Eye disorder.ppt
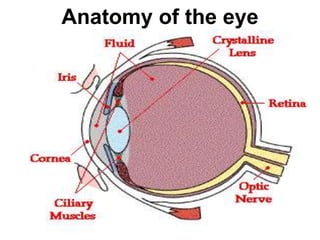
- 1. 1 Anatomy of the eye
- 2. 2 The front part of the eye
- 3. 3 Anatomy of the Eye
- 4. 4 1. Assessment of the eye and vision Subjective data-includes complaints of altered vision or other symptoms, associated lifestyle and other factors, and recent and past health history Presenting symptoms • Any blurred vision, double vision, and loss of vision or a portion of the visual field? • Is there pain, headache, foreign body sensation, photophobia, redness, itchiness, lacrimation? • Is there difficulty in functioning such as driving or reading due to visual problem? Associated factors • Does the patient wear contact lenses or glasses? • What is the patient’s occupation? • How long have there been symptoms? History • Any eye injury or accident • Any recent infections • Any ocular history, such as previous injury, surgery, or use of medication • Medical history such as diabetes, and hypertension
- 5. 5 A. Tests of visual acuity/Snellen chart/ Visual acuity is a measure of the resolving power of eye. It can be for the near or distant vision. Nurse’s responsibility • Assessment of near vision is to ask client to read printed materials under adequate light • If the client is unable to read, the nurse uses an E- chart or one picture of familiar objects • The client is instructed to hold the material at a distance of 5 to 6 cm from the eyes • If the patient has a complaint of visual problems at near, and for all patients 40 years of age or older, the nurse tests the near visual acuity Examination, investigation, and nursing responsibilities
- 7. 7 Continued…Tests of visual acuity/Snellen chart/ • Assessment of distant vision requires use of Snellen chart (paper chart). The chart should be well lighted • The nurse has the client to sit or stand 20 feet/6 meter/ away from the chart and try to read all of the letters beginning at any line with both eyes open and then with each eye separately (with the opposite eye covered) • When covering the eye, the client shouldn’t apply pressure to the eye • If the patient reads the line with two or fewer errors the examiner instructs the patient to read the next lower line
- 8. Continued…Tests of visual acuity/Snellen chart/ • The nurse notes the smallest line the patient can read with two or fewer errors, and records the standard of 20 feet (6 meters) and then the distance in feet on the line of the Snellen chart the patient read successfully • The test is repeated with the client wearing corrective lenses • The nurse does the test rapidly enough that the client doesn’t memorize the chart 8
- 9. 9 Continued…Tests of visual acuity/Snellen chart/ • The nurse records visual acuity as with out correction (sc) or with correction (cc) depending on whether or not the client wears glasses or contact lenses • The nurse then asks the patient to cover the other eye and the processes is repeated • If the patient cannot read letters, the examiner can use an eye chart with pictures, numbers, letter E in four different directions (the examiner asks the patient to point the direction of the E) • If the patient is unable to see the 20/400 letter, the nurse holds up a number of fingers 3 to 5 feet (0.9 to 1.5 meters) in front of the patient and asks the patient to count them • If the patient is unable to count the fingers, the nurse holds up a different number of fingers at successively close distance up to 1 feet and again asks the patient to count them • If the patient could count the number of fingers at 2 feet (0.6 meters) the nurse records the acuity as FC or CF (Finger Count or Count Fingers) at 2 feet (0.6 metes)
- 10. 10 Continued…Tests of visual acuity/Snellen chart/ • If the patient can not count fingers, the nurse asks the patient to indicate if moving the hand is seen in front of the face, the level of visual acuity is HM (Hand Motion) • The abbreviation LP (Light Perception) is used for patients with visual acuity of only light can be seen – If client note when the light is turned on or off, light perception is intact • The abbreviation NLP (No Light Perception) is used for patients with visual acuity of unable to identify light perception • The Snellen chart has standardized number at the end of each line of the chart. The numerator is the number 20, or the distance the client stands from the chart. The denominator is the distance from which the normal eye can read the chart • The largest the denominator, the poorer the clients visual acuity • The nurse records the visual acuities using ophthalmic abbreviations • A normal person is able to read letters at a distance of 20 feet/6 meters/, there fore the normal vision is 20/20
- 11. 11 2. Ophthalmoscopic examination Ophthalmoscope is a hand held instrument with a light source and magnifying lenses that is held close to the patients eye to visualize the posterior part of the eye • The ophthalmoscope is used to inspect the cornea, lens, and the fundus (retina, choroids, optic nerve) • There is no pain or discomfort associated with these examinations • As a rule the patient sits and the examiner stands facing each other with their eyes at the same height • When the right eye is examined the examiner holds the ophthamoscope on the right hand and stands on the right side of the patient • The examination requires dark room
