1 merged documents
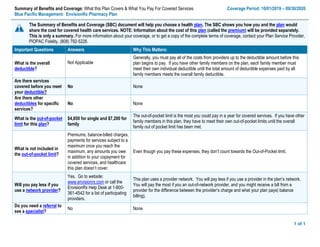
- 1. Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services Coverage Period: 10/01/2019 – 09/30/2020 Blue Pacific Management: EnvisionRx Pharmacy Plan 1 of 1 The Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, contact your Plan Service Provider, PIOPAC Fidelity, (808) 792-5226. Important Questions Answers Why This Matters: What is the overall deductible? Not Applicable Generally, you must pay all of the costs from providers up to the deductible amount before this plan begins to pay. If you have other family members on the plan, each family member must meet their own individual deductible until the total amount of deductible expenses paid by all family members meets the overall family deductible. Are there services covered before you meet your deductible? No None Are there other deductibles for specific services? No None What is the out-of-pocket limit for this plan? $4,850 for single and $7,200 for family The out-of-pocket limit is the most you could pay in a year for covered services. If you have other family members in this plan, they have to meet their own out-of-pocket limits until the overall family out of pocket limit has been met. What is not included in the out-of-pocket limit? Premiums, balance-billed charges, payments for services subject to a maximum once you reach the maximum, any amounts you owe in addition to your copayment for covered services, and healthcare this plan doesn’t cover. Even though you pay these expenses, they don’t count towards the Out-of-Pocket limit. Will you pay less if you use a network provider? Yes. Go to website: www.envisionrx.com or call the EnvisionRx Help Desk at 1-800- 361-4542 for a list of participating providers. This plan uses a provider network. You will pay less if you use a provider in the plan’s network. You will pay the most if you an out-of-network provider, and you might receive a bill from a provider for the difference between the provider’s charge and what your plan pays) balance billing). Do you need a referral to see a specialist? No None
- 2. 2 of 2Questions: 1-808-792-5226 If you are not clear about any of the underlined terms used in this form, call PIOPAC Fidelity, your Plan Service Provider. All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical/Rx Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) If you visit a health care provider’s office or clinic Primary care visit to treat an injury or illness Not Applicable Not Applicable None Specialist visit Not Applicable Not Applicable None Preventive care/screening/ immunization Not Applicable Not Applicable None If you have a test Diagnostic test (x-ray, blood work) Not Applicable Not Applicable None Imaging (CT/PET scans, MRIs) Not Applicable Not Applicable None If you need drugs to treat your illness or condition More information about prescription drug coverage is available at www.envisionrx.com Generic drugs $7 copay Not Applicable Covers up to a 30-day supply Preferred brand drugs $20 copay Not Applicable Covers up to a 30-day supply Non-preferred brand drugs $40 copay Not Applicable Covers up to a 30-day supply Diabetic Supplies $0 Not Applicable Applies only to Generic and Preferred Brand Diabetic Supplies Specialty drugs 30% Not Applicable All Specialty drugs are excluded from coverage including Self- Administered Injectables (excluding Insulin), fertility agents, growth Hormones and Hemophilia Factors EXCEPT FOR THE LISTED MEDICATIONS LISTED BELOW under Specialty Drugs covered with Prior Authorization. Covers up to a 30-day supply 90 Day Retail and Envision Mail Order For Maintenance Medication Pay for 2, get 1 Free Not Applicable Covers up to a 90-day supply Copay Exception Coinsurance applies if drug cost is over $150 for 30 DS or $450 for 90 DS If the copay is $0.00, the 20% coinsurance does not apply 20% coinsurance Not Applicable Formulary Exclusions Mandatory Generic Substitution Preferred Brand or Non- Preferred Brand Drugs Brand Name Copayment will apply Not Applicable If a brand name drug is dispensed when a generic equivalent is available, the brand
- 3. 3 of 3Questions: 1-808-792-5226 If you are not clear about any of the underlined terms used in this form, call PIOPAC Fidelity, your Plan Service Provider. Common Medical/Rx Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) name copayment will Apply PLUS the difference in cost between the Brand Name drug and the generic equivalent. Drug Quantity Management Envision Standard Refer to (If you need drugs to treat your illness or condition Not Applicable EnvisionRx Standard Formulary is a reference tool for identifying preferred medication within certain therapeutic categories Formulary 2018 Select Formulary Refer to (If you need drugs to treat your illness or condition) Not Applicable The drug list (formulary) that is the core of your prescription drug benefit plan. For complete formulary drug information visit www.envisionrx.com Step Therapy If you require a medication that is not on the EnvisionRx formulary and you cannot use a formulary alternative, you have the right to a coverage determination Prior-authorization Prior-authorization PPI, CoxII Inhibitor, Antidepressant, Insomnia Agents, ADD, Gout, Angiotensin Receptor Blocker, Cholesterol, Statins, Serotonin and Norepinephrine Inhibitors, Duexis, Vimovo Prior Authorization Custom List Not Applicable Not Applicable Formulary Exclusions Envision Specialty Specialty Drugs 30% Prior Authorization Specialty Drugs are classified as high cost, high complexity, specialty drugs are often injectable or infused If you have outpatient surgery Facility fee (e.g., ambulatory surgery center) Not Applicable Not Applicable None Physician/surgeon fees Not Applicable Not Applicable None If you need immediate medical attention Emergency room care Not Applicable Not Applicable None Emergency medical transportation Not Applicable Not Applicable None Urgent care Not Applicable Not Applicable None If you have a hospital stay Facility fee (e.g., hospital room) Not Applicable Not Applicable None Physician/surgeon fees Not Applicable Not Applicable None
- 4. 4 of 4Questions: 1-808-792-5226 If you are not clear about any of the underlined terms used in this form, call PIOPAC Fidelity, your Plan Service Provider. Common Medical/Rx Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) If you need mental health, behavioral health, or substance abuse services Outpatient services Not Applicable Not Applicable None Inpatient services Not Applicable Not Applicable None If you are pregnant Office visits Not Applicable Not Applicable None Childbirth/delivery professional services Not Applicable Not Applicable None Childbirth/delivery facility services Not Applicable Not Applicable None If you need help recovering or have other special health needs Home health care Not Applicable Not Applicable None Rehabilitation services Not Applicable Not Applicable None Habilitation services Not Applicable Not Applicable None Skilled nursing care Not Applicable Not Applicable None Durable medical equipment Not Applicable Not Applicable None Hospice services Not Applicable Not Applicable None If your child needs dental or eye care Children’s eye exam Not Applicable Not Applicable None Children’s glasses Not Applicable Not Applicable None Children’s dental check-up Not Applicable Not Applicable None Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: Other coverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call 1-800-318-2596. Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called a grievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents also provide complete information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance, contact: Blue Pacific Management Human Resources Department, 808-457-1871 or cwong@bluepacific.com. Does this plan provide Minimum Essential Coverage? Yes If you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for an exemption from the requirement that you have health coverage for that month. Does this plan meet the Minimum Value Standards? Yes If your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace.
- 5.
- 7. * = Annual Deductible Applies | % = Coinsurance (Percentage based on eligible charge) | $ = Copayment (Fixed dollar amount) Phone 591-0088 • Fax 591-0463 • Toll-Free 800-621-6998 • www.hmaa.com • Customer Service 941-4622 • Toll-Free 888-941-4622 00 ANNU COMP E-44-2 010119 DEDUCTIBLE APPLIES Plan Pays: Comprehensive Plus Medical Plan Schedule of Benefits Annual Deductible $100 per person / $300 maximum per family Stop Loss $2,000 per person / $6,000 per family (per calendar year, includes deductibles & copayments) Lifetime Maximum Unlimited Benefit Coinsurance/Copayment Participating Non-Participating Hospital and Facility Services Ambulatory Surgical Center (ASC) 20% 20% Hospital Ancillary Services 20% 20% Hospital Room and Board 20% 20% Outpatient Facility 20% 20% Skilled Nursing Facility 20% 20% Emergency Services Emergency Room 20% 20% Physician Visits $15 $15 Online Care and Telephonic Services None Not Covered Physician Services Physician Visits $15 $15 Hospital Visits $15 $15 Immunizations (standard, including travel) None None Testing, Laboratory and Radiology Allergy Testing 20%* 20%* Allergy Treatment Materials $5 $5 Diagnostic Testing 20% 20% Laboratory and Pathology — Inpatient 20% 20% Outpatient None None Radiology 20% 20% Chemotherapy and Radiation Therapy Chemotherapy — Infusion/Injections 20%* 20%* Radiation Therapy — Inpatient Inpatient 20%* 20%* Outpatient Inpatient 20% 20% Other Medical Services and Supplies Acupuncture, Chiropractic and Naturopathic Services 20% 20% Ambulance (air) 20%* 20%* Ambulance (ground) 20% 20% Blood and Blood Products 20%* 20%* Dialysis and Supplies 20%* 20%* Durable Medical Equipment and Supplies 20%* 20%* Evaluations for Hearing Aids 20%* 20%* Growth Hormone Therapy 20% 20% Home IV Therapy 20% 20% Inhalation Therapy 20% 20% Injections 20%* 20%* Medical Foods 20% 20% Orthotics and External Prosthetics 20%* 20%* Vision and Hearing Appliances 20%* 20%*
- 8. * = Annual Deductible Applies | % = Coinsurance (Percentage based on eligible charge) | $ = Copayment (Fixed dollar amount) Note: Reimbursement is based on a percentage of HMAA’s eligible charges, not the billed charges. Eligible charges may be based on a procedure fee schedule, a percentage of billed charges, per day (per diem) fees, per case fees, per treatment fees, or other methods. This document is intended to provide a condensed explanation of benefits. Please refer to the Description of Coverage (DOC) for details. In the case of a discrepancy between this document and the language contained within the DOC, the latter will take precedence. Benefit Coinsurance/Copayment Participating Non-Participating Rehabilitation Therapy Physical and Occupational Therapy InpatientInpatient 20% 20% Outpatient 20%* 20%* Speech Therapy Services — Inpatient 20% 20% Outpatient 20%* 20%* Special Benefits – Disease Management and Preventive Services Disease Management None Not covered Preventive Services — Laboratory None None Preventive Services — Physical Exam None None Screening and Preventive Counseling None None Special Benefits for Children Newborn Care 10% 10% Well Child Care Immunizations None None Well Child Care Laboratory Tests None None Well Child Care Physician Office Visits None None Special Benefits for Men Prostate Specific Antigen Test (screening) None None Special Benefits for Women Breast Pump None None Chlamydia Screening None None Contraceptive Implants (generic) None None Contraceptive lnjectables (generic) None None Contraceptive IUD (generic) None None In Vitro Fertilization 20%* 20%* Mammography (screening) None None Maternity Care 10% 10% Pap Smears (screening) None None Tubal Ligation None None Well Woman Exam None None Special Benefits for Homebound, Terminal, or Long-Term Care Home Health Care 20% 20% Hospice Services None None Behavioral Health – Mental Health and Substance Abuse Hospital and Facility Services 20% 20% Physician Services — Inpatient None None Outpatient $15 $15 Psychological Testing 20% 20% Special Offers Employee Assistance Program (EAP) Up to 6 fully-covered visits to assist subscribers with personal or family issues Health and Wellness Programs A variety of solutions for healthy living including Active&Fit® , Flu Prevention, Colorectal Cancer Screening, Maternity & Baby Care Incentive Program, and more Member Plus Discount Program Discounted prices and special offers from HMAA member groups and other participating merchants The Active&Fit and Active&Fit Direct programs are provided by American Specialty Health Fitness, Inc., a subsidiary of American Specialty Health Incorporated (ASH). Active&Fit Direct, Active&Fit Connected!, Active&Fit, and the Active&Fit Direct logos are trademarks of ASH and used with permission herein.
