Pneumonia
- 1. Puru Koirala Resident, Division of Pulmonary, Critical and Sleep Medicine Department of Internal Medicine BPKIHS Pneumonias
- 2. BPKIHS 72/F, Dharan-7 Presenting Complaints- – Fever- 2 days – Cough-2 days – Chest pain-2 days – Increased sleepiness since 24 hours
- 3. Past History: – No similar illness in the past – No known DM,PTB, HTN or other known co-morbidity Personal History: – Current smoker, 5 cigarettes/day, 12 pack year – Chronic Alcohol Consumer • Daily consumed 150ml home made alcohol
- 4. Physical Examination • GCS E4 M6 V4(Oriented to person not to place and time) • BP:90/60 mmHg with Ionotropic support ,Rt arm supine • Pulse: 112/min normal volume, regular Dorsalis Pedis Palpable bilaterally • RR:32/min, thoraco-abdominal type, shallow • Temperature: afebrile • SpO2:98% with O2 by facemask @ 6L/min • No pallor • No Icterus • No Lymphadenopathy • No Cyanosis • No Clubbing • No Odema • Dehydration
- 5. • Chest: – Expansion of Rt. Hemithorax less than Lt. – Tactile fremitus increased in Rt.Infra-axillary & infrascapular area – Dullness on percussion – B/L equal intensity of VBS – Fine end inspiratory crepitations in Rt. Infrascapular and infra-axillary area – No pleural rub • CVS – AB 5th ICS – S1+, S2+ No murmur • Abdomen – Soft, non tender – No organomegaly – BS normoactive
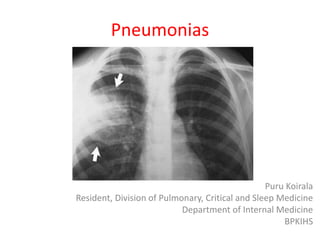
- 6. Investigation • Hb-13.8 gm/dl • PCV-41.1 • TLC- 220005700/ml • DLC-N80L17M 2 E1 • Platelet- 59000134000/ml • PT/INR-20/13/1.87 • RBS 102mg/dl • Urea- 5723mg/dl • Creatinine 2.40.9mg/dl • Na/K:140/3.4 144/4.6 mmol/lt • ECG:Sinus Tacycardia • CXR PA-view: Rt. Lower zone inhomogenous opacity ABG • Ph;7.527.46 • Pco2:2336 • PO2: 82--151 • HCO3-2022 • Lac : 3.21.1 • ESR-51 mm/hr • Mantoux< 5mm • Sputum for AFB *3 Negative • Sputum C/S:Normal respiratory flora • Blood culture:Sterile in 48 hrs • D-dimer; O.4 ng/dl
- 7. Impression • Acute Febrile Illness with Right lower lobe Community Acquired Pneumonia with CURB- 65- 5/5 ( Severe Pneumonia) presented in sepsis with septic shock with Multi-organ Dysfunction Syndrome(MODS) with AKI Lactic Acidosis Thrombocytopenia
- 8. Management • ICU admission • O2 therapy:FiO2 @40%, flow rate 6-8LPM via facemask • Inj. 1000ml( 20ml/kg) NS stat. • Inj. Hydrocort. 50mg iv stat &QID* 7days. • Inj. Nordrenaline @ 10ugm/min tapered in 3days. • Inj. Ceftriaxone 1gm iv BD * 7days • Inj. Levofloxacin 750mg iv OD * 5 days
- 9. Topic Review Community- Acquired Pneumonia (CAP)
- 10. Definition • Pneumonia is an infection of the pulmonary parenchyma • CAP: An infection that begins outside of the hospital or is diagnosed within 48 h after admission to the hospital in a patient who has not been hospitalized or visited health care facility in last 3 month Current Diagnosis and Treatment in Pulmonary Medicine 2008
- 11. Definition HCAP= Pneumonia in a patient with at least one of the following risk factors: 1. Hospitalization for two or more days in the last 90 days 2. Residence in a nursing home or long-term care facility in the last 90 days 3. Receiving outpatient intravenous therapy (like antibiotics or chemotherapy) within the past 30 days 4. Receiving home wound care within the past 30 days 5. Attending a hospital clinic or dialysis center in the last 30 days 6. Having a family member with known multi-drug resistant pathogens
- 12. Definition • HAP: Infection of lung parenchyma occurring more than 48 h after admission to a hospital • VAP: When HAP occurs in the subset of patients receiving mechanical ventilation, it is termed VAP