- 13. 13 Ophthalmoscopic examination…continued • The client removes eye glasses, but contact lenses may be left in place • The examiner’s right hand and eye are used to examine the client’s right eye, and the left hand and eye are used to examine the client’s left eye • The ophtalmoscope is held comfortably against the examiner’s face • As the client gazes, straight a head with both eyes open, the examiner, at a distance of approximately 25 cm from the client and 25 degrees lateral to the client’s central line of vision shines the light on the pupil • The light from the ophthalmoscope causes the pupil to constrict • The nurse must relax and keep both eyes open
- 15. 15 Ophthalmoscopic examination…continued • The examiner inspects the size, color, and clarity of the disk; checks the integrity of the vessels, looks for the presence of retinal lesions; and assesses the appearance of the macula and fovea • Normally the following structures are observed: – A clear, yellow optic nerve disc – Reddish pink retina (whites) or darkened retina (African-Americans) – Light red arteries and dark red veins – The avascular macula
- 16. 16 Normal eye
- 19. 19 3. Measurement of intraocular pressure Intraocular pressure is the pressure of the eye • Intraocular pressure is measured by using an instrument called Tonometer (Schiotz’s tonometry) • Use of the intraocular pressure measurement is to determine the intraocular pressure Procedure • The patient lies supine and both eyes are anesthetized by using tetracaine/amitocaine • Ask the patient to place his thumb far from his forehead • As the patient stare directly upward to his own thumb finger, the lids are opened wider, the foot of the tonometer is set lightly but firmly on the center of the cornea • A reading is quickly taken, while the shaft of the tonometer is held absolutely vertical • The normal intraocular pressure is between10-21 mmHg
- 20. 20 Tonometer
- 21. 21 3. Measurement of intraocular pressure…continued Nurse’s responsibility • Clean the tonometer before each use by carefully wiping the foot plate with a moist sterile cotton swab and sterilize the instrument once a day (dry heat) • Wash hands on each patients exam • Make sure that the tonometer is very clean and dry, even a tiny speck of dirt, or grease or moisture can cause friction in the plunger and so give an inaccurate readings • Measurement of intraocular pressure in patient’s with corneal ulcer should be done in great care
- 22. 22 Slit lamp with aplanation tonometer
- 23. 23 4. Estimation of the visual field Visual field-useful in detecting decreased peripheral vision Procedure • Patient is seated 18 to 24 inches in front of the examiner • One eye is covered while the patient focuses with the other eye on a spot about 1 feet from the eye • A test object is brought in from the side at 15 degree intervals, through complete 360 degrees • The patient signals when he or she sees the test object and again when the object disappears through the 360 degrees
- 24. 24 Refraction errors/Ametropia Refraction error is a pathological condition where parallel rays of light are not brought to focus on retina, because of defect in refractive media that is the cornea and lens • Refraction is the ability of the eye to bend light rays so that they fall on to the retina • In the normal eye, parallel light rays are focused through the lens in to a sharp image on the retina, this condition is termed as emmetropia and it is to mean that light is focused exactly on the retina, not in front of it or behind it • When the light does not focus properly, it is called a refractive error Refractive errors can be: • Myopia • Hypermetropia • Astigmatism • Presbyopia • Aphakia
- 25. 25 A. Myopia/Near sightedness/ • The individual with this condition see near objects clearly (near sightedness/short sightedness), but objects at a distance are blurred • This condition occurs when an image is focused in front of the retina, because the eye is too long, or because there is excessive refracting power (cornea or lens have excessive refractive power) • A concave lens/minus/ is used to correct the light refraction so that objects seen in the distance are focused clearly on the retina (bends light ray outward)
- 28. 28 B. Hypermetropia/farsightedness • The individual with this condition see distant objects clearly (farsightedness/long sightedness), but close objects are blurred • This condition occurs when an image is focused behind the retina, either because the eye is too short, or because there is inadequate refracting power (cornea or lens have inadequate refractive power) • A convex lens/plus/ is used to correct the refraction (lens bends light ray in ward)