- 9. Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services Coverage Period: Beginning on or after 01/01/2019 Hawaii Medical Assurance Association: Comprehensive Plus Coverage for: Single/Two-Party/Family | Plan Type: PPO 1 of 6 COMP E-33 010119 (CompPlus) The Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, visit www.hmaa.com or call 1-888-941-4622. For general definitions of common terms, such as allowed amount, balance billing, coinsurance, copayment, deductible, provider, or other underlined terms see the Glossary. You can view the Glossary at www.hmaa.com or call 1-888-941-4622 to request a copy. Important Questions Answers Why This Matters: What is the overall deductible? $100/Individual or $300/family Generally, you must pay all of the costs from providers up to the deductible amount before this plan begins to pay. If you have other family members on the plan, each family member must meet their own individual deductible until the total amount of deductible expenses paid by all family members meets the overall family deductible. Are there services covered before you meet your deductible? Yes. Preventive care, primary care services, contraceptives, emergency services, prescription drug and supplies and well-child care services are covered before you meet your deductible. This plan covers some items and services even if you haven’t yet met the deductible amount. But a copayment or coinsurance may apply. For example, this plan covers certain preventive services without cost-sharing and before you meet your deductible. See a list of covered preventive services at https://www.healthcare.gov/coverage/preventive-care-benefits/. Are there other deductibles for specific services? No. You don’t have to meet deductibles for specific services. What is the out-of-pocket limit for this plan? $2,000/Individual or $6,000/family The out-of-pocket limit is the most you could pay in a year for covered services. If you have other family members in this plan, they have to meet their own out-of-pocket limits until the overall family out-of-pocket limit has been met. What is not included in the out-of-pocket limit? Copayments and coinsurance for certain services, premiums, balance-billing charges, and health care this plan doesn’t cover. Even though you pay these expenses, they do not count toward the out–of–pocket limit. Will you pay less if you use a network provider? Yes. See www.hmaa.com or call 1-888-941-4622 for a list of network providers. This plan uses a provider network. You will pay less if you use a provider in the plan’s network. You will pay the most if you use an out-of-network provider, and you might receive a bill from a provider for the difference between the provider’s charge and what your plan pays (balance billing). Be aware, your network provider might use an out-of-network provider for some services (such as lab work). Check with your provider before you get services. Do you need a referral to see a specialist? No. You can see the specialist you choose without a referral. OMB Control Numbers 1545‐2229, 1210‐0147, and 0938‐1146 Released on April 6, 2016
- 10. 2 of 6 COMP E-33 010119 (CompPlus) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) If you visit a health care provider’s office or clinic Primary care visit to treat an injury or illness $15 copay/office visit; deductible does not apply $15 copay/office visit; deductible does not apply None Specialist visit $15 copay/office visit; deductible does not apply $15 copay/office visit; deductible does not apply Preventive care/screening/ immunization No charge No charge Age and frequency limitations may apply. You may have to pay for services that aren’t preventive. Ask your provider if the services you need are preventive. Then check what your plan will pay for. If you have a test Diagnostic test (x-ray, blood work) 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply NoneNo charge No charge Imaging (CT/PET scans, MRIs) 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply If you need drugs to treat your illness or condition More information about prescription drug coverage is available at www.hmaa.com Generic drugs No charge No charge Coverage limited to diabetic drugs and diabetic supplies for all members. Contraceptives covered for women only. Only preferred brand named diabetic supplies are covered at no charge. Generic diabetic drugs and non-preferred brand named diabetic drugs and supplies have a 20% coinsurance. Diaphragms, cervical caps and generic contraceptives for women are covered at no charge when using a network provider. Preferred brand drugs 20% coinsurance 20% coinsurance Non-preferred brand drugs 20% coinsurance 20% coinsurance Specialty drugs No charge No charge Coverage for specialty drugs limited to oral chemotherapy only. If you have outpatient surgery Facility fee (e.g., ambulatory surgery center) 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply None
- 11. 3 of 6 COMP E-33 010119 (CompPlus) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) Physician/surgeon fees $15 copay; deductible does not apply $15 copay; deductible does not apply If you need immediate medical attention Emergency room care 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply None Emergency medical transportation 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Coverage for air transportation is limited to the United States and the deductible applies. Urgent care $25 copay; deductible does not apply $25 copay; deductible does not apply None If you have a hospital stay Facility fee (e.g., hospital room) 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Physician/surgeon fees $15 copay; deductible does not apply $15 copay; deductible does not apply None If you need mental health, behavioral health, or substance abuse services Outpatient services 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply None Inpatient services 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Preauthorization is required. If you don't get preauthorization, benefits could be reduced. If you are pregnant Office visits 10% coinsurance; deductible does not apply 10% coinsurance; deductible does not apply None Childbirth/delivery professional services 10% coinsurance; deductible does not apply 10% coinsurance; deductible does not apply Childbirth/delivery facility services 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply If you need help recovering or have other special health needs Home health care 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Coverage limited to 150 days per calendar year. Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Rehabilitation services Inpatient: 20% coinsurance; deductible does not apply Inpatient: 20% coinsurance; deductible does not apply Preauthorization is required for inpatient services. If you don't get preauthorization, benefits could be reduced.Outpatient: 20% coinsurance Outpatient: 20% coinsurance Habilitation services Not covered Not covered None
- 12. 4 of 6 COMP E-33 010119 (CompPlus) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) Skilled nursing care 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Coverage limited to 120 days in any calendar year. Durable medical equipment 20% coinsurance 20% coinsurance Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Hospice services No Charge No Charge None If your child needs dental or eye care Children’s eye exam Not covered Not covered None Children’s glasses Not covered Not covered None Children’s dental check-up Not covered Not covered None Excluded Services & Other Covered Services: Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Cosmetic surgery Dental care (Adult) Long-term care Non-emergency care when traveling outside the U.S. Private-duty nursing Routine eye care (Adult) Routine foot care Weight loss programs Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Acupuncture Bariatric surgery Chiropractic care Hearing aids Infertility treatment Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: HMAA at (888) 941-4622 or CustomerService@hmaa.com, or the Department of Labor’s Employee Benefits Security Administration at 1-866-444-EBSA (3272) or www.dol.gov/ebsa/healthreform. Other coverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call 1-800-318-2596. Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called a grievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents also provide complete information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance, contact: HMAA at (888) 941-
- 13. 5 of 6 COMP E-33 010119 (CompPlus) 4622 or CustomerService@hmaa.com, or the Hawaii Insurance Division, ATTN: Health Insurance Branch – External Appeals, 335 Merchant Street, Room 213, Honolulu, HI 96813 at (808) 586-2804 or the Department of Labor Employment Benefits Security Administration at 1-866-444-EBSA (3272) or www.dol.gov/ebsa/healthreform. Does this plan provide Minimum Essential Coverage? Yes. If you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for an exemption from the requirement that you have health coverage for that month. Does this plan meet the Minimum Value Standards? Yes. If your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace. Language Access Services: Spanish (Español): Para obtener asistencia en Español, llame al 1-888-941-4622. Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 1-888-941-4622. Chinese (中文): 如果需要中文的帮助,请拨打这个号码 1-888-941-4622. Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' 1-888-941-4622. ––––––––––––––––––––––To see examples of how this plan might cover costs for a sample medical situation, see the next section.––––––––––––––––––––––
- 14. 6 of 6 The plan would be responsible for the other costs of these EXAMPLE covered services. Peg is Having a Baby (9 months of in-network pre-natal care and a hospital delivery) Mia’s Simple Fracture (in-network emergency room visit and follow up care) Managing Joe’s type 2 Diabetes (a year of routine in-network care of a well- controlled condition) The plan’s overall deductible $100 Specialist copayment $15 Hospital (facility) coinsurance 20% Other coinsurance 20% This EXAMPLE event includes services like: Specialist office visits (prenatal care) Childbirth/Delivery Professional Services Childbirth/Delivery Facility Services Diagnostic tests (ultrasounds and blood work) Specialist visit (anesthesia) Total Example Cost $12,800 In this example, Peg would pay: Cost Sharing Deductibles $0 Copayments $0 Coinsurance $2,000 What isn’t covered Limits or exclusions $60 The total Peg would pay is $2,060 The plan’s overall deductible $100 Specialist copayment $15 Hospital (facility) coinsurance 20% Other coinsurance 20% This EXAMPLE event includes services like: Primary care physician office visits (including disease education) Diagnostic tests (blood work) Prescription drugs Durable medical equipment (glucose meter) Total Example Cost $7,400 In this example, Joe would pay: Cost Sharing Deductibles $100 Copayments $150 Coinsurance $1,089 What isn’t covered Limits or exclusions $55 The total Joe would pay is $1,394 The plan’s overall deductible $100 Specialist copayment $15 Hospital (facility) coinsurance 20% Other coinsurance 20% This EXAMPLE event includes services like: Emergency room care (including medical supplies) Diagnostic test (x-ray) Durable medical equipment (crutches) Rehabilitation services (physical therapy) Total Example Cost $1,900 In this example, Mia would pay: Cost Sharing Deductibles $100 Copayments $45 Coinsurance $326 What isn’t covered Limits or exclusions $0 The total Mia would pay is $471 About these Coverage Examples: This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost sharing amounts (deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion of costs you might pay under different health plans. Please note these coverage examples are based on self-only coverage.