- 13. • Aspiration pneumonitis (Mendelson's syndrome) is a chemical injury caused by the inhalation of sterile gastric contents, whereas aspiration pneumonia is an infectious process caused by the inhalation of oropharyngeal secretions that are colonized by pathogenic bacteria • The term “aspiration pneumonia,” refers specifically to the development of a radiographically evident infiltrate in patients who are at increased risk for oropharyngeal aspiration • Anaerobes play a significant role only when an episode of aspiration has occurred days to weeks before presentation for pneumonia Aspiration Pneumonitis and Aspiration Pneumonia Paul E. Marik, M.B., B.Ch. N Engl J Med 2001; 344:665-671March 1, 2001
- 14. Epidemiology • CAP, together with influenza, remains the seventh leading cause of death especially in the extremes of ages • 80% of the 4 million CAP – an outpatient basis • 20% in the hospital • Responsible for – 600,000 hospitalizations – 64 million days of restricted activity – 45,000 deaths • 55% AKI patients presented with diagnosis of CAP. – Outcomes of Acute Kidney Injury:A Hospital Based Study, 2009-10; Koirala P et al
- 15. PATHOPHYSIOLOGY • Pneumonia results from – Proliferation of microbial pathogens at the alveolar level – Host's response to those pathogens • Modes of Acquisition – Inhalation of infected Nasopharayngeal secretions – Aspiration from the oropharynx • sleep (in the elderly) • decreased levels of consciousness – Hematogenous spread (e.g., from tricuspid endocarditis) or by contiguous extension from an infected pleural or mediastinal space
- 16. Pulmonary Clearance of Infectious Agents Mechanical Defenses: Nasopharyngeal Airways Conducting Airways Hairs and turbinates of the nares Normal flora adhering to mucosal cells of the oropharynx Gag reflex and the cough mechanism Branching architecture of the Tracheobronchial tree Mucociliary clearance and local antibacterial factors Innate Immunity: Innate Immune Recognition Resident alveolar macrophages NK Cells Complement Alveolar Epithelial Cells (e.g., surfactant proteins A and D)
- 17. PATHOPHYSIOLOGY Capacity of the alveolar macrophages exceeded The inflammatory response • The host Inflammatory Response, rather than the proliferation of microorganisms, triggers the clinical syndrome of pneumonia • Adaptive Immune Response
- 18. PATHOPHYSIOLOGY Macrophage • IL-1, TNF alpha IL-8 and G-CSF • Fever Peripheral leukocytosis Purulent secretions Respiratory alkalosis Alveolar filling( Rales,Hypoxemia)
- 19. PATHOLOGY 1. Edema or Congestion 2. Red hepatization 3. Gray hepatization 4. Resolution
- 20. PATHOLOGY
- 21. Etiology Bacteria, Fungi, Viruses, and Protozoa Hantaviruses, Metapneumoviruses, the Coronavirus responsible SARS and community-acquired strains MRSA
- 22. • Typical bacterial pathogens – S. pneumoniae, – Haemophilus influenzae, – S. aureus – Gram-negative bacilli such as Klebsiella pneumoniae and Pseudomonas aeruginosa. • Atypical organisms – Mycoplasma pneumoniae – Chlamydia pneumoniae – Legionella spp. – Respiratory viruses
- 23. Epidemiologic Factors Suggesting Possible Causes of Community-Acquired Pneumonia Alcoholism Streptococcus pneumoniae, oral anaerobes, Klebsiella pneumoniae, Mycobacterium tuberculosis COPD and/or smoking Haemophilus influenzae, Pseudomonas aeruginosa, Legionella spp Structural lung disease (e.g., bronchiectasis) P. aeruginosa, Staphylococcus aureus Dementia, stroke, decreased level of consciousness Oral anaerobes, gram-negative enteric bacteria Lung abscess CA-MRSA, oral anaerobes, endemic fungi, M. tuberculosis, Stay in hotel or on cruise ship in previous 2 weeks Legionella spp. Local influenza activity Influenza virus, S. pneumoniae, S. aureus
- 24. Epidemiologic Factors Suggesting Possible Causes of Community-Acquired Pneumonia Exposure to bats or birds H. capsulatum Exposure to birds Chlamydia psittaci Exposure to rabbits Francisella tularensis Exposure to sheep, goats, cats Coxiella burnetii SOURCE: Harrison's Principles of Internal Medicine, 18th Ed.