- 31. 31 C. Astigmatism • Is caused by unevenness in the corneal or lenticular curvature causing horizontal and vertical rays to be focused at two different points on the retina, which results in visual distortion (blurred vision) • It can be myopic or hypermetropic in nature in relation to where the image falls
- 32. 32 Astigmatism
- 34. 34 D. Presbyopia • Is a form of hypermetropia that occurs as a normal process of aging, usually around the age of 40 • As the lens ages and becomes less elastic, it loses its refractive power, and the eye can no longer accommodate for near vision • As with hypermetropia, convex lenses are used to correct the light refraction so that the presbyopic individual can see clearly to read and accomplish other near vision tasks by reading glass /bifocals/ or pogressive lense
- 35. 35 E. Aphakia • Is the absence of the crystalline lens • The lens may be absent congenitally, or it may be removed during cataract surgery or due to trauma • Eye loses approximately 30% of its refractive power and no near vision • Currently correction is by implanting intraocular lens (IOL)
- 37. 37 Cataract
- 38. 38 1. Hordeolum/sty/ Hordeolum (sty) is an acute suppurative infection of the sebaceous glands in the eye lid margin Etiology/cause • Staphylococcus aureus Clinical manifestation • The lid becomes red and edematous • Small collection of pus in the form of an abscess • Pain Management • Warm and moist compress application 3-4 times a day for 10 to 15 minutes • If condition is not improved after 48 hours, incision and drainage may be indicated • Application of topical antibiotics may be prescribed there after External ocular disease
- 40. 40 2. Chalazion Chalazion- is blockage of the meibomian gland in the lids Etiology/cause • Obstruction of the meibomian gland Clinical manifestation • Painless swelling that is firm • Reddened area • The swelling is at some distance from the lid margin Management • Warm and moist compress application 3-4 times a day for 10-15 minutes, especially in the early stage • Most often surgical excision is indicated • Corticosteroid injection to the chalazion lesion
- 41. 41 Chalazion
- 42. 42 Chalazion
- 43. 43 Chalazion
- 44. 44 3. Blepharitis Blepharitis is inflammation of both eye lid margins It can take the form of: • Staphylococcal blepharitis • Seborrheic blepharitis 1. Staphylococcal blepharitis • Is usually ulcerative and is more serious due to involvement of the base of hair follicle • Permanent scaring can result 2. Seborrheic blepharitis • Is chronic and usually resistant to treatment, but the milder cases may respond to lid hygiene
- 45. 45 Blepharitis
- 46. 46 Blepharitis
- 47. 47 Blepharitis Clinical manifestation • The lids are red rimmed with many scales or crusts on the lid margins and lashes • Itching • Burning, irritation, and photophobia • Conjunctivitis may occur simultaneously Management • Staphylococcal blepharitis requires topical antibiotics • Instruction on lid hygiene (to keep the lid margins clean and free of exudates) are given to the patient for both staphylococcal and seborrheic
- 48. 48 Disease of the conjunctiva 1. Conjunctivitis/pink eye/ Conjunctivitis is inflammation of the conjunctiva • It is the most common ocular disease world wide • It is characterized by a pink appearance (hence the common term “pink eye”), because of subconjunctival blood vessel hemorrhages Etiology • Bacteria: haemophilus influenza, staphylococcus aureus, etc (Bacterial conjuctivitis) • Virus: adenovirus, herpes simplex virus, etc (Viral conjuctivitis) • Allergy: allergy to pollens and other environmental allergens, etc (Allergic conjunctivitis) • Toxins: chemicals like chlorine, exposure to fumes, smoke, hair sprays, etc (Toxic conjunctivitis)
- 52. 52 Clinical manifestation • Redness in the white of the eye or inner eye lid • Foreign body sensation • Scratching or burning sensation • Itching • Photophobia • Discharge • Increased amount of tears • The infection usually starts in one eye and then spreads to the other eye by hand contacts Assessment and diagnostic findings • Types of discharge: watery, mucoid, mucopurulent or purulent • Eye swab for culture and sensitivity test
- 53. 53 • Topical antibiotics, eye drops or ointment • For viral conjunctivitis, since not responsive to any treatment cold compress may alleviate some symptom • For allergic conjunctivitis, especially recurrent type corticosteroids in ophthalmic preparations • Use of vasoconstrictors • Cold compress, ice packs, and cool ventilation usually provide comfort by decreasing swelling • For toxic conjunctivitis caused by chemical irritants- eye irrigation with saline or sterile water Management
- 54. 54 • Aware the patient the contagious nature of the disease, especially the bacterial and viral type of conjunctivitis – Emphasis hand washing – Avoid sharing hand towels – Avoid sharing face clothes – Avoid sharing eye drops – Tissue paper should be directly discarded in to a trash can after use – Using new tissue paper every time you wipe the discharge • All forms of tonometry must be avoided, unless medically indicated • Wearing dark glasses for the photophobia Management…cont.