- 15. Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services Coverage Period: Beginning on or after 01/01/2019 Hawaii Medical Assurance Association: Comprehensive Plus Coverage for: Single/Two-Party/Family | Plan Type: PPO 1 of 6 COMP E-33 010119 (CompPlus) The Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, visit www.hmaa.com or call 1-888-941-4622. For general definitions of common terms, such as allowed amount, balance billing, coinsurance, copayment, deductible, provider, or other underlined terms see the Glossary. You can view the Glossary at www.hmaa.com or call 1-888-941-4622 to request a copy. Important Questions Answers Why This Matters: What is the overall deductible? $100/Individual or $300/family Generally, you must pay all of the costs from providers up to the deductible amount before this plan begins to pay. If you have other family members on the plan, each family member must meet their own individual deductible until the total amount of deductible expenses paid by all family members meets the overall family deductible. Are there services covered before you meet your deductible? Yes. Preventive care, primary care services, contraceptives, emergency services, prescription drug and supplies and well-child care services are covered before you meet your deductible. This plan covers some items and services even if you haven’t yet met the deductible amount. But a copayment or coinsurance may apply. For example, this plan covers certain preventive services without cost-sharing and before you meet your deductible. See a list of covered preventive services at https://www.healthcare.gov/coverage/preventive-care-benefits/. Are there other deductibles for specific services? No. You don’t have to meet deductibles for specific services. What is the out-of-pocket limit for this plan? $2,000/Individual or $6,000/family The out-of-pocket limit is the most you could pay in a year for covered services. If you have other family members in this plan, they have to meet their own out-of-pocket limits until the overall family out-of-pocket limit has been met. What is not included in the out-of-pocket limit? Copayments and coinsurance for certain services, premiums, balance-billing charges, and health care this plan doesn’t cover. Even though you pay these expenses, they do not count toward the out–of–pocket limit. Will you pay less if you use a network provider? Yes. See www.hmaa.com or call 1-888-941-4622 for a list of network providers. This plan uses a provider network. You will pay less if you use a provider in the plan’s network. You will pay the most if you use an out-of-network provider, and you might receive a bill from a provider for the difference between the provider’s charge and what your plan pays (balance billing). Be aware, your network provider might use an out-of-network provider for some services (such as lab work). Check with your provider before you get services. Do you need a referral to see a specialist? No. You can see the specialist you choose without a referral. OMB Control Numbers 1545‐2229, 1210‐0147, and 0938‐1146 Released on April 6, 2016
- 16. 2 of 6 COMP E-33 010119 (CompPlus) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) If you visit a health care provider’s office or clinic Primary care visit to treat an injury or illness $15 copay/office visit; deductible does not apply $15 copay/office visit; deductible does not apply None Specialist visit $15 copay/office visit; deductible does not apply $15 copay/office visit; deductible does not apply Preventive care/screening/ immunization No charge No charge Age and frequency limitations may apply. You may have to pay for services that aren’t preventive. Ask your provider if the services you need are preventive. Then check what your plan will pay for. If you have a test Diagnostic test (x-ray, blood work) 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply NoneNo charge No charge Imaging (CT/PET scans, MRIs) 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply If you need drugs to treat your illness or condition More information about prescription drug coverage is available at www.hmaa.com Generic drugs No charge No charge Coverage limited to diabetic drugs and diabetic supplies for all members. Contraceptives covered for women only. Only preferred brand named diabetic supplies are covered at no charge. Generic diabetic drugs and non-preferred brand named diabetic drugs and supplies have a 20% coinsurance. Diaphragms, cervical caps and generic contraceptives for women are covered at no charge when using a network provider. Preferred brand drugs 20% coinsurance 20% coinsurance Non-preferred brand drugs 20% coinsurance 20% coinsurance Specialty drugs No charge No charge Coverage for specialty drugs limited to oral chemotherapy only. If you have outpatient surgery Facility fee (e.g., ambulatory surgery center) 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply None
- 17. 3 of 6 COMP E-33 010119 (CompPlus) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) Physician/surgeon fees $15 copay; deductible does not apply $15 copay; deductible does not apply If you need immediate medical attention Emergency room care 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply None Emergency medical transportation 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Coverage for air transportation is limited to the United States and the deductible applies. Urgent care $25 copay; deductible does not apply $25 copay; deductible does not apply None If you have a hospital stay Facility fee (e.g., hospital room) 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Physician/surgeon fees $15 copay; deductible does not apply $15 copay; deductible does not apply None If you need mental health, behavioral health, or substance abuse services Outpatient services 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply None Inpatient services 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Preauthorization is required. If you don't get preauthorization, benefits could be reduced. If you are pregnant Office visits 10% coinsurance; deductible does not apply 10% coinsurance; deductible does not apply None Childbirth/delivery professional services 10% coinsurance; deductible does not apply 10% coinsurance; deductible does not apply Childbirth/delivery facility services 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply If you need help recovering or have other special health needs Home health care 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Coverage limited to 150 days per calendar year. Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Rehabilitation services Inpatient: 20% coinsurance; deductible does not apply Inpatient: 20% coinsurance; deductible does not apply Preauthorization is required for inpatient services. If you don't get preauthorization, benefits could be reduced.Outpatient: 20% coinsurance Outpatient: 20% coinsurance Habilitation services Not covered Not covered None
- 18. 4 of 6 COMP E-33 010119 (CompPlus) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) Skilled nursing care 20% coinsurance; deductible does not apply 20% coinsurance; deductible does not apply Coverage limited to 120 days in any calendar year. Durable medical equipment 20% coinsurance 20% coinsurance Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Hospice services No Charge No Charge None If your child needs dental or eye care Children’s eye exam Not covered Not covered None Children’s glasses Not covered Not covered None Children’s dental check-up Not covered Not covered None Excluded Services & Other Covered Services: Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Cosmetic surgery Dental care (Adult) Long-term care Non-emergency care when traveling outside the U.S. Private-duty nursing Routine eye care (Adult) Routine foot care Weight loss programs Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Acupuncture Bariatric surgery Chiropractic care Hearing aids Infertility treatment Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: HMAA at (888) 941-4622 or CustomerService@hmaa.com, or the Department of Labor’s Employee Benefits Security Administration at 1-866-444-EBSA (3272) or www.dol.gov/ebsa/healthreform. Other coverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call 1-800-318-2596. Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called a grievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents also provide complete information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance, contact: HMAA at (888) 941-
- 19. 5 of 6 COMP E-33 010119 (CompPlus) 4622 or CustomerService@hmaa.com, or the Hawaii Insurance Division, ATTN: Health Insurance Branch – External Appeals, 335 Merchant Street, Room 213, Honolulu, HI 96813 at (808) 586-2804 or the Department of Labor Employment Benefits Security Administration at 1-866-444-EBSA (3272) or www.dol.gov/ebsa/healthreform. Does this plan provide Minimum Essential Coverage? Yes. If you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for an exemption from the requirement that you have health coverage for that month. Does this plan meet the Minimum Value Standards? Yes. If your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace. Language Access Services: Spanish (Español): Para obtener asistencia en Español, llame al 1-888-941-4622. Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 1-888-941-4622. Chinese (中文): 如果需要中文的帮助,请拨打这个号码 1-888-941-4622. Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' 1-888-941-4622. ––––––––––––––––––––––To see examples of how this plan might cover costs for a sample medical situation, see the next section.––––––––––––––––––––––
- 20. 6 of 6 The plan would be responsible for the other costs of these EXAMPLE covered services. Peg is Having a Baby (9 months of in-network pre-natal care and a hospital delivery) Mia’s Simple Fracture (in-network emergency room visit and follow up care) Managing Joe’s type 2 Diabetes (a year of routine in-network care of a well- controlled condition) The plan’s overall deductible $100 Specialist copayment $15 Hospital (facility) coinsurance 20% Other coinsurance 20% This EXAMPLE event includes services like: Specialist office visits (prenatal care) Childbirth/Delivery Professional Services Childbirth/Delivery Facility Services Diagnostic tests (ultrasounds and blood work) Specialist visit (anesthesia) Total Example Cost $12,800 In this example, Peg would pay: Cost Sharing Deductibles $0 Copayments $0 Coinsurance $2,000 What isn’t covered Limits or exclusions $60 The total Peg would pay is $2,060 The plan’s overall deductible $100 Specialist copayment $15 Hospital (facility) coinsurance 20% Other coinsurance 20% This EXAMPLE event includes services like: Primary care physician office visits (including disease education) Diagnostic tests (blood work) Prescription drugs Durable medical equipment (glucose meter) Total Example Cost $7,400 In this example, Joe would pay: Cost Sharing Deductibles $100 Copayments $150 Coinsurance $1,089 What isn’t covered Limits or exclusions $55 The total Joe would pay is $1,394 The plan’s overall deductible $100 Specialist copayment $15 Hospital (facility) coinsurance 20% Other coinsurance 20% This EXAMPLE event includes services like: Emergency room care (including medical supplies) Diagnostic test (x-ray) Durable medical equipment (crutches) Rehabilitation services (physical therapy) Total Example Cost $1,900 In this example, Mia would pay: Cost Sharing Deductibles $100 Copayments $45 Coinsurance $326 What isn’t covered Limits or exclusions $0 The total Mia would pay is $471 About these Coverage Examples: This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost sharing amounts (deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion of costs you might pay under different health plans. Please note these coverage examples are based on self-only coverage.
