Clinical Ophthamology: A Systematic Approach by JACK KANSKI & BRAD BOWLING. 7th Edition
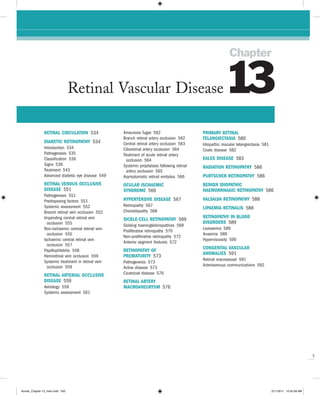
- 1. Chapter Retinal Vascular Disease 13 RETINAL CIRCULATION 534 Amaurosis fugax 562 PRIMARY RETINAL Branch retinal artery occlusion 562 TELANGIECTASIA 580 DIABETIC RETINOPATHY 534 Central retinal artery occlusion 563 Idiopathic macular telangiectasia 581 Introduction 534 Cilioretinal artery occlusion 564 Coats disease 582 Pathogenesis 535 Treatment of acute retinal artery Classification 536 occlusion 564 EALES DISEASE 583 Signs 536 Systemic prophylaxis following retinal RADIATION RETINOPATHY 586 Treatment 543 artery occlusion 565 Advanced diabetic eye disease 549 Asymptomatic retinal embolus 566 PURTSCHER RETINOPATHY 586 RETINAL VENOUS OCCLUSIVE OCULAR ISCHAEMIC BENIGN IDIOPATHIC DISEASE 551 SYNDROME 566 HAEMORRHAGIC RETINOPATHY 586 Pathogenesis 551 Predisposing factors 551 HYPERTENSIVE DISEASE 567 VALSALVA RETINOPATHY 588 Systemic assessment 552 Retinopathy 567 LIPAEMIA RETINALIS 588 Branch retinal vein occlusion 552 Choroidopathy 568 Impending central retinal vein SICKLE-CELL RETINOPATHY 569 RETINOPATHY IN BLOOD occlusion 555 DISORDERS 589 Sickling haemoglobinopathies 569 Non-ischaemic central retinal vein Leukaemia 589 Proliferative retinopathy 570 occlusion 555 Anaemia 589 Non-proliferative retinopathy 572 Ischaemic central retinal vein Hyperviscosity 590 Anterior segment features 572 occlusion 557 CONGENITAL VASCULAR Papillophlebitis 558 RETINOPATHY OF ANOMALIES 591 Hemiretinal vein occlusion 559 PREMATURITY 573 Systemic treatment in retinal vein Retinal macrovessel 591 Pathogenesis 573 occlusion 559 Arteriovenous communications 592 Active disease 573 RETINAL ARTERIAL OCCLUSIVE Cicatricial disease 576 DISEASE 559 RETINAL ARTERY Aetiology 559 MACROANEURYSM 576 Systemic assessment 561 Q Kanski_Chapter 13_main.indd 533 2/11/2011 10:42:58 AM
- 2. Clinical Ophthalmology 534 A S y S T e m AT I C A P P RoAC H Capillaries Retinal capillaries supply the inner two-thirds of the retina, with the outer third being supplied by the choriocapillaris. The inner capillary network (plexus) is located in the ganglion cell layer, with an outer plexus in the inner nuclear layer. Capillary-free zones are present around arterioles (Fig. 13.1A) and at the fovea (foveal avascular zone – FAZ). Retinal capillaries are devoid of smooth muscle and elastic tissue and their walls consist of the following (Fig. 13.1B): 1. Endothelial cells form a single layer on the basement membrane and are linked by tight junctions that form A the inner blood–retinal barrier. 2. The basement membrane lies beneath the endo- thelial cells with an outer basal lamina enclosing pericytes. 3. Pericytes lie external to endothelial cells and have multiple pseudopodial processes that envelop the capillaries. The pericytes have contractile properties and are thought to participate in autoregulation of the microvascular circulation. Venous system Retinal venules and veins drain blood from the capillaries. 1. Small venules are larger than capillaries but have a B similar structure. 2. Larger venules contain smooth muscle and merge to Fig. 13.1 Normal retinal capillary bed. (A) Periarteriolar form veins. capillary-free zone – flat preparation of Indian ink-injected 3. Veins contain a small amount of smooth muscle retina; (B) endothelial cells with elongated nuclei and and elastic tissue in their walls and are relatively pericytes with rounded nuclei – trypsin digest preparation distensible. They gradually expand in diameter (Courtesy of J Harry and G Misson, from Clinical Ophthalmic Pathology, Butterworth-Heinemann 2001) as they pass posteriorly towards the central retinal vein. DIABETIC RETINOPATHY Introduction RETINAL CIRCULATION Prevalence Arterial system The reported prevalence of diabetic retinopathy (DR) varies substantially between studies, even amongst con- 1. The central retinal artery is an end artery that enters temporary diabetic populations in the same country, but the optic nerve approximately 1 