart block at any site. Isoproterenol should be used with extreme caution or not at all in patients who have acute myocardial infarction. The use of transcutaneous pacing is preferable. 25
- 26. Fig 12. Heart block. A, First degree atrioventricular (AV) block; the PR interval is prolonged. B, Second-degree AV block, type 1 (Wenckebach). There is progressive PR prolongation preceding a nonconducted P wave (arrows). C, Second degree AV block, type 11. Nonconducted P waves are seen (arrows) in the absence of progressive PR prolongation. D, Third degree (complete) AV block with AV dissociation and a narrow-complex (AV nodal) escape rhythm. (Reproduced from Cecil Essentials of Medicine). Antiarrhythmic Drugs Class Mode of Drugs Action Class Reduces Quinidine IA rate of (Quinidine) entry of sodium into the cell Indication Dose For 600 – supraventricular 1000 and ventricular mg/day arrhythmias including conversion of AF or A flutter, SVT, VT Side Effects Marked prolongation of QT interval, risk of Torsade de pointes. Quinidine syncope, quinidine induced sudden 26
- 27. Procainamid Is effective e against (Pronestyl) supraventricular and ventricular arrhythmias Disopyrami Is effective de against (Norpace) supraventricular and ventricular arrhythmias Class IB Lidocaine (Zylocain) Mexiletine (Mexitil) Class IC 2-6 mg/min IV. 3501000 mg q 6 h PO 100-400 mg q 8 h Ventricular 1-4 arrhythmias only mg/min IV (50150 mg IV loading dose) Ventricular 150-300 arrhythmias only mg q 6-8 h death. Diarrhea, vomiting SLE like syndrome, prolonged QT, nausea, rash, myalgia, Worsening of heart failure, anticholinergic actions as urine retention, dry mouth. Avoid in pts with glaucoma Confusion, convulsions Confusion, tremor, bradycardia, hypotension Flecainide Is very effective 100-200 Aggravation of (Tambocor) for ventricular mg q 12 h arrhythmia and PO (proarrhythmia), supraventricular negative tachycardias inotropic effect, depression of sinus node Propafenone Has a rule in 150-300 Negative (Rytmonor treatment of mg q 8-12 inotropic effect m) many types of h arrhythmias including supraventricular arrhythmias 27
- 28. Class Beta adrenerg II ic blockers e.g. Propranolol (Inderal), Atenolol, Bisoprolol, Carvedilol For premature beats atrial and ventricular, for torsade de pointes, 10-200 mg q 8 h PO Bradycardia, hypotension, heart failure, intermittent claudication, worsening of asthma, impotence Class Prolong Amiodarone Life-threatening 200-400 Corneal deposits, III action (Cordarone) ventricular mg q 6-8 photosensitivity, potential arrhythmias, h skin duration conversion and pigmentation, slowing of atrial thyroid fibrillation, disturbances AVNRT, (hypo & tachycardias hyperfunction), associated with alveolitis, liver WPWs enzyme elevation Sotalol Effective in 80-160 Torsade de (Betacor) supraventricular mg x 2-3 pointes, and ventricular PO bronchospasm in arrhythmias asthmatic patients Ibutilide FDA approved 1 mg over Torsade de (Covert) for rapid 10 min IV pointes conversion of recent AF & A flutter Dofetilide Approved for 0.1 – 0.5 Torsade de (Tikosyn) oral therapy of mg q 12 h pointes AF & flutter PO Dronedaron For prevention 400 mg Contraindicated e (Multaq) of recurrence of /tab twice for Heart Failure AF (for daily Class III, IV maintenance of sinus rhythm) Class Calcium Verapamil Slow the 0.1 Mg/kg Constipation, IV antagoni (Isoptin) ventricular rate IV 40-160 edema of LL, sts Diltiazem in AF or flutter, mg q 6-8 negative treat and prevent h PO inotropic effect AVNRT 60-120 mg q 6-8 h PO Uncla Activate Adenosine Is very effective 6-18 mg Contraindicated 28
- 29. ssified s K+ (Adenocore) for the acute IV rapidly in sick sinus s., channels conversion of or 2nd or 3rd˚ paroxysmal SVT heart block. Antidote is theophylline Enhance Digoxin s central (Lanoxin, and Cardixin) peripher al vagal tone Slow ventricular 0.5 – 1 rate in AF, mg IV or flutter 0.125 – 0.25 mg /d PO Bradycardias and tachycardias (atrial, junctional, vent. tachycardia), nausea, vomiting Sudden Cardiac Death Definition Natural death due to cardiac causes, within one hour of the onset of acute symptoms in a person with known or unknown cardiac disease, but the time and mode of death are unexpected’. Common Causes of SCD CAD (80 %) DCM (10 %) Other CM: HCM, RVCM (ARVD). Myocarditis. Non atherosclerotic CAD: Anomalies, M Bridge Congenital HD: F4, TGA, AS, PS Valvular HD: AS, AR, MVP, MS, … Primary Electrical Abnormalities: LQTS, Brugada S., CPVT, IMVT, IVF, WPW, Bradyarrhythmias. Congenital Arrhythmogenic Syndromes With structural heart disease: - Right ventricular dysplasia - Hypertrophic cardiomyopathy - Dilated cardiomyopathy - Significant mitral valve prolapse 29
- 30. - Anomalous coronary artery With no or minimal structural heart disease - Long QT syndrome - Brugada syndrome - Wolff Parkinson White syndrome - Idiopathic ventricular tachyarrhythmias - Short QT, catecholaminergic VT - Congenital complete heart block Clinical syndromes treated with ICD implantation (Implantable Cardioverter Defibrillator) - Ejection fraction below 35%, ischemic or no ischemic cardiomyopathy. Cardiac arrest survivors. VT not hemodynamically well-tolerated Idiopathic cardiomyopathy/syncope or VT Hypertrophic cardiomyopathy/syncope or VT RV dysplasia Long QT syndrome Brugada syndrome 30