- 21. * = Annual Deductible Applies | % = Coinsurance (Percentage based on eligible charge) | $ = Copayment (Fixed dollar amount) Phone 591-0088 • Fax 591-0463 • Toll-Free 800-621-6998 • www.hmaa.com • Customer Service 941-4622 • Toll-Free 888-941-4622 00 ANNU COMP E-44-2 010119 DEDUCTIBLE APPLIES Plan Pays: Comprehensive Plus Medical Plan Schedule of Benefits Annual Deductible $100 per person / $300 maximum per family Stop Loss $2,000 per person / $6,000 per family (per calendar year, includes deductibles & copayments) Lifetime Maximum Unlimited Benefit Coinsurance/Copayment Participating Non-Participating Hospital and Facility Services Ambulatory Surgical Center (ASC) 20% 20% Hospital Ancillary Services 20% 20% Hospital Room and Board 20% 20% Outpatient Facility 20% 20% Skilled Nursing Facility 20% 20% Emergency Services Emergency Room 20% 20% Physician Visits $15 $15 Online Care and Telephonic Services None Not Covered Physician Services Physician Visits $15 $15 Hospital Visits $15 $15 Immunizations (standard, including travel) None None Testing, Laboratory and Radiology Allergy Testing 20%* 20%* Allergy Treatment Materials $5 $5 Diagnostic Testing 20% 20% Laboratory and Pathology — Inpatient 20% 20% Outpatient None None Radiology 20% 20% Chemotherapy and Radiation Therapy Chemotherapy — Infusion/Injections 20%* 20%* Radiation Therapy — Inpatient Inpatient 20%* 20%* Outpatient Inpatient 20% 20% Other Medical Services and Supplies Acupuncture, Chiropractic and Naturopathic Services 20% 20% Ambulance (air) 20%* 20%* Ambulance (ground) 20% 20% Blood and Blood Products 20%* 20%* Dialysis and Supplies 20%* 20%* Durable Medical Equipment and Supplies 20%* 20%* Evaluations for Hearing Aids 20%* 20%* Growth Hormone Therapy 20% 20% Home IV Therapy 20% 20% Inhalation Therapy 20% 20% Injections 20%* 20%* Medical Foods 20% 20% Orthotics and External Prosthetics 20%* 20%* Vision and Hearing Appliances 20%* 20%*
- 22. * = Annual Deductible Applies | % = Coinsurance (Percentage based on eligible charge) | $ = Copayment (Fixed dollar amount) Note: Reimbursement is based on a percentage of HMAA’s eligible charges, not the billed charges. Eligible charges may be based on a procedure fee schedule, a percentage of billed charges, per day (per diem) fees, per case fees, per treatment fees, or other methods. This document is intended to provide a condensed explanation of benefits. Please refer to the Description of Coverage (DOC) for details. In the case of a discrepancy between this document and the language contained within the DOC, the latter will take precedence. Benefit Coinsurance/Copayment Participating Non-Participating Rehabilitation Therapy Physical and Occupational Therapy InpatientInpatient 20% 20% Outpatient 20%* 20%* Speech Therapy Services — Inpatient 20% 20% Outpatient 20%* 20%* Special Benefits – Disease Management and Preventive Services Disease Management None Not covered Preventive Services — Laboratory None None Preventive Services — Physical Exam None None Screening and Preventive Counseling None None Special Benefits for Children Newborn Care 10% 10% Well Child Care Immunizations None None Well Child Care Laboratory Tests None None Well Child Care Physician Office Visits None None Special Benefits for Men Prostate Specific Antigen Test (screening) None None Special Benefits for Women Breast Pump None None Chlamydia Screening None None Contraceptive Implants (generic) None None Contraceptive lnjectables (generic) None None Contraceptive IUD (generic) None None In Vitro Fertilization 20%* 20%* Mammography (screening) None None Maternity Care 10% 10% Pap Smears (screening) None None Tubal Ligation None None Well Woman Exam None None Special Benefits for Homebound, Terminal, or Long-Term Care Home Health Care 20% 20% Hospice Services None None Behavioral Health – Mental Health and Substance Abuse Hospital and Facility Services 20% 20% Physician Services — Inpatient None None Outpatient $15 $15 Psychological Testing 20% 20% Special Offers Employee Assistance Program (EAP) Up to 6 fully-covered visits to assist subscribers with personal or family issues Health and Wellness Programs A variety of solutions for healthy living including Active&Fit® , Flu Prevention, Colorectal Cancer Screening, Maternity & Baby Care Incentive Program, and more Member Plus Discount Program Discounted prices and special offers from HMAA member groups and other participating merchants The Active&Fit and Active&Fit Direct programs are provided by American Specialty Health Fitness, Inc., a subsidiary of American Specialty Health Incorporated (ASH). Active&Fit Direct, Active&Fit Connected!, Active&Fit, and the Active&Fit Direct logos are trademarks of ASH and used with permission herein.
- 23. * = Annual Deductible Applies | % = Coinsurance (Percentage based on eligible charge) | $ = Copayment (Fixed dollar amount) Phone 591-0088 • Fax 591-0463 • Toll-Free 800-621-6998 • www.hmaa.com • Customer Service 941-4622 • Toll-Free 888-941-4622 00 ANNU COMP E-44-1 010119 DEDUCTIBLE APPLIES Plan Pays: Option Plus two Medical Plan Schedule of Benefits Annual Deductible $100 per person / $300 maximum per family Stop Loss $2,500 per person / $7,500 per family (per calendar year, includes deductibles & copayments) Lifetime Maximum Unlimited Benefit Coinsurance/Copayment Participating Non-Participating Hospital and Facility Services Ambulatory Surgical Center (ASC) 10% 30%* Hospital Ancillary Services 10% 30%* Hospital Room and Board 10% 30%* Outpatient Facility 10% 30%* Skilled Nursing Facility 10% 30%* Emergency Services Emergency Room 10% 10% Physician Visits 10% 10% Online Care and Telephonic Services None Not Covered Physician Services Physician Visits 10% 30%* Hospital Visits 10% 30%* Immunizations (standard, including travel) None 30%* Testing, Laboratory and Radiology Allergy Testing 20%* 30%* Allergy Treatment Materials 20%* 30%* Diagnostic Testing — Inpatient 10% 30%* Outpatient 20% 30%* Laboratory and Pathology — Inpatient 10% 30%* Outpatient 20% 30%* Radiology — Inpatient 10% 30%* Outpatient 20% 30%* Chemotherapy and Radiation Therapy Chemotherapy — Infusion/Injections 20%* 30%* Radiation Therapy — Inpatient Inpatient 10% 30%* Outpatient 20% 30%* Other Medical Services and Supplies Acupuncture, Chiropractic, Naturopathic Services 10% 30%* Ambulance (air) 20%* 30%* Ambulance (ground) 20%* 30%* Blood and Blood Products 20%* 30%* Dialysis and Supplies 20%* 30%* Durable Medical Equipment & Supplies 20%* 30%* Evaluations for Hearing Aids 20% 30%* Growth Hormone Therapy 20%* 30%* Home IV Therapy None 30%* Inhalation Therapy 20%* 30%* Injections 20%* 30%* Medical Foods 20% 30% Orthotics and External Prosthetics 20%* 30%* Vision and Hearing Appliances 20%* 30%*
- 24. * = Annual Deductible Applies | % = Coinsurance (Percentage based on eligible charge) | $ = Copayment (Fixed dollar amount) Note: Reimbursement is based on a percentage of HMAA’s eligible charges, not the billed charges. Eligible charges may be based on a procedure fee schedule, a percentage of billed charges, per day (per diem) fees, per case fees, per treatment fees, or other methods. This document is intended to provide a condensed explanation of benefits. Please refer to the Description of Coverage (DOC) for details. In the case of a discrepancy between this document and the language contained within the DOC, the latter will take precedence. Benefit Coinsurance/Copayment Participating Non-Participating Rehabilitation Therapy Physical and Occupational Therapy InpatientInpatient 10% 30%* Outpatient 20%* 30%* Speech Therapy Services — Inpatient 10% 30%* Outpatient 20%* 30%* Special Benefits – Disease Management and Preventive Services Disease Management None Not covered Preventive Services — Laboratory None 30%* Preventive Services — Physical Exam None 30%* Screening and Preventive Counseling None 30%* Special Benefits for Children Newborn Care 10% 30%* Well Child Care Immunizations None None Well Child Care Laboratory Tests None 30% Well Child Care Physician Office Visits None 30% Special Benefits for Men Prostate Specific Antigen Test (screening) 20% 30%* Special Benefits for Women Breast Pump None None* Chlamydia Screening None 30%* Contraceptive Implants (generic) None 30% Contraceptive lnjectables (generic) None 30% Contraceptive IUD (generic) None 30% In Vitro Fertilization 10% 30% Mammography (screening) None 30% Maternity Care 10% 30%* Pap Smears (screening) None 30%* Pregnancy Termination 10% 30%* Tubal Ligation None 30%* Well Woman Exam None 30%* Special Benefits for Homebound, Terminal, or Long-Term Care Home Health Care None 30%* Hospice Services None Not covered Behavioral Health – Mental Health and Substance Abuse Hospital and Facility Services 10% 30%* Physician Services 10% 30%* Psychological Testing — Inpatient 10% 30%* Outpatient 20% 30%* Special Offers Employee Assistance Program (EAP) Up to 6 fully-covered visits to assist subscribers with personal or family issues Health and Wellness Programs A variety of solutions for healthy living including Active&Fit® , Flu Prevention, Colorectal Cancer Screening, Maternity & Baby Care Incentive Program, and more Member Plus Discount Program Discounted prices and special offers from HMAA member groups and other participating merchants The Active&Fit and Active&Fit Direct programs are provided by American Specialty Health Fitness, Inc., a subsidiary of American Specialty Health Incorporated (ASH). Active&Fit Direct, Active&Fit Connected!, Active&Fit, and the Active&Fit Direct logos are trademarks of ASH and used with permission herein.
