Facial nerve
- 1. FACIAL NERVE
- 2. CONTENTS 1. Introduction 2. Nuclei of origin 3. Course & Relations 4. Branches of facial nerve 5. Ganglia associated with facial nerve 6. Testing of facial nerve 7. Identification of facial nerve 8. Nerve injury
- 3. Introduction • The Facial nerve is the 7th of twelve paired cranial nerves. • It is a mixed nerve with motor and sensory roots. • It also supplies pre-ganglionic parasympathetic fibres to several head and neck ganglia
- 4. Nuclei of Origin 1. Motor nucleus 2. Superior salivatory nucleus 3. Nucleus of tractus solitarius
- 5. The facial nerve is formed mainly of two parts: • 1- Facial nerve proper (motor): arising from facial motor nucleus in pons. • 2- Nervus intermedius: it is the sensory root of facial lies position between the facial proper and vestibulcochlear nerve in the pontocerebellar angle. Carrying para-sympathetic fibers (from superior salivary nucleus) and taste fibers ( to the solitary nucleus).
- 6. Course & Relations • I- Intracranial (intrapetrosal) course • II- Extracranial course
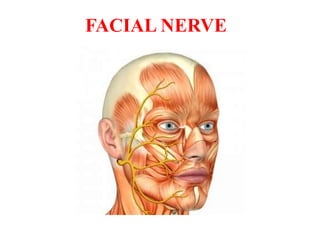
- 13. Branches 1. Greater superficial petrosal – arises from the geniculate ganglion. 2. Branches within the facial canal: • i) nerve to stapedius • ii) Chorda tympani 3. After exit from stylomastoid foramen: • i) Posterior auricular • ii) Nerve to posterior belly of digastric • iii) Nerve to stylohyoid. 4. On the face - Five major branches: • i) Temporal • ii) Zygomatic • iii) Buccal • iv) Marginal mandibular • v) Cervical
- 14. Ganglia associated with facial nerve • Geniculate ganglion • Submandibular ganglion • Pterygopalatine ganglion
- 15. Geniculate ganglion • The geniculate ganglion (from Latin genu, for "knee") is an L-shaped collection of fibers and sensory neurons of the facial nerve located in the facial canal of the head. • It receives fibers from the motor, sensory, and parasympathetic components of the facial nerve
- 16. Submandibular ganglion • The submandibular ganglion is small and fusiform in shape. It is situated above the deep portion of the submandibular gland, on the hyoglossus muscle, near the posterior border of the mylohyoid muscle
- 17. Pterygopalatine ganglion • The pterygopalatine ganglion (meckel's ganglion, nasal ganglion or sphenopalatine ganglion) is a parasympathetic ganglion found in the pterygopalatine fossa. • It's largely innervated by the greater petrosal nerve (a branch of the facial nerve); and its axons project to the lacrimal glands and nasal mucosa
- 18. Facial Nerve blood supply • The facial nerve gets it’s blood supply from 5 vessels: Anterior inferior cerebellar artery – at the cerebellopontine angle Labyrinthine artery (branch of anterior inferior cerebellar artery) – within internal acoustic meatus Superficial petrosal artery (branch of middle meningeal artery) – geniculate ganglion and nearby parts Stylomastoid artery (branch of posterior auricular artery) – mastoid segment Posterior auricular artery supplies the facial nerve at & distal to stylomastoid foramen • Venous drainage parallels the arterial blood supply
- 19. Testing of Facial Nerve Branches • Temporal branches -patient is asked to frown and wrinkle his or her forehead. • Zygomatic branches -the patient is asked to close their eyes tightly • Buccal branches -puff up cheeks (buccinator) smile and show teeth (orbicularis oris) tap with finger over each cheek to detect ease of air expulsion on the affected side
- 20. Applied Surgical anatomy of Facial Nerve in Oral & Maxillofacial Surgery After exiting the stylomastoid foramen, which is situated posterolateral to stylomastoid process, the nerve enters the substance of parotid gland where it divides into its upper and lower divisions just posterior to the mandible The approximate distance from the lowest point of the external bony auditory meatus to the bifurcation of the facial nerve is 2.3cm Posterior to the parotid gland,the nerve is atleast 2cm deep into the skin surface,from this point the two branches curve around the posterior mandible,where they form plexus between the parotid gland and the masseter muscle
- 21. Temporal branch • It exits the parotid gland anterior to superficial temporal artery During an open approach to the TMJ, violation of this branch is possible
- 22. Zygomatic Branch : • Its course is antero superior crossing the zygomatic bone Inadvertent damage may occur to this nerve during open reduction of zygomatic arch or with the use of a byrd screw or zygomatic hook during closed approaches
- 23. The surgeon must be mindful of the facial nerves intimate involvement with the TMJ, specially when performing surgical approaches to the joint. The temporal and zygomatic branches are at increased risk during pre auricular approach and the marginal mandibular branch during submandibular approach The intra oral approach to the TMJ has minimal risk to the branches of facial nerve which is its major advantage
- 24. Buccal Branch: • It runs almost horizontally and will often divide into separate branch above and below parotid duct as it runs anteriorly Injury is possible in association with soft tissue trauma to the cheek region
- 25. Marginal mandibular branch: • It extends anteriorly and inferiorly within the substance of parotid gland, there may be two or three branches of this nerve. These branches run anteriorly parallel to inferior border of mandible and in some cases the course of the nerve is above the inferior border. In essentially all cases the nerve is located above the inferior border of mandible beyond the facial artery. The marginal mandibular branch is an important structure encountered at the inferior border of the mandible just beneath the platysma muscle fibres during an open approach to the mandibular angle and body area. • For this reason, an initial incision made approximately 1 to 1.5cm below the inferior border which prevents direct exposure or trauma to the nerve
- 26. Cervical Branch: • The cervical branch exits the parotid gland above its inferior pole and runs downwards underneath the platysma muscle
- 27. Identification of Facial Nerve 3 surgical maneuvers used to identify nerve trunk A. Blood free plane in front of external acoustic meatus B. Exposure of anterior border of SCM below insertion into mastoid process C. Peripheral identification of terminal branch of facial nerve (marginal mandibular branch)
- 29. Supra nuclear type: • Paralysis of lower part of face (opposite side) • Normal taste and saliva secretion • Stapedius not paralysed Nuclear type: • Paralysis of facial muscle (same side) • Paralysis of lateral rectus • Internal strabismus
- 30. Peripheral lesion At internal acoustic meatusa Paralysis of secretomotor fibers Hyper acusis Loss of corneal reflex Taste fibers unaffected Facial expression and movements paralysed Injury distal to geniculate ganglion Complete motor paralysis (same side) No hyper acusis Loss of corneal reflex Taste fibers affected Facial expression and movements paralysed Pronounced reaction of degeneration Injury at stylomastoid foramen Bell’s Palsy
- 31. THANK YOU