cm behind the globe is probably up to 40%. It is more common in type 1 dia- and is composed of the following three anatomical betes than in type 2 and sight-threatening disease is layers: present in up to 10%. Proliferative diabetic retinopathy a. The intima, the innermost, is composed of a single (PDR) affects 5–10% of the diabetic population; type 1 layer of endothelium resting on a collagenous diabetics are at particular risk with an incidence of about zone. 60% after 30 years. b. The internal elastic lamina separates the intima from the media. Risk factors c. The media consists mainly of smooth muscle. d. The adventitia is the outermost and is composed 1. Duration of diabetes is the most important risk factor. of loose connective tissue. In patients diagnosed with diabetes before the age of 2. Retinal arterioles arise from the central retinal artery. 30 years, the incidence of DR after 10 years is 50%, and They contain smooth muscle within their walls, after 30 years 90%. DR rarely develops within 5 years but unlike arteries the internal elastic lamina is of the onset of diabetes or before puberty, but about Q discontinuous. 5% of type 2 diabetics have DR at presentation. It Kanski_Chapter 13_main.indd 534 2/11/2011 10:43:00 AM
- 3. 13 CHAPTeR Retinal Vascular Disease 535 appears that duration is a stronger predictor for pro- liferative disease than for maculopathy. 2. Poor control of diabetes. It has been shown that tight blood glucose control, particularly when instituted early, can prevent or delay the development or pro- gression of DR. However, a sudden improvement in control may be associated with progression of retin- opathy in the near term. Type 1 diabetic patients appear to obtain greater benefit from good control than those with type 2. Raised HbA1c is associated with an increased risk of proliferative disease. 3. Pregnancy is sometimes associated with rapid pro- gression of DR. Predicating factors include greater pre-pregnancy severity of retinopathy, poor pre- pregnancy control of diabetes, control exerted too rapidly during the early stages of pregnancy, and the development of pre-eclampsia and fluid imbalance. The risk of progression is related to the severity of DR in the first trimester. If substantial DR is present, fre- quency of review should reflect the individual risk, and can be up to monthly. Diabetic macular oedema A usually resolves spontaneously after pregnancy and need not be treated if it develops in later pregnancy. 4. Hypertension, which is very common in patients with type 2 diabetes, should be rigorously controlled (<140/80). Tight control appears to be particularly beneficial in type 2 diabetics with maculopathy. Car- diovascular disease and previous stroke are also predictive. 5. Nephropathy, if severe, is associated with worsening of DR. Conversely, treatment of renal disease (e.g. renal transplantation) may be associated with impro- vement of retinopathy and a better response to photocoagulation. 6. Other risk factors include hyperlipidaemia, smoking, cataract surgery, obesity and anaemia. B Pathogenesis DR is predominantly a microangiopathy in which small blood vessels are particularly vulnerable to damage from hyperglycaemia. Direct hyperglycaemic effects on retinal cells are also likely to play a role. 1. Mechanisms of cellular damage include intracellular sorbitol accumulation, oxidative stress due to free radical excess, accumulation of advanced glycation end products and excessive activation of several protein kinase C isoforms. Disruption of ion channel function is an important early feature. 