- 25. SYMPTOMS • Fever • Chills and/or sweats • Cough; nonproductive or productive of mucoid, purulent, or blood- tinged sputum • May be able to speak in full sentences or may be very short of breath • Pleuritic chest pain(If pleura involved) • Nausea, vomiting, and/or diarrhea in 20% • Constitutional symptoms fatigue, headache, myalgias, and arthralgias in 30%
- 26. Physical Examination • Elderly confusion • Use of accessory muscles of respiration & Tachypnea • Increased or decreased tactile fremitus • Percussion note can vary from dull to flat, reflecting underlying consolidated lung and pleural fluid, respectively • Crackles, bronchial breath sounds, and possibly a pleural friction rub
- 27. Differential Diagnosis • The sensitivity and specificity signs & symptoms is 58% and 67% respectively – Acute bronchitis – Acute exacerbations of chronic bronchitis – Heart failure – Pulmonary embolism – Radiation pneumonitis • In addition to a constellation of suggestive clinical features, a demonstrable infiltrate by chest radiograph or other imaging technique, with or without supporting microbiological data diagnosis of pneumonia
- 28. Investigations • Except for the 2% of CAP patients who are admitted to ICU, no data exist to show that treatment directed at a specific pathogen is statistically superior to empirical therapy
- 29. Investigation • Gram's Stain The main purpose of the sputum Gram's stain – To ensure sample is suitable for culture – To be adequate for culture, sample must have >25 neutrophils and <10 squamous epithelial cells/lpf – may also identify S. pneumoniae, S. aureus, and gram-negative bacteria
- 30. Blood Cultures • Only 5–14% of cultures positive • The most frequently isolated pathogen S. pneumoniae • Since all provide pneumococcal coverage, a positive blood culture little, if any, significance • Because of the low yield and the lack of significant impact on outcome, blood cultures are no longer considered de rigueur for all hospitalized CAP patients • Certain high-risk patients—including those with neutropenia, asplenia, or complement deficiencies; chronic liver disease; or severe CAP—should have blood cultured
- 31. Other Tests • Urine Antigen Tests – Pneumococi and Legionella – Sensitivity and specificity >90% – Influenza & RSV • PCR – Legionella, Mycoplasma, Mycobacteria, Chlamydia • Serology – A fourfold rise diagnostic of infection – Fallen out of favour
- 32. Treatment SITE OF CARE There are currently two sets of criteria 1. The Pneumonia Severity Index (PSI) 2. The CURB-65 criteria Time to first antibiotic dose • For patients admitted through the emergency department (ED), the first antibiotic dose should be administered while still in the ED
- 34. CURB-65
- 35. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults
- 36. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults
- 37. Empirical Antibiotic Treatment of Community-Acquired Pneumonia • Outpatients A macrolide [clarithromycin (500 mg PO bid) or azithromycin (500 mg PO once, then 250 mg qd)] or • Doxycycline (100 mg PO bid) Comorbidities or antibiotics in past 3 months: select an alternative from a different class • A respiratory fluoroquinolone [moxifloxacin (400 mg PO qd), gemifloxacin (320 mg PO qd), levofloxacin (750 mg PO qd)] or • A B-lactam [preferred: high-dose amoxicillin (1 g tid) or amoxicillin/clavulanate (2 g bid); • alternatives: ceftriaxone (1–2 g IV qd), cefpodoxime (200 mg PO bid), cefuroxime (500 mg PObid)] Plus A macrolide
- 38. Inpatients, Non-ICU • A Respiratory Fluoroquinolone [moxifloxacin (400 mg PO or IV qd), gemifloxacin (320 mg PO qd),levofloxacin (750 mg PO or IV qd)] OR • A B-lactam [cefotaxime (1–2 g IV q8h), ceftriaxone (1–2 g IV qd), ampicillin (1–2 g IV q4–6h), ertapenem (1 g IV qd in selected patients)] plus • A Macrolide [oral clarithromycin or azithromycin (as listed above for previously healthy patients) or IV azithromycin (1 g once, then 500 mg qd)]
- 39. Inpatients, ICU • A B-lactam [cefotaxime (1–2 g IV q8h), ceftriaxone (2 g IV qd), ampicillin-sulbactam (2 g IV q8h)] plus • Azithromycin or a Fluoroquinolone (as listed above for inpatients, non-ICU)
- 40. Special Concerns If Pseudomonas is a consideration • An Antipneumococcal, Antipseudomonal B-lactam [piperacillin/tazobactam (4.5 g IV q6h), cefepime (1–2 g IV q12h), imipenem (500 mg IV q6h), meropenem (1 g IV q8h)] plus either Ciprofloxacin (400 mg IV q12h) or Levofloxacin (750 mg IV qd) OR • The above B-lactams plus an Aminoglycoside [amikacin (15 mg/kg qd) or tobramycin (1.7 mg/kg • qd)] plus Azithromycin/Antipneumococcal Fluoroquinolone
- 41. Special Concerns If CA-MRSA is a concern • Add linezolid (600 mg IV q12h) OR • Vancomycin (1 g IV q12h).