- 25. Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services Coverage Period: Beginning on or after 01/01/2019 Hawaii Medical Assurance Association: Option Plus Two Coverage for: Single/Two-Party/Family | Plan Type: PPO 1 of 6 COMP E-31 010119 (OP2) The Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, visit www.hmaa.com or call 1-888-941-4622. For general definitions of common terms, such as allowed amount, balance billing, coinsurance, copayment, deductible, provider, or other underlined terms see the Glossary. You can view the Glossary at www.hmaa.com or call 1-888-941-4622 to request a copy. Important Questions Answers Why This Matters: What is the overall deductible? $100/Individual or $300/family Generally, you must pay all of the costs from providers up to the deductible amount before this plan begins to pay. If you have other family members on the plan, each family member must meet their own individual deductible until the total amount of deductible expenses paid by all family members meets the overall family deductible. Are there services covered before you meet your deductible? Yes. Preventive care, primary care services, contraceptives, emergency services, prescription drug and supplies and well-child care services are covered before you meet your deductible. This plan covers some items and services even if you haven’t yet met the deductible amount. But a copayment or coinsurance may apply. For example, this plan covers certain preventive services without cost-sharing and before you meet your deductible. See a list of covered preventive services at https://www.healthcare.gov/coverage/preventive-care-benefits/. Are there other deductibles for specific services? No. You don’t have to meet deductibles for specific services. What is the out-of-pocket limit for this plan? $2,500/Individual or $7,500/family The out-of-pocket limit is the most you could pay in a year for covered services. If you have other family members in this plan, they have to meet their own out-of-pocket limits until the overall family out-of-pocket limit has been met. What is not included in the out-of-pocket limit? Copayments and coinsurance for certain services, premiums, balance-billing charges, and health care this plan doesn’t cover. Even though you pay these expenses, they do not count toward the out–of–pocket limit. Will you pay less if you use a network provider? Yes. See www.hmaa.com or call 1-888-941-4622 for a list of network providers. This plan uses a provider network. You will pay less if you use a provider in the plan’s network. You will pay the most if you use an out-of-network provider, and you might receive a bill from a provider for the difference between the provider’s charge and what your plan pays (balance billing). Be aware, your network provider might use an out-of-network provider for some services (such as lab work). Check with your provider before you get services. Do you need a referral to see a specialist? No. You can see the specialist you choose without a referral. OMB Control Numbers 1545‐2229, 1210‐0147, and 0938‐1146 Released on April 6, 2016
- 26. 2 of 6 COMP E-31 010119 (OP2) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) If you visit a health care provider’s office or clinic Primary care visit to treat an injury or illness 10% coinsurance; deductible does not apply 30% coinsurance None Specialist visit 10% coinsurance; deductible does not apply 30% coinsurance Preventive care/screening/ immunization No charge 30% coinsurance Age and frequency limitations may apply. You may have to pay for services that aren’t preventive. Ask your provider if the services you need are preventive. Then check what your plan will pay for. If you have a test Diagnostic test (x-ray, blood work) 20% coinsurance; deductible does not apply 30% coinsurance None Imaging (CT/PET scans, MRIs) 20% coinsurance; deductible does not apply 30% coinsurance If you need drugs to treat your illness or condition More information about prescription drug coverage is available at www.hmaa.com Generic drugs No charge 20% coinsurance Coverage limited to diabetic drugs and diabetic supplies for all members. Contraceptives covered for women only. Only preferred brand named diabetic supplies are covered at no charge. Diabetic drugs and non-preferred brand named diabetic supplies have a 20% coinsurance. Non-preferred brand named diabetic drugs have a 30% coinsurance. Diaphragms, cervical caps and generic contraceptives for women are covered at no charge when using a network provider. Preferred brand drugs 20% coinsurance 20% coinsurance Non-preferred brand drugs 20% coinsurance 30% coinsurance Specialty drugs No charge No charge Coverage for specialty drugs limited to oral chemotherapy only. If you have outpatient surgery Facility fee (e.g., ambulatory surgery center) 10% coinsurance; deductible does not apply 30% coinsurance None
- 27. 3 of 6 COMP E-31 010119 (OP2) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) Physician/surgeon fees 10% coinsurance; deductible does not apply 30% coinsurance If you need immediate medical attention Emergency room care 10% coinsurance; deductible does not apply 10% coinsurance; deductible does not apply None Emergency medical transportation 20% coinsurance 30% coinsurance Coverage for air transportation is limited to the United States. Urgent care $25 copay; deductible does not apply $50 copay; deductible does not apply None If you have a hospital stay Facility fee (e.g., hospital room) 10% coinsurance; deductible does not apply 30% coinsurance Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Physician/surgeon fees 10% coinsurance; deductible does not apply 30% coinsurance If you need mental health, behavioral health, or substance abuse services Outpatient services 10% coinsurance; deductible does not apply 30% coinsurance None Inpatient services 10% coinsurance; deductible does not apply 30% coinsurance Preauthorization is required. If you don't get preauthorization, benefits could be reduced. If you are pregnant Office visits 10% coinsurance; deductible does not apply 30% coinsurance None Childbirth/delivery professional services 10% coinsurance; deductible does not apply 30% coinsurance Childbirth/delivery facility services 10% coinsurance; deductible does not apply 30% coinsurance If you need help recovering or have other special health needs Home health care No charge 30% coinsurance Coverage limited to 150 days per calendar year. Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Rehabilitation services Inpatient: 10% coinsurance; deductible does not apply Inpatient: 30% coinsurance Preauthorization is required for inpatient services. If you don't get preauthorization, benefits could be reduced.Outpatient: 20% coinsurance Outpatient: 30% coinsurance
- 28. 4 of 6 COMP E-31 010119 (OP2) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) Habilitation services Not covered Not covered None Skilled nursing care Inpatient: 10% coinsurance; deductible does not apply 30% coinsurance Coverage limited to 120 days in any calendar year. Durable medical equipment 20% coinsurance 30% coinsurance Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Hospice services No Charge Not covered None If your child needs dental or eye care Children’s eye exam Not covered Not covered None Children’s glasses Not covered Not covered None Children’s dental check-up Not covered Not covered None Excluded Services & Other Covered Services: Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Cosmetic surgery Dental care (Adult) Long-term care Non-emergency care when traveling outside the U.S. Private-duty nursing Routine eye care (Adult) Routine foot care Weight loss programs Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Acupuncture Bariatric surgery Chiropractic care Hearing aids Infertility treatment Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: HMAA at (888) 941-4622 or CustomerService@hmaa.com, or the Department of Labor’s Employee Benefits Security Administration at 1-866-444-EBSA (3272) or www.dol.gov/ebsa/healthreform. Other coverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call 1-800-318-2596. Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called a grievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents also provide complete
- 29. 5 of 6 COMP E-31 010119 (OP2) information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance, contact: HMAA at (888) 941- 4622 or CustomerService@hmaa.com, or the Hawaii Insurance Division, ATTN: Health Insurance Branch – External Appeals, 335 Merchant Street, Room 213, Honolulu, HI 96813 at (808) 586-2804 or the Department of Labor Employment Benefits Security Administration at 1-866-444-EBSA (3272) or www.dol.gov/ebsa/healthreform. Does this plan provide Minimum Essential Coverage? Yes. If you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for an exemption from the requirement that you have health coverage for that month. Does this plan meet the Minimum Value Standards? Yes. If your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace. Language Access Services: Spanish (Español): Para obtener asistencia en Español, llame al 1-888-941-4622. Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 1-888-941-4622. Chinese (中文): 如果需要中文的帮助,请拨打这个号码 1-888-941-4622. Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' 1-888-941-4622. ––––––––––––––––––––––To see examples of how this plan might cover costs for a sample medical situation, see the next section.––––––––––––––––––––––
- 30. 6 of 6 The plan would be responsible for the other costs of these EXAMPLE covered services. Peg is Having a Baby (9 months of in-network pre-natal care and a hospital delivery) Mia’s Simple Fracture (in-network emergency room visit and follow up care) Managing Joe’s type 2 Diabetes (a year of routine in-network care of a well- controlled condition) The plan’s overall deductible $100 Specialist coinsurance 10% Hospital (facility) coinsurance 10% Other coinsurance 10% This EXAMPLE event includes services like: Specialist office visits (prenatal care) Childbirth/Delivery Professional Services Childbirth/Delivery Facility Services Diagnostic tests (ultrasounds and blood work) Specialist visit (anesthesia) Total Example Cost $12,800 In this example, Peg would pay: Cost Sharing Deductibles $0 Copayments $0 Coinsurance $1,364 What isn’t covered Limits or exclusions $60 The total Peg would pay is $1,424 The plan’s overall deductible $100 Specialist coinsurance 10% Hospital (facility) coinsurance 10% Other coinsurance 10% This EXAMPLE event includes services like: Primary care physician office visits (including disease education) Diagnostic tests (blood work) Prescription drugs Durable medical equipment (glucose meter) Total Example Cost $7,400 In this example, Joe would pay: Cost Sharing Deductibles $100 Copayments $0 Coinsurance $1,195 What isn’t covered Limits or exclusions $55 The total Joe would pay is $1,350 The plan’s overall deductible $100 Specialist coinsurance 10% Hospital (facility) coinsurance 10% Other coinsurance 10% This EXAMPLE event includes services like: Emergency room care (including medical supplies) Diagnostic test (x-ray) Durable medical equipment (crutches) Rehabilitation services (physical therapy) Total Example Cost $1,900 In this example, Mia would pay: Cost Sharing Deductibles $100 Copayments $0 Coinsurance $296 What isn’t covered Limits or exclusions $0 The total Mia would pay is $396 About these Coverage Examples: This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost sharing amounts (deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion of costs you might pay under different health plans. Please note these coverage examples are based on self-only coverage.