- 55. 55 2. Trachoma Trachoma (rough eye) is a highly contagious eye disease which may result in blindness Etiology/cause • Chlamidia trachomatis Pathophysiology • Scaring of the inside of the eye lid • The eye lid turns inward and the lash rubs the eye ball • Scaring of the cornea (the front eye) • Irreversible corneal opacities and blindness Mode of transmission • Direct contact with eye, nose and throat secretions from infected individuals or contact with objects such as towel, handkerchiefs, fingers, flies, or wash clothes
- 56. 56 Clinical manifestations • Swollen eye lids with pain • Eye discharge which is slightly mucopurulent • Photophobia • Conjunctival follicles and papillae , especially on the upper tarsal conjunctiva • Entropion or trichiasis of the upper lid • Scarring of the upper tarsal conjunctiva • Pannus blood vessels on the upper part of the cornea • Corneal scarring
- 62. 62 Entropion
- 63. 63 Corneal vascularization and scaring
- 64. 64 Acute secondary bacterial infections
- 65. 65 Management • Surgery: Trichiasis and entropion • Antibiotics: TTC, Sulphonamides, Erythromycin • Facial cleanliness: good hand and face washing practice • Environmental changes: address water shortage, eradicate flies, avoid crowded households, etc SAFE strategy (Global Elimination of Trachoma, GET 2020)
- 66. 66 Disease of the cornea 1. keratitis Keratitis is inflammation of the cornea Etiology • Bacteria: Staphylococcus aureus, Streptococcus pneumoniae, pseudomonas aeruginosa, etc • Fungus: candidia, aspergillus, cephalosporium, etc • Virus: herpes simplex, varicella zoster virus, etc • Exposure: exophthalmos, lagophtalmos, etc Clinical manifestaion • Eye pain • Vision loss/blurred vision • Sensation of foreign body • Photophobia • Watering
- 68. 3/16/2023 68
- 69. Lagophthalmos
- 70. 70 keratitis
- 71. 71 Diagnostic test • Slit lamp examination after the eye stained with fluorescein Herpes simplex keratitis stained with fluorescein
- 72. 72 Management • Think blink- for exposure type • Broad spectrum antibiotic for bacterial type (drops and systemics) • Acyclovir for viral type • Natamycin for fungal type • Application of moisturizing ointment for exposure type • Wearing sun glass-day time • Keratoplasty- corneal transplantation
- 74. 74 2. Corneal ulcer-ulceration of the cornea Etiology Bacteria - Streptococcus pneumonia - Pseudomonas - Staphylococcus aureus Fungus - Aspergillus - Candidia albicanus Clinical manifestation – Pain – Blurred vision – Photophobia – Epiphoria – The ciliary vessels around the cornea will be dilated
- 75. 75 A dendritic herpes simplex corneal ulcer stained with fluorescein
- 76. 76 Diagnostic tests • Visible ulcer if the ulcer is larger and deeper • Instillation of fluorescein dye in to the conjunctiva sac • The anterior chamber may contain an inflammatory exudates in severe cases it may form hypopyon • Gram stain and microscopic examination with possible culture and sensitivity test Management • Treat urgently Antibacterial • Gentamycin eye drops • Ciprofloxacilin eye drops Antifungal • Natamycin eye drops • Econazole eye drops
- 77. 77 Intraocular disease 1. Cataract Cataract is clouding or opacity of the crystalline lens that impairs vision • According to WHO, cataract is the leading cause of blindness in the world (2002) Etiology • Aging (senile cataract) • From birth (congenital cataract) • Eye injury (traumatic cataract) • Intraocular diseases like uveitis • Drugs like corticosteroids • Additional risk factors include: diabetes, ultraviolet light exposure, high dose of radiation therapy, etc
- 78. 78 Cataract
- 79. 79 Clinical manifestations • Gradual, progressive, and painless loss of vision • Double vision/blurred vision • Reduced light transmission • Rainbow/haloes/ • Previously dark pupil may appear milky or white Diagnostic assessment • History and physical examination • Ophthalmoscopic examination • Slit lamp examination Management Surgery • Surgical removal of the lens-usually done under local anesthesia • Intra Ocular Lens (IOL) are usually implanted at the time of cataract extraction
- 81. 81 Nursing • Preoperative care/preparing the patient for surgery/ – Orient patient and explain procedures and plan of care to decrease anxiety – Instruct patient not to touch eyes to decrease contamination – Administer preoperative eye drops • Post operative care – Medication as prescribed – Teach the patient to report sudden pain and restlessness with increased pulse – Caution patient against coughing, sneezing, rapid movement, bending – Encourage patient to wear shield at night to protect operated eye from injury while sleeping
- 82. 82 Disease of the sclera 1. Scleritis Scleritis-is an inflammation and swelling of the sclera Etiology • Associated with connective tissue disorders like rheumatoid arthritis Clinical manifestation • Severe pain • The white part of the eye may appear red, swollen and a nodule which is painful to touch Management • Heavy immunosupperesion may be needed – Systemic corticosteroids and eye drops – Systemic NSAID’s and treating the underlining cause.