- 42. When to Switch from intravenous to oral therapy? • Hemodynamically stable and improving • Clinically able to ingest medications • Have a normally functioning gastrointestinal tract
- 43. When to Switch from intravenous to oral therapy? Ramirez JA, Srinath L, Ahkee S, Huang A, Raff MJ. Early switch from intravenous to oral cephalosporins in the treatment of hospitalized patients with community-acquired pneumonia. Arch Intern Med 1995; 155:1273–6.
- 44. Duration of Antibiotic Therapy • Minimum of 5 days • Afebrile for 48–72 h • No more than 1 CAP-associated sign of clinical instability • A longer duration of therapy needed – if initial therapy was not active against the identified pathogen – Complications: extrapulmonary infection, such as meningitis or endocarditis
- 45. When to Discharge? • Patients should be discharged as soon as they are – Clinically stable – Have no other active medical problems – Have a safe environment for continued care
- 46. GENERAL CONSIDERATIONS • Adequate hydration • Oxygen therapy for hypoxemia • Patients with severe CAP who remain hypotensive despite fluid resuscitation may have adrenal insufficiency and may respond to glucocorticoid treatment • Assisted ventilation when necessary
- 47. Ventilation in Pneumonia • Patients with hypoxemia or respiratory distress should receive a cautious trial of non- invasive ventilation unless immediate intubation needed – PaO2/FiO2 < 150 – Bilateral alveolar infiltrates • Low-tidal-volume ventilation (6 cm3/kg of ideal body weight) should be used
- 48. Failure to Improve • Nonresponding Pneumonia – Situation in which an inadequate clinical response despite antibiotic treatment – Lack of a clear-cut and validated definition – Re-evaluated at about day 3 (sooner if condition is worsening)
- 49. Failure to Improve • Lack of Response – Correct drug at the wrong dose or frequency – Nosocomial superinfections—both pulmonary and extrapulmonary – Resistant,unsuspected pathogen, or a sequestered focus ( lung abscess or empyema) – Missed diagnosis • In all cases of delayed response or deteriorating condition, the patient must be carefully reassessed and appropriate studies initiated
- 50. Complications • Respiratory Failure • Lung abscess • Complicated Pleural Effusion • Metastatic infection, (e.g., Brain abscess or Endocarditis) • Shock – Multiorgan failure – Coagulopathy – Exacerbation of Comorbid Illnesses
- 51. Follow Up • Fever and leukocytosis resolve in 2–4 days • Other physical findings may persist • Chest radiograph requires 4–12 weeks to clear • Follow-up radiograph advised after 4–6 weeks If relapse or recurrence, particularly in the same lung segment occurs, the possibility of an underlying neoplasm must be considered
- 52. Prognosis • Young patients without comorbidity recover fully in 2 weeks • Mortality rate for the outpatient <1% • In-hospital mortality rate is 10% with 50% deaths directly attributable to pneumonia
- 53. Prevention • Smoking Cessation • Vaccination
- 54. Pneumococcal polysaccharide vaccine • All persons 65 years of age • Current smoker • Chronic cardiovascular, pulmonary, renal, or liver disease • Diabetes mellitus • Alcoholism • Asplenia • Immunocompromising conditions • Long-term care facility residents
- 55. Inactivated Influenza Vaccine • All persons 50 years &above • Household contacts • Health care providers • Children 6–23 months of age • Chronic cardiovascular or pulmonary disease (including asthma) • • Chronic metabolic disease (including diabetes mellitus) • Renal dysfunction • Hemoglobinopathies • Immuno-compromised conditions • Compromised respiratory function or increased aspiration risk • Pregnancy • Residence in a long-term care facility • Aspirin therapy in persons< 18 years of age
- 56. References: •Harrison’s Principles of Internal Medicine, 18th edition, Anthony S. Fauci, MD, Eugene Braunwald, MD, Dennis L. Kasper, MD, Stephen L. Hauser, MD, Dan L. Longo, MD, J. Larry Jameson, MD, PhD, Joseph Loscalzo, MD, PhD •Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired •Pneumonia in Adults Lionel A. Mandell et al, Clinical Infectious Diseases 2007; 44:S27–72 2007 by the Infectious Diseases Society of America •Robbins and Cotran Pathologic Basis of Disease 7th Ed. •Current Diagnosis Treatment in Pulmonary Medicine 2008. •Aspiration Pneumonitis and Aspiration Pneumonia Paul E. Marik, M.B., B.Ch. N Engl J Med 2001; 344:665-671 March 1, 2001 •Crofton and Douglas’s Respiratiory Diseases 5th Edition S.Anthony, S. Douglas
- 57. Thank You!