- 31. Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services Coverage Period: Beginning on or after 01/01/2019 Hawaii Medical Assurance Association: Option Plus Two Coverage for: Single/Two-Party/Family | Plan Type: PPO 1 of 6 COMP E-31 010119 (OP2) The Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, visit www.hmaa.com or call 1-888-941-4622. For general definitions of common terms, such as allowed amount, balance billing, coinsurance, copayment, deductible, provider, or other underlined terms see the Glossary. You can view the Glossary at www.hmaa.com or call 1-888-941-4622 to request a copy. Important Questions Answers Why This Matters: What is the overall deductible? $100/Individual or $300/family Generally, you must pay all of the costs from providers up to the deductible amount before this plan begins to pay. If you have other family members on the plan, each family member must meet their own individual deductible until the total amount of deductible expenses paid by all family members meets the overall family deductible. Are there services covered before you meet your deductible? Yes. Preventive care, primary care services, contraceptives, emergency services, prescription drug and supplies and well-child care services are covered before you meet your deductible. This plan covers some items and services even if you haven’t yet met the deductible amount. But a copayment or coinsurance may apply. For example, this plan covers certain preventive services without cost-sharing and before you meet your deductible. See a list of covered preventive services at https://www.healthcare.gov/coverage/preventive-care-benefits/. Are there other deductibles for specific services? No. You don’t have to meet deductibles for specific services. What is the out-of-pocket limit for this plan? $2,500/Individual or $7,500/family The out-of-pocket limit is the most you could pay in a year for covered services. If you have other family members in this plan, they have to meet their own out-of-pocket limits until the overall family out-of-pocket limit has been met. What is not included in the out-of-pocket limit? Copayments and coinsurance for certain services, premiums, balance-billing charges, and health care this plan doesn’t cover. Even though you pay these expenses, they do not count toward the out–of–pocket limit. Will you pay less if you use a network provider? Yes. See www.hmaa.com or call 1-888-941-4622 for a list of network providers. This plan uses a provider network. You will pay less if you use a provider in the plan’s network. You will pay the most if you use an out-of-network provider, and you might receive a bill from a provider for the difference between the provider’s charge and what your plan pays (balance billing). Be aware, your network provider might use an out-of-network provider for some services (such as lab work). Check with your provider before you get services. Do you need a referral to see a specialist? No. You can see the specialist you choose without a referral. OMB Control Numbers 1545‐2229, 1210‐0147, and 0938‐1146 Released on April 6, 2016
- 32. 2 of 6 COMP E-31 010119 (OP2) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) If you visit a health care provider’s office or clinic Primary care visit to treat an injury or illness 10% coinsurance; deductible does not apply 30% coinsurance None Specialist visit 10% coinsurance; deductible does not apply 30% coinsurance Preventive care/screening/ immunization No charge 30% coinsurance Age and frequency limitations may apply. You may have to pay for services that aren’t preventive. Ask your provider if the services you need are preventive. Then check what your plan will pay for. If you have a test Diagnostic test (x-ray, blood work) 20% coinsurance; deductible does not apply 30% coinsurance None Imaging (CT/PET scans, MRIs) 20% coinsurance; deductible does not apply 30% coinsurance If you need drugs to treat your illness or condition More information about prescription drug coverage is available at www.hmaa.com Generic drugs No charge 20% coinsurance Coverage limited to diabetic drugs and diabetic supplies for all members. Contraceptives covered for women only. Only preferred brand named diabetic supplies are covered at no charge. Diabetic drugs and non-preferred brand named diabetic supplies have a 20% coinsurance. Non-preferred brand named diabetic drugs have a 30% coinsurance. Diaphragms, cervical caps and generic contraceptives for women are covered at no charge when using a network provider. Preferred brand drugs 20% coinsurance 20% coinsurance Non-preferred brand drugs 20% coinsurance 30% coinsurance Specialty drugs No charge No charge Coverage for specialty drugs limited to oral chemotherapy only. If you have outpatient surgery Facility fee (e.g., ambulatory surgery center) 10% coinsurance; deductible does not apply 30% coinsurance None
- 33. 3 of 6 COMP E-31 010119 (OP2) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) Physician/surgeon fees 10% coinsurance; deductible does not apply 30% coinsurance If you need immediate medical attention Emergency room care 10% coinsurance; deductible does not apply 10% coinsurance; deductible does not apply None Emergency medical transportation 20% coinsurance 30% coinsurance Coverage for air transportation is limited to the United States. Urgent care $25 copay; deductible does not apply $50 copay; deductible does not apply None If you have a hospital stay Facility fee (e.g., hospital room) 10% coinsurance; deductible does not apply 30% coinsurance Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Physician/surgeon fees 10% coinsurance; deductible does not apply 30% coinsurance If you need mental health, behavioral health, or substance abuse services Outpatient services 10% coinsurance; deductible does not apply 30% coinsurance None Inpatient services 10% coinsurance; deductible does not apply 30% coinsurance Preauthorization is required. If you don't get preauthorization, benefits could be reduced. If you are pregnant Office visits 10% coinsurance; deductible does not apply 30% coinsurance None Childbirth/delivery professional services 10% coinsurance; deductible does not apply 30% coinsurance Childbirth/delivery facility services 10% coinsurance; deductible does not apply 30% coinsurance If you need help recovering or have other special health needs Home health care No charge 30% coinsurance Coverage limited to 150 days per calendar year. Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Rehabilitation services Inpatient: 10% coinsurance; deductible does not apply Inpatient: 30% coinsurance Preauthorization is required for inpatient services. If you don't get preauthorization, benefits could be reduced.Outpatient: 20% coinsurance Outpatient: 30% coinsurance
- 34. 4 of 6 COMP E-31 010119 (OP2) All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies. Common Medical Event Services You May Need What You Will Pay Limitations, Exceptions, & Other Important Information Network Provider (You will pay the least) Out-of-Network Provider (You will pay the most) Habilitation services Not covered Not covered None Skilled nursing care Inpatient: 10% coinsurance; deductible does not apply 30% coinsurance Coverage limited to 120 days in any calendar year. Durable medical equipment 20% coinsurance 30% coinsurance Preauthorization is required. If you don't get preauthorization, benefits could be reduced. Hospice services No Charge Not covered None If your child needs dental or eye care Children’s eye exam Not covered Not covered None Children’s glasses Not covered Not covered None Children’s dental check-up Not covered Not covered None Excluded Services & Other Covered Services: Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Cosmetic surgery Dental care (Adult) Long-term care Non-emergency care when traveling outside the U.S. Private-duty nursing Routine eye care (Adult) Routine foot care Weight loss programs Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Acupuncture Bariatric surgery Chiropractic care Hearing aids Infertility treatment Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: HMAA at (888) 941-4622 or CustomerService@hmaa.com, or the Department of Labor’s Employee Benefits Security Administration at 1-866-444-EBSA (3272) or www.dol.gov/ebsa/healthreform. Other coverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call 1-800-318-2596. Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called a grievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents also provide complete
- 35. 5 of 6 COMP E-31 010119 (OP2) information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance, contact: HMAA at (888) 941- 4622 or CustomerService@hmaa.com, or the Hawaii Insurance Division, ATTN: Health Insurance Branch – External Appeals, 335 Merchant Street, Room 213, Honolulu, HI 96813 at (808) 586-2804 or the Department of Labor Employment Benefits Security Administration at 1-866-444-EBSA (3272) or www.dol.gov/ebsa/healthreform. Does this plan provide Minimum Essential Coverage? Yes. If you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for an exemption from the requirement that you have health coverage for that month. Does this plan meet the Minimum Value Standards? Yes. If your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace. Language Access Services: Spanish (Español): Para obtener asistencia en Español, llame al 1-888-941-4622. Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 1-888-941-4622. Chinese (中文): 如果需要中文的帮助,请拨打这个号码 1-888-941-4622. Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' 1-888-941-4622. ––––––––––––––––––––––To see examples of how this plan might cover costs for a sample medical situation, see the next section.––––––––––––––––––––––
- 36. 6 of 6 The plan would be responsible for the other costs of these EXAMPLE covered services. Peg is Having a Baby (9 months of in-network pre-natal care and a hospital delivery) Mia’s Simple Fracture (in-network emergency room visit and follow up care) Managing Joe’s type 2 Diabetes (a year of routine in-network care of a well- controlled condition) The plan’s overall deductible $100 Specialist coinsurance 10% Hospital (facility) coinsurance 10% Other coinsurance 10% This EXAMPLE event includes services like: Specialist office visits (prenatal care) Childbirth/Delivery Professional Services Childbirth/Delivery Facility Services Diagnostic tests (ultrasounds and blood work) Specialist visit (anesthesia) Total Example Cost $12,800 In this example, Peg would pay: Cost Sharing Deductibles $0 Copayments $0 Coinsurance $1,364 What isn’t covered Limits or exclusions $60 The total Peg would pay is $1,424 The plan’s overall deductible $100 Specialist coinsurance 10% Hospital (facility) coinsurance 10% Other coinsurance 10% This EXAMPLE event includes services like: Primary care physician office visits (including disease education) Diagnostic tests (blood work) Prescription drugs Durable medical equipment (glucose meter) Total Example Cost $7,400 In this example, Joe would pay: Cost Sharing Deductibles $100 Copayments $0 Coinsurance $1,195 What isn’t covered Limits or exclusions $55 The total Joe would pay is $1,350 The plan’s overall deductible $100 Specialist coinsurance 10% Hospital (facility) coinsurance 10% Other coinsurance 10% This EXAMPLE event includes services like: Emergency room care (including medical supplies) Diagnostic test (x-ray) Durable medical equipment (crutches) Rehabilitation services (physical therapy) Total Example Cost $1,900 In this example, Mia would pay: Cost Sharing Deductibles $100 Copayments $0 Coinsurance $296 What isn’t covered Limits or exclusions $0 The total Mia would pay is $396 About these Coverage Examples: This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost sharing amounts (deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion of costs you might pay under different health plans. Please note these coverage examples are based on self-only coverage.