- 83. 83 Disease of the uveal tract 1. Uveitis Uveitis- is inflammation of uveal tract (Iris/Iritis/, Ciliary body/Cyclitis/, and choroids/Chorioiditis/) Etiology • Toxoplasmosis • Herpes zoster and simplex virus • Candidiasis • Histoplasmosis • Tuberculosis • Syphilis Types 1. Non granulomatous 2. Granulomatous
- 84. 84 Clinical manifestation: for non granulomatous uveitis(the most common) • Acute onset • Pain • Photophobia • Conjunctival injection, especially around the cornea • Pupil will be small or irregular • Vision will be blurred • In severe case hypopyon- accumulation of pus in the anterior chamber • Repeated attack can cause anterior synechia- peripeheral iris adheres to the cornea and impeds outflow of aqueous humor or • Posterior synechia- adherence of the iris and lens
- 85. 85 Hypopyon
- 87. 87 Clinical manifestation: for granulomatous uveitis • Insidious onset • Vision is markedly and adversely affected • Conjunctival injection is diffuse • Vitreous clouding • Photophobia and pain is minimal Management • Mydraisis (pupil dilator)- for ciliary spasm and synechia • Cycloplegic medications- for paralysis of the iris sphincter • Local corticosteroid drops instilled 4 to 6 times a day to reduce inflammation • In severe cases, systemic corticosteroids intravenously • Wearing dark glass for the photophobia during out door stay
- 88. 88 Disease of the inner eye A. Panophthalmitis Panophthalmitis-is an inflammation of all the tissues of the eye ball Etiology • Bacteria • Virus • Fungus, etc On assessment • History of recent intraocular operation • Penetrating trauma • Common in immunocompromised patients: HIV/AIDS and diabetes Clinical manifestation • Severe pain • Loss of vision • Redness of the conjunctiva and the underlying episclera Management • Medications (antimicrobials + steroids) – Topical – Subconjunctival – Intravitreally – Systematically, or in a combination form • Surgery – Enucleation
- 89. 89 Injuries to the eye 1. Trauma to the eye A. Blunt contusion- bruising of periorbital soft tissue Clinical manifestation • Swelling and discoloration of the tissue • Bleeding into the tissue and structures of the eye • Pain Management • Reduce swelling and pain • Refer for ophthalmologist assessment
- 90. 90 B. Hyphema- presence of blood in the anterior chamber Clinical manifestation • Pain • Blood in the anterior chamber • Increased intraocular pressure Management • Usually spontaneously recovers • If severe bed rest, and eye shield application
- 91. 91 Hyphema
- 92. 92 C. Orbital fracture- fracture and dislocation of walls of the orbit, orbital margins, or both Clinical manifestation • May be accompanied by other signs of head injury • Rhinorrhea • Contusion • Diplopia Management • May heal by itself, if no displacement or infringement on other structure • Surgery/repair the orbital floor/
- 93. 93 D. Foreign body- on conjunctiva, cornea Clinical manifestation • Sever pain with lacrimation • Foreign body sensation • Photophobia • Redness • Swelling Management • Consider as medical emergency • Removal of foreign body through irrigation, cotton tipped applicator, magnet or needle tip • Surgical removal
- 94. 94 Foreign body
- 95. Foreign body: corneal, conjunctival, sub-tarsal and intraocular .