Notas do Editor
- On inspection no nasal flaring anatomic abnormality of upper airways
- Esr unit
- Why severe pnemonia
- subscript
- Critical care setting internist Behaviourist’s classification Difficult pnemonia Easy pnemonia manged on oPD basis manged even by family physician Most common cause of LRTI. Anatomist classification:Lobar, segmental subsegmental broncho pneumonia Microbiological classification
- HCAP= Healthcare-associated pneumonia can be defined as pneumonia in a patient with at least one of the following risk factors: hospitalization in an acute care hospital for two or more days in the last 90 days; residence in a nursing home or long-term care facility in the last 90 days receiving outpatient intravenous therapy (like antibiotics or chemotherapy) within the past 30 days receiving home wound care within the past 30 days attending a hospital clinic or dialysis center in the last 30 days having a family member with known multi-drug resistant pathogens Pneumonia vs Pneumonitis
- Critical care setting internist Behaviourist’s classification Difficult pnemonia Easy pnemonia manged on oPD basis manged even by family physician Most common cause of LRTI. Anatomist classification:Lobar, segmental subsegmental broncho pneumonia Microbiological classification
- The combination of an unprotected airway (e.g., in patients with alcohol or drug overdose or a seizure disorder) and significant gingivitis constitutes the major risk factor. Anaerobic pneumonias are often complicated by abscess formation and significant empyemas or parapneumonic effusion
- Pneumonia results from the proliferation of microbial pathogens at the alveolar level and the host's response to those pathogens. aspiration from the oropharynx. sleep (especially in the elderly) decreased levels of consciousness. hematogenous spread (e.g., from tricuspid endocarditis) or by contiguous extension from an infected pleural or mediastinal space.
- hairs and turbinates of the nares Branching architecture of the bracheobronchial tree Mucociliary clearance and local antibacterial factors either clear or kill the potential pathogen. gag reflex and the cough mechanism normal flora adhering to mucosal cells of the oropharynx resident alveolar macrophages Macrophages are assisted by local proteins (e.g., surfactant proteins A and D) that have intrinsic opsonizing properties or antibacterial or antiviral activity
- Alveolar capillary leakerythrocyteshemoptysis
- grayThis phase corresponds with successful containment of the infection and improvement in gas exchange been described best for lobar pneumococcal pneumonia and may not apply to pneumonias of all etiologies, especially viral or Pneumocystis pneumonia Edema or Congesion ( proteinaceous exudate—and often of bacteria—in the alveoli) Red hepatization ( presence of erythrocytes in the neutrophil influx is more important from the standpoint of host defense) Gray hepatization( no new erythrocytes are extravasating, and those already present have been lysed and degraded,neutrophil is the predominant cell, fibrin deposition abundant, and bacteria disappeared). Resolution( macrophage reappears as thedominant cell type and the debris of neutrophils, bacteria, and fibrin has been cleared)
- Foci of bronchopneumonia are consolidated areas of acute suppurative inflammation. The consolidation may be patchy through one lobe but is more often multilobar and frequently bilateral and basal because of the tendency of secretions to gravitate into the lower lobes Because of the microaspiration mechanism, a bronchopneumonia pattern is most common in nosocomial pneumonias, whereas a lobar pattern is more common in bacterial CAP
- , the coronavirus responsible for severe acute respiratory syndrome (SARS),
- such as influenza viruses, adenoviruses, and respiratory syncytial viruses. Atypical organisms Cannot be cultured on standard media, Not stainable by Gram stain Resistant to all -lactam agen
- cardiac disease may suggest worsening pulmonary edema, while underlying carcinoma may suggest lung injury secondary to irradiation. Occasionally, radiographic results suggest an etiologic diagnosis. For example, pneumatoceles suggest infection with S. aureus, and an upperlobe cavitating lesion suggests tuberculosis. CT is rarely necessary but may be of value in a patient with suspected postobstructive pneumonia caused by a tumor or foreign body Presence of a parenchymal infiltrate on chest radiograph distinguishes pneumonia from acute bronchitis
- ) by their characteristic appearance INVESTIGATIONS
- Amplification of a microorganism's DNA or RNA bacterial load documented by PCR the time required to obtain a final result for the convalescent-phase sample
- Patients in classes 4 and 5 should be admitted to the hospital, while those in class 3 should ideally be admitted to an observation unit until a further decision can be made.