- 37. * = Annual Deductible Applies | % = Coinsurance (Percentage based on eligible charge) | $ = Copayment (Fixed dollar amount) Phone 591-0088 • Fax 591-0463 • Toll-Free 800-621-6998 • www.hmaa.com • Customer Service 941-4622 • Toll-Free 888-941-4622 00 ANNU COMP E-44-1 010119 DEDUCTIBLE APPLIES Plan Pays: Option Plus two Medical Plan Schedule of Benefits Annual Deductible $100 per person / $300 maximum per family Stop Loss $2,500 per person / $7,500 per family (per calendar year, includes deductibles & copayments) Lifetime Maximum Unlimited Benefit Coinsurance/Copayment Participating Non-Participating Hospital and Facility Services Ambulatory Surgical Center (ASC) 10% 30%* Hospital Ancillary Services 10% 30%* Hospital Room and Board 10% 30%* Outpatient Facility 10% 30%* Skilled Nursing Facility 10% 30%* Emergency Services Emergency Room 10% 10% Physician Visits 10% 10% Online Care and Telephonic Services None Not Covered Physician Services Physician Visits 10% 30%* Hospital Visits 10% 30%* Immunizations (standard, including travel) None 30%* Testing, Laboratory and Radiology Allergy Testing 20%* 30%* Allergy Treatment Materials 20%* 30%* Diagnostic Testing — Inpatient 10% 30%* Outpatient 20% 30%* Laboratory and Pathology — Inpatient 10% 30%* Outpatient 20% 30%* Radiology — Inpatient 10% 30%* Outpatient 20% 30%* Chemotherapy and Radiation Therapy Chemotherapy — Infusion/Injections 20%* 30%* Radiation Therapy — Inpatient Inpatient 10% 30%* Outpatient 20% 30%* Other Medical Services and Supplies Acupuncture, Chiropractic, Naturopathic Services 10% 30%* Ambulance (air) 20%* 30%* Ambulance (ground) 20%* 30%* Blood and Blood Products 20%* 30%* Dialysis and Supplies 20%* 30%* Durable Medical Equipment & Supplies 20%* 30%* Evaluations for Hearing Aids 20% 30%* Growth Hormone Therapy 20%* 30%* Home IV Therapy None 30%* Inhalation Therapy 20%* 30%* Injections 20%* 30%* Medical Foods 20% 30% Orthotics and External Prosthetics 20%* 30%* Vision and Hearing Appliances 20%* 30%*
- 38. * = Annual Deductible Applies | % = Coinsurance (Percentage based on eligible charge) | $ = Copayment (Fixed dollar amount) Note: Reimbursement is based on a percentage of HMAA’s eligible charges, not the billed charges. Eligible charges may be based on a procedure fee schedule, a percentage of billed charges, per day (per diem) fees, per case fees, per treatment fees, or other methods. This document is intended to provide a condensed explanation of benefits. Please refer to the Description of Coverage (DOC) for details. In the case of a discrepancy between this document and the language contained within the DOC, the latter will take precedence. Benefit Coinsurance/Copayment Participating Non-Participating Rehabilitation Therapy Physical and Occupational Therapy InpatientInpatient 10% 30%* Outpatient 20%* 30%* Speech Therapy Services — Inpatient 10% 30%* Outpatient 20%* 30%* Special Benefits – Disease Management and Preventive Services Disease Management None Not covered Preventive Services — Laboratory None 30%* Preventive Services — Physical Exam None 30%* Screening and Preventive Counseling None 30%* Special Benefits for Children Newborn Care 10% 30%* Well Child Care Immunizations None None Well Child Care Laboratory Tests None 30% Well Child Care Physician Office Visits None 30% Special Benefits for Men Prostate Specific Antigen Test (screening) 20% 30%* Special Benefits for Women Breast Pump None None* Chlamydia Screening None 30%* Contraceptive Implants (generic) None 30% Contraceptive lnjectables (generic) None 30% Contraceptive IUD (generic) None 30% In Vitro Fertilization 10% 30% Mammography (screening) None 30% Maternity Care 10% 30%* Pap Smears (screening) None 30%* Pregnancy Termination 10% 30%* Tubal Ligation None 30%* Well Woman Exam None 30%* Special Benefits for Homebound, Terminal, or Long-Term Care Home Health Care None 30%* Hospice Services None Not covered Behavioral Health – Mental Health and Substance Abuse Hospital and Facility Services 10% 30%* Physician Services 10% 30%* Psychological Testing — Inpatient 10% 30%* Outpatient 20% 30%* Special Offers Employee Assistance Program (EAP) Up to 6 fully-covered visits to assist subscribers with personal or family issues Health and Wellness Programs A variety of solutions for healthy living including Active&Fit® , Flu Prevention, Colorectal Cancer Screening, Maternity & Baby Care Incentive Program, and more Member Plus Discount Program Discounted prices and special offers from HMAA member groups and other participating merchants The Active&Fit and Active&Fit Direct programs are provided by American Specialty Health Fitness, Inc., a subsidiary of American Specialty Health Incorporated (ASH). Active&Fit Direct, Active&Fit Connected!, Active&Fit, and the Active&Fit Direct logos are trademarks of ASH and used with permission herein.