- 96. Removing a sub-tarsal foreign body
- 97. 97 Foreign body
- 99. Removing a corneal foreign body by needle tip
- 100. 100 E. Laceration/perforation- cutting or penetration of soft tissue Clinical manifestation • Pain • Bleeding • Lacrimation • Photophobia Management • Consider as medical emergency • Surgical repair-method of repair depends on the severity of injury • Antibiotics
- 103. 103 F. Ruptured globe-concussive injury to globe with tears in the ocular coats Clinical manifestation • Pain • Altered intraocular pressure • Limitation of gaze in field of rupture • Hyphema • Hemorrhage Management • Consider as medical emergency • Surgical repair • Antibiotics • Steroids • Enucleation
- 104. Hyphema
- 105. 105 2. Burn of the eye- is the destruction of eye tissue by chemical, thermal, and ultraviolet ray. • Determine the causative agent A.Burns of chemical agent that is caused by alkali or acids Clinical manifestation • Pain • Burning • Lacrimation • Photophobia Management • Consider as medical emergency • Copious irrigation until PH is 7 • Severe scarring may require keratoplasty • Antibiotics
- 106. 106 B. Burns of thermal sources Clinical manifestation • Pain • Burned skin • Blisters Management • First aid- apply sterile dressing • Pain control • Leave fluid blebs intact • Suture eye lids together to protect eye- if perforation is possible • Skin grafting with severe second and third degree burns
- 107. 107 C. Burns of ultraviolet source Clinical manifestation • Pain • Foreign body sensation • Lacrimation • Photophobia Management • Pain relief • Bilateral patching with antibiotic ointment and cycloplegics
- 108. 108 Other conditions of the eye 1. Glaucoma Glaucoma-is a pathological rise in the intraocular pressure, which damages various structures in the eye, especially the optic nerve There are four types of glaucoma A. Congenital glaucoma B. Closed angle glaucoma (acute glaucoma) C. Open angle glaucoma (chronic glaucoma) D. Secondary glaucoma A. Congenital glaucoma • Is a rare condition that occurs in infants and neonates Etiology • The angle of the anterior chamber does not develop normally in the embryo Clinical manifestations • The eye, and especially the diameter of the cornea, increases in size • The cornea becomes edematous
- 109. 109 Normal aqueous humor flow inside the eye
- 110. Normal aqueous humor flow
- 111. 111 Diagnostic evaluations • Increase in IOP Management Medical • Pilocarpine drops • Acetazolamide tablet Surgical • Goniotomy- to incise the mesodermal membrane in the angle of anterior chamber
- 112. 112 B. Closed angle glaucoma (acute glaucoma) • It accounts for 10% of glaucoma Etiology • Mechanical blockage of anterior chamber angle • Angle closure occurs because of the pupillary dilation or forward displacement of the iris • Results in accumulation of aqueous humor • Within several days, scar tissue forms between the iris and cornea, closing the angle. The iris and ciliary body begin to atrophy, the cornea degenerates because of edema, and the optic nerve begins to atrophy
- 113. POAG & ACG
- 115. 115 Pupilary dilation in glaucoma
- 116. 116 Glaucoma and the iris
- 117. 117 Glaucoma and the optic nerve disk
- 119. 119 Clinical manifestations • Severe pain in and around the eye • Nausea and vomiting • Pupil mid-dilated and fixed • Hazy appearing cornea due to corneal edema • Progressive visual field loss • It occurs suddenly with loss of vision • Sudden elevation of intra ocular pressure/IOP/ Diagnostic evaluations • Tonometery-IOP usually elevated
- 120. 120 Management Medical • Lower the IOP as quick as possible by medical means • Miotics-used to constrict the pupil and contract the ciliary muscle, thus the iris is drawn away from cornea; aqueous humor may drain through lymph spaces(meshwork) in to canal of schlemm E.g.: Pilocarpine drops 2%-4%- 1 drop every 5 minutes for an hour, and then every hour for 12 hours topically • Carbonic anhydrase inhibitor-restricts action of enzyme that is necessary to produce aqueous humor E.g.: Acetazolamide (Diamox) 250 mg 4 times a day orally • Hyperosmotic agents-reduces intraocular pressure by promoting diuresis E.g.: Mannitol intravenously Surgical • Iridectomy- excision of a small portion of the iris whereby aqueous humor can bypass pupil- this prevents the periphery of the iris blocking the angle of the anterior chamber • Trabeculectomy- partial thickness scleral resection with small part of trabecular meshwork removed and iridectomy • Laser iridotomy- multiple tiny laser incision to iris to create openings for aqueous flow