- PSI is less practical in a busy emergency room While the CURB-65 criteria are easily remembered, they have not been studied as extensively.
- ICU admission decision. 7. Direct admission to an ICU is required for patients with septic shock requiring vasopressors or with acute respiratory failure requiring intubation and mechanical ventilation. (Strong recommendation; level II evidence.) 8. Direct admission to an ICU or high-level monitoring unit is recommended for patients with 3 of the minor criteria for severe CAP listed in table 4.
- Table 6 source
- Since the physician rarely knows the etiology of CAP at the outset of treatment, initial therapy is usually empirical and is designed to cover the most likely pathogens joint statements from the IDSA and the ATS Therapy with a macrolide or a fluoroquinolone within the previous 3 months is associated with an increased likelihood of infection with a resistant strain of S. pneumoniae. For this reason, a fluoroquinolone-based regimen should be used for patients recently given a macrolide, and vice versa
- synergistic antibacterial effect
- Initially, Ramirez et al. [268] defined a set of criteria for an early switch from intravenous to oral therapy (table 10). In general, as many as two-thirds of all patients have clinical improvement and meet criteria for a therapy switch in the first 3 days, and most non-ICU patients meet these criteria by day 7.
- Inpatient observation while receiving oral therapy is not necessary.
- Patients with CAP who have persistent septic shock despite adequate fluid resuscitation should be considered for treatment with drotrecogin alfa activated within 24 h of admission
- Finally, nonresolving or slow-resolving pneumonia has been10 days of iv antibiotics used to refer to the conditions of patients who present with persistence of pulmonary infiltrates 130 days after initial pneumonia- like syndrome [298]. As many as 20% of these patients will be found to have diseases other than CAP when carefully evaluated [295
- Gm stain culture, cxr blood count culture urine rutine culture These studies may include such diverse procedures as CT and bronchoscopy.
- Respiratory Failure, complicated pleural effusion light complicated simple(krishna dai\) Shock and Multiorgan failure Coagulopathy Exacerbation of Comorbid Ilnesses. metastatic infection, lung abscess, and complicated pleural effusion Metastatic infection (e.g., brain abscess or endocarditis), although unusual, deserves immediate attention by the physician, with a detailed workup and proper treatment. Lung abscess may occur in association with aspiration or with infection caused by a single CAP pathogen such as CA-MRSA, P. aeruginosa, or (rarely) S. pneumoniae A significant pleural effusion should be tapped for both diagnostic and therapeutic purposes. If the fluid has a pH of <7, a glucose level of <2.2 mmol/L, and a lactate dehydrogenase concentration of >1000 U/L or if bacteria are seen or cultured, then the fluid should be drained; a chest tube is usually required. A significant pleural effusion should be tapped for both diagnostic and therapeutic purposes. If the fluid has a pH of <7, a glucose level of <2.2 mmol/L, and a lactate dehydrogenase concentration of >1000 U/L or if bacteria are seen or cultured, then the fluid should be drained; a chest tube is usually required
- Fever and leukocytosis resolve within 2–4 days Other physical findings may persist. Chest radiographic require 4–12 weeks to clear, with the speed of clearance depending on the patient's age and underlying lung disease. Patients may be discharged from the hospital once their clinical conditions are stable, follow-up radiograph can be done ~4–6 weeks later If relapse or recurrence is documented, particularly in the same lung segment, the possibility of an underlying neoplasm must be considered.
- Crofton