- 39. $5,000 Employer paid Life Insurance is included Comp Basic Bi-Weekly Deduction Comp Plus Bi-Weekly Deduction HMO Bi-Weekly Deduction Employee Only 1.5% of wages Employee Only $10.46 + 1.5% of wages Employee Only $66.04 + 1.5% of wages Employee + Spouse $152.57 + 1.5% of wages Employee + Spouse $175.57 + 1.5% of wages Employee + Spouse $292.89 + 1.5% of wages Employee + Child(ren) $103.99 + 1.5% of wages Employee + Child(ren) $122.82 + 1.5% of wages Employee + Child(ren) $259.91 + 1.5% of wages Employee + Family $268.5 + 1.5% of wages Employee + Family $300.91 + 1.5% of wages Employee + Family $477.06 + 1.5% of wages Bi-Weekly Deduction Bi-Weekly Deduction Bi-Weekly Deduction Employee Only $22.32 + 1.5% of wages Employee Only $32.78 + 1.5% of wages Employee Only $88.36 + 1.5% of wages Employee + Spouse $199.81 + 1.5% of wages Employee + Spouse $222.81 + 1.5% of wages Employee + Spouse $340.13 + 1.5% of wages Employee + Child(ren) $149.18 + 1.5% of wages Employee + Child(ren) $168.01 + 1.5% of wages Employee + Child(ren) $305.1 + 1.5% of wages Employee + Family $339.71 + 1.5% of wages Employee + Family $372.12 + 1.5% of wages Employee + Family $548.27 + 1.5% of wages Bi-Weekly Deduction Bi-Weekly Deduction Bi-Weekly Deduction Employee Only 8.57$ Employee Only 12.91$ Employee Only 0.84$ Employee + Spouse 17.14$ Employee + Spouse 28.42$ Employee + Spouse 1.68$ Employee + Child(ren) 18.85$ Employee + Child(ren) 24.54$ Employee + Child(ren) 1.80$ Employee + Family 25.71$ Employee + Family 42.62$ Employee + Family 2.88$ JJC Hawaii, LLC - Jamba Juice Hawaii MEDICAL BENEFIT PACKAGES AND RATES Team Member and Team Leader Effective October 1, 2019 - September 30, 2020 HMAA Comprehensive Plus Plan VOLUNTARY"Buyup" HMAA Option Plus Two Plan VOLUNTARY"Buyup" Kaiser Permanente BASEPLAN Medical Medical Medical **Default Medical ONLY Plan** HMAA Option Plus Two ONLY Kaiser HMO ONLY VOLUNTARY"Buyup" Medical + Drug + Vision + Dental VOLUNTARY"Buyup" Medical + Drug + Vision + Dental VOLUNTARY"Buyup" VOLUNTARY"StandAlone" Dental VOLUNTARY"Add-On" Pharmacy Add-On VOLUNTARY"StandAlone" Dental ONLY *Must be enrolled in a Medical plan Vision ONLY All bi-weekly deductions (26 pay-periods per year) will be deducted from payroll on a pre-tax basis via the Cafeteria Section 125 Plan, unless you opt-out in writing. Medical + Drug + Vision + Dental Package includes HMAA Comp Plus with voluntary Prescription Drug, Vision and Dental Package includes HMAA Option Plus Two with voluntary Prescription Drug, Vision and Dental Package includes Kaiser Medical with voluntary Prescription Drug, Vision and Dental Vision
- 40. 201 Kaiser Permanente Group Plan 201 Benefit and Payment Chart 3651 BLUE PACIFIC MANAGEMENT About this chart This benefit and payment chart: • Is a summary of covered services and other benefits. It is not a complete description of your benefits. For coverage criteria, description and limitations of covered Services, and excluded Services, be sure to read Chapter 1: Important Information, Chapter 3: Benefit Description, and Chapter 4: Services Not Covered. • Tells you if a covered service or supply is subject to limits or referrals. • Gives you the page number where you can find the description of your services and other benefits. • Tells you what your Cost Share is for covered services and supplies. Note: Special limits may apply to services or other benefits listed in this benefit and payment chart. Please read the benefit description found on the page referenced by this chart. You only pay a single Cost Share for covered benefits you receive in the Total Care Service settings. If your care is not received in a Total Care setting, you pay the Cost Share for each medical service or item in accord with its relevant benefit section. Remember, services and other benefits are available only for care you receive when provided, prescribed, or directed by your KP Hawaii Care Team except for care for Emergency Services and out-of-state Urgent Care. To find a Medical Office near you visit our website at www.kp.org. For more information on these services see Chapter 3: Benefit Description. You are encouraged to choose a Personal Care Physician (PCP). You may choose any PCP that is available to accept you. Parents may choose a pediatrician as the PCP for their child. You do not need a referral or prior authorization to obstetrical or gynecological care from a health care professional who specializes in obstetrics or gynecology. Your Physician, however, may have to get prior authorization for certain Services. Additionally, in accord with state law, you do not need a referral or prior authorization to obtain access to physical therapy from a physical therapist or Physician who specialized in physical therapy. Members age 65 and over (excluding Tax Equity and Fiscal Responsibility Act of 1982 ”TEFRA” members) must meet the required eligibility requirements to receive the benefit of either 1) those listed in this Benefit Summary, or 2) benefits covered under Original Medicare. See Chapter 9: Coordination of Benefits. Senior Advantage Members, please refer to your Senior Advantage Evidence of Coverage. 2019 Kaiser Permanente Hawaii’s Guide–GP Page 1 of 8 Benefit Summary
- 41. Description Cost Share Annual Copayment Maximum Member $2,500 per calendar year Family Unit (3 or more members) $7,500 per calendar year Annual Deductible Member None per calendar year Family Unit None Routine and Preventive Health Education and Disease Management •Physician Visits •Primary Care $20 per visit •Specialty Care $20 per visit •Tobacco Cessation and Counseling Sessions None •Health education publications None •Healthy Living Classes Applicable class fees Immunizations (endorsed by the Centers for Disease Control and Prevention (CDC)) None •Office visit for (CDC) Immunizations None •Office visit for Travel Immunization •Primary Care $20 per visit •Specialty Care $20 per visit •Unexpected Mass Population Immunizations 50% of all Applicable Charges Office Visits •Well-Child Care None •Annual Preventive Care (physical exam) Office Visit None •Hearing Exam (for correction) •Primary Care $20 per visit •Specialty Care $20 per visit •Vision Exam (for glasses) •Primary Care $20 per visit •Specialty Care $20 per visit Preventive Screenings and Care None Total Health Assessment (www.kp.org) None Special Services for Women Preventive Care •Annual Gynecological Exam None •Mammography (screening) None •Pap Smears (cervical cancer screening) None Family Planning Visits •Primary Care $20 per visit •Specialty Care $20 per visit Infertility Consultation •Primary Care $20 per visit •Specialty Care $20 per visit In Vitro Fertilization 20% of applicable charges Maternity •Maternity Care–routine prenatal visits None •Maternity Care–delivery 20% of applicable charges •Maternity Care–one postpartum visit None 2019 Kaiser Permanente Hawaii’s Guide–GP Page 2 of 8 Benefit Summary
- 42. Description Cost Share •Maternity and Newborn Length of Stay 20% of applicable charges •Breast Pump None Contraceptive Drugs and Devices See Prescription Drugs Pregnancy Termination •Primary Care $20 per visit •Specialty Care $20 per visit •Total Care Settings Included in Total Care Services Voluntary Sterilization (including tubal ligation) •Medical Office •Total Care Settings Included in Total Care Settings Special Services for Men Prostate Specific Antigen (screening) $10 per day Vasectomy •Primary Care $20 per visit •Specialty Care $20 per visit •Total Care Settings Included in Total Care Settings Online Care My Health Manager (www.kp.org) None Office Visits Office Visits •Primary Care $20 per visit •Specialty Care $20 per visit •Routine pre-surgical and post-surgical None Urgent Care Visits •Within Service Area (Primary Care) $20 per visit •Within Service Area (Specialty Care) $20 per visit •Outside Service Area 20% of Applicable Charges Dependent Child Outside of Service Area •Routine Primary Care $20 per visit •Basic laboratory and general imaging $10 per visit •Testing 20% of applicable charges •Self-administered drug prescriptions 20% of applicable charges House Calls •Primary Care $20 per visit •Specialty Care $20 per visit Telehealth $20 per visit; Cost share will vary depending on service. 2019 Kaiser Permanente Hawaii’s Guide–GP Page 3 of 8 Benefit Summary
- 43. Description Cost Share Laboratory, Imaging, and Testing Laboratory •Basic $10 per day •Specialty 20% of applicable charges Imaging •Basic $10 per day •Specialty 20% of applicable charges Testing •Allergy Testing •Primary Care $20 per visit •Specialty Care $20 per visit •Skilled-Administered Drugs 20% of applicable charges •Diagnostic Testing 20% of applicable charges Surgery Outpatient Surgery and Procedures •Primary Care $20 per visit •Specialty Care $20 per visit •Total Care Settings Included in Total Care Services Reconstructive Surgery •Primary Care $20 per visit •Specialty Care $20 per visit •Covered Mastectomy 20% of applicable charges •Total Care Settings Included in Total Care Services Total Care Services You only pay a single Cost Share for covered benefits you receive in the following Total Care Service settings: Inpatient Hospital Services 20% of applicable charges Outpatient Surgery and Procedures in a Hospital-Based Setting or Ambulatory Surgery Center (ASC) 20% of applicable charges Emergency Services 20% of applicable charges in area, 20% of applicable charges out of area. Observation 20% of applicable charges Skilled Nursing Facility 20% of applicable charges Dialysis •Dialysis 20% applicable charges •Equipment, Training and Medical Supplies for home Dialysis None Radiation Therapy 20% of applicable charges Ambulance Air Ambulance 20% of applicable charges Ground Ambulance 20% of applicable charges Physical, Occupational, and Speech Therapy Physical and Occupational Therapy •Primary Care $20 per visit •Specialty Care $20 per visit •Home Health Care None •Total Care Settings Included in Total Care Services Speech Therapy •Primary Care $20 per visit 2019 Kaiser Permanente Hawaii’s Guide–GP Page 4 of 8 Benefit Summary
- 44. Description Cost Share •Specialty Care $20 per visit •Home Health Care None •Total Care Settings Included in Total Care Services Home Health Care and Hospice Care Home Health Care None Hospice Care None Physician Visits •Primary Care $20 per visit •Specialty Care $20 per visit Chemotherapy •Primary Care $20 per visit •Specialty Care $20 per visit •Total Care Settings Included in Total Care Services Internal, External Prosthetics Devices and Braces Implanted Internal Prosthetics, Devices and Aids •Medical Office None •Total Care Settings Included in Total Care Services External Prosthetics Devices •Outpatient 20% of applicable charges •Total Care Settings Included in Total Care Services Braces •Outpatient 20% of applicable charges •Total Care Settings Included in Total Care Services Durable Medical equipment Durable Medical equipment •Outpatient 20% of applicable charges •Total Care Settings Included in Total Care Services Oxygen (for use with DME) •Outpatient 20% of applicable charges •Total Care Settings Included in Total Care Services Repair or Replacement •Outpatient 20% of applicable charges •Total Care Settings Included in Total Care Services Diabetes Equipment 50% of Applicable Charges Home Phototherapy equipment None Behavioral Health–Mental Health and Substance Abuse Mental Health Care •Medical Office $20 per visit •Total Care Settings Included in Total Care Services Chemical Dependency Care •Medical Office $20 per visit 2019 Kaiser Permanente Hawaii’s Guide–GP Page 5 of 8 Benefit Summary