- 121. 121 Procedures of iridectomy Incision close to the limbus
- 124. 124 C. Open angle glaucoma (chronic glaucoma) • Makes up 90% of primary glaucoma cases • Its incidence increases with age Etiology • Degenerative changes occur in the trabecullar meshwork and canal of schlemm • This causes microscopic obstruction • Aqueous fluid can not emptied from the anterior chamber Risk factors • Age • Familial history of glaucoma • Diabetes • Hypertension Clinical manifestations • Mild, bilateral discomfort (tired feeling in eyes, foggy vision) • Slowly developing impairment of peripheral vision with dilated pupil • Progressive loss of visual field • No pain or inflammation
- 125. POAG & ACG
- 127. 127 Diagnostic tests • A rise in IOP • Optic nerve atrophy • Paleness of the optic disk Management Medical • Reduce the IOP by medication-the medication should be continued for the rest of patient’s life – Pilocarpine drops 2%-4% 4 times a day – Adrenaline drops 1% 2 times a day – Timolol/Timoptol/ drops 0.25%-0.5% 2 times a day Surgery – Iridencleisis- an opening is created between anterior chamber and space beneath the conjunctiva ; this by passes the blocked meshwork, and aqueous humor is absorbed in to conjunctival tissues – Cyclodiathermy/cyclocryotherapy- destruction of ciliary body with a high frequency electrical current or supercooled probe respectively
- 128. 128 A normal optic disc
- 130. 130 Early glaucomatous optic atrophy
- 131. 131 Advanced glaucomatous optic atrophy
- 133. 133 Procedures of iridencleisis Iris prolapsed through incision, and transected radially
- 135. 135 D. Secondary glaucoma-a type of glaucoma caused by a specific causes or pathologies Etiology • Hemorrhage • Corticosteroid use • Uveitis, etc Management • Treat the cause
- 136. 136 2. Diabetic retinopathy Diabetic retinopathy-is a complication of diabetes mellitus that affects the retinal blood vessels Etiology • Weakening of the walls of the micro blood vessels • Capillary dilation • Decreased capillary blood flow • Retina becomes ischemic and it stimulates the growth of new blood vessels Clinical manifestations • Complain of sudden, often severe loss of vision • Bleeding to the vitreous • Floaters Diagnostic evaluation • History • Ophthalmoscopic examination • Slit lamp microscopic examination Management • Photocoagulation-coagulation of the new blood vessels that bleeds • Proper control and expert management of the diabetes mellitus
- 137. 137 Normal fundus of white people
- 138. 138 Normal fundus of black people
- 140. 140 3. Strabismus Strabismus/Squint/- the two eyes are looking in different directions Etiology • Disorder of the vision • Disorder of the eye movements • Refractive errors Clinical manifestation • The corneal light reflex – This is the best and simplest test of squint – If the two eyes are straight, then the two corneal light reflexes are central and symmetrical, but if one eye squints, then the reflex deviates from the center of the cornea • Testing the ocular movements – There are six extra ocular muscles, and each one produces most of the movement in a particular direction
- 141. 141 Muscles of the eye
- 142. 142 Movement of the eye
- 143. 143 Effect of squint In adults • Double vision /diplopia/ • Abnormal head posture In children • Amblyopia /lazy eye/ Management • In children – Try to correct any refractive errors and amblyopia before straightening the squint surgically – Patching the good eye – Surgical correction by either weakening, strengthening or realigning the extra ocular muscles • In adults – Cosmetic surgery is the only treatment
- 144. 144 Muscle movement • Medial rectus (MR) – Moves the eye inward, towards the nose (adduction) • Lateral rectus (LR) – Moves the eye outward, away from the nose (abduction) • Superior rectus (SR) – Primarily moves the eye upward (elevation) – Secondarily rotates the top of the eye toward the nose (intorsion) – Tertiarily moves the eye inward (adduction) • Inferior rectus (IR) – Primarily moves the eye downward (depression) – Secondarily rotates the top of the eye away from the nose (extorsion) – Tertiarily moves the eye inward (adduction) • Superior oblique (SO) – Primarily rotates the top of the eye toward the nose (intorsion) – Secondarily moves the eye downward (depression) – Tertiarily moves the eye outward (abduction) • Inferior oblique (IO) – Primarily rotates the top of the eye away from the nose (extorsion) – Secondarily moves the eye upward (elevation) – Tertiarily moves the eye outward (abduction)
- 145. 145 Position of the eye and the muscles
- 146. 146 4. Detachment of the retina Retinal detachment is a separation of the sensory retina and the underlying pigment epithelium with fluid accumulation between the two layers Etiology • Degenerative changes in the retina that occurs in aging • Trauma, inflammation, or tumor • Diabetic retinopathy • Occurs most commonly in patients older than age 40 Clinical manifestations • Painless loss of peripheral or central vision • Photopsia- light flashes • Blurred vision • The patient notes sensation of particles moving-floaters • A sensation of a veil like coating coming down, coming up, or coming sideways in front of the eye: is often misinterpreted as a drooping eyelid or elevated cheek
- 148. 148 Floaters
- 149. 149 Diagnostic method • Visual acuity measurement • Ophthalmoscopic examination • Slit lamp microscopic examination Management • Sedation, bed rest, and eye patch • Surgery – Photocoagulation-a light beam is passed through the pupil, causing a small burn and producing an exudates between the pigment epithelium and retina – Electrodiatermy- an electrode needle is passed through the sclera to allow subretinal fluid to escape. An exudates forms from the pigment epithelium and adheres to the retina – Cryosurgery/retinal cryopexy- a supercooled probe is touched to the sclera, causing minimal damage; as a result of scarring, the pigment epithelium adheres to the retina
- 150. 150 5. Vitamin “A” deficiency Vitamin “A” deficiency- a disorder of the eye caused by a deficiency of vitamin “A” Clinical manifestation • Night blindness • Conjuctival xerosis/Xerophthalmia/- dry and wrinkled appearance of the conjunctiva • Bitoti’s spots- a small plaque/spot of material on the surface of the bulbar conjunctiva • Corneal xerosis-dried and lusterless appearance of the cornea • Corneal ulceration/Keratomalacia/- part or the whole cornea melts away • Corneal scaring-the healed state of the cornea
- 151. 151 Conjunctival xerosis- dry and wrinkled appearance of the conjunctiva
- 152. 152 Bitoti’s spot- a small plaque/spot of material on the surface of the bulbar conjunctiva
- 153. 153 Corneal xerosis- dried and lusterless appearance of the cornea
- 154. 154 Corneal xerosis with ulceration
- 155. 155 Corneal and conjunctival xerosis
- 156. 156 A large superficial ulcer stained with fluorescein
- 157. 157 Corneal ulceration/Keratomalacia/- part or the whole cornea melts away
- 158. 158 Corneal scaring-the healed state of the cornea
- 159. 159 Management • Vitamin “A”(Retinol/Carotene) –<6 months of age------50,000 IU –>6 months of age------100,000 IU –>12 months of age-----200,000 IU –Next day------------------same age specific dose –At least 2 weeks later-same age specific dose –Women of reproductive age group with night blindness or Bitoti’s spots should receive daily doses of < 25,000 IU weekly
- 160. 160 6. Onchocerciasis Onchocerciasis- a disease caused by infestation with filarial of the genus onchocerca • The disease affects the eye, skin, and lymph node • Is the second leading cause of infectious blindness worldwide Etiology • Infection in humans begins with the deposition of infective larvae on the skin by the bite of an infected black fly • The black fly vector breeds along free flowing rivers and streams • Both biting and disease transmission are most intense in these locations
- 161. 161 Clinical manifestations • Early findings are conjunctivitis with photophobia • Snowflakes/white-grey spots-due to a reaction to the dead microfilariae • Sclerosing keratitis- opacity of the cornea • Corneal opacities • Anterior uveal tract deformity may cause secondary glaucoma
- 164. 164 More advanced sclerosing keratitis
- 165. 165 Diagnosis • Skin snip • Presence of microfilaria in the anterior chamber of the eye
- 166. 166 Management • Ivermectin single dose of 150µg/kg either yearly or semiannually • Vector control • Community based administration of ivermectin every 6 to 12 months- for endemic area • Wearing cloths which covers most of the skin surface