2. Capillaropathy is characterized by death of pericytes (Fig. 13.2A), thickening of capillary basement mem- brane, loss of vascular smooth muscle cells and C proliferation of endothelial cells. Haematological/ rheological changes such as abnormalities of erythro- Fig. 13.2 The capillary bed in diabetic retinopathy. (A) Capillary closure with adjacent dilated and elongated capillaries – flat cytes and leucocytes, increased platelet stickiness, preparation of Indian ink-injected retina; (B) degenerate and increased plasma viscosity may also contribute. pericytes which are eosinophilic – trypsin digest Capillary dysfunction manifests with leakage and preparation; (C) new capillaries (arrows) on the inner retinal occlusion. surface growing from vessels in relation to non-perfused 3. Neovascularization is caused by capillary non- areas – flat preparation of Indian ink-injected retina perfusion (Fig. 13.2B) which leads to retinal hypoxia (Courtesy of J Harry and G Misson, from Clinical Ophthalmic Pathology, which may progress to neovascularization extending Butterworth-Heinemann 2001) Q preretinally (PDR) and intraretinally; intraretinal Kanski_Chapter 13_main.indd 535 2/11/2011 10:43:02 AM
- 4. Clinical Ophthalmology 536 A S y S T e m AT I C A P P RoAC H microvascular abnormalities (IRMA) are shunts that ILM NFL haem. run within the retina from arterioles to venules. New vessel growth is thought to be caused by an imbalance NFL between the elaboration of angiogenic and anti- GCL IPL angiogenic factors, putatively in an attempt to INL re-vascularize hypoxic retina. Many angiogenic stimulators have been identified; vascu- Oedema lar endothelial growth factor (VEGF), especially VEGF-A, OPL H.Ex. Cystoid spaces appears to be of particular importance. Others include platelet-derived growth factor and hepatocyte growth ONL Dot haem factor. Similarly, several endogenous inhibitors of angio- R & CL RPE genesis have also been reported such as endostatin, angi- ostatin and pigment epithelium-derived factor. It has BrM been hypothesized that a key determinant of the activity of retinopathy is the net balance between VEGF and Fig. 13.3 Location of lesions in background diabetic endostatin. retinopathy Classification layer) frequently in relation to areas of capillary non- The classification used in the Early Treatment Diabetic perfusion (Fig. 13.4B). Loss of pericytes may also lead to Retinopathy Study (the modified Airlie House classifica- endothelial cell proliferation with the formation of ‘cel- tion) is widely used internationally. An abbreviated lular’ microaneurysms (Fig. 13.4C). Microaneurysms may version is set out in Table 13.1, in conjunction with man- leak plasma constituents into the retina as a result of agement guidelines. The following descriptive categories breakdown in the blood–retinal barrier, or become throm- are also in widespread use in clinical practice: bosed (Fig. 13.4D). 1. Background diabetic retinopathy (BDR) is character- 1. Signs. Tiny red dots, often initially temporal to ized by microaneurysms, dot and blot haemorrhages the fovea; tend to be the earliest signs of DR and exudates. Generally the earlier signs of DR, (Fig. 13.4E). They may be indistinguishable from although persisting as more advanced lesions appear. dot haemorrhages. 2. Diabetic maculopathy strictly refers to the presence 2. Fluorescein angiography (FA). Early frames show of any retinopathy at the macula, but commonly tiny hyperfluorescent dots (Fig. 13.4F), representing reserved for significant changes, particularly vision- non-thrombosed microaneurysms, typically more threatening oedema and ischaemia. numerous than visible clinically. Late frames show 3. Preproliferative diabetic retinopathy (PPDR) mani- diffuse hyperfluorescence due to leakage. fests cotton wool spots, venous changes, intraretinal microvascular anomalies (IRMA) and often deep Retinal haemorrhages retinal haemorrhages. PPDR indicates progressive retinal ischaemia, with a heightened risk of progres- Figure 13.5A is a histological section showing the location sion to retinal neovascularization. of blood. 4. PDR is characterized by neovascularization on or 1. Retinal nerve fibre layer haemorrhages arise from the within one disc diameter of the disc (NVD) and/or larger superficial pre-capillary arterioles and because new vessels elsewhere (NVE) in the fundus. of the architecture of the retinal nerve fibres are flame- 4. Advanced diabetic eye disease is characterized by shaped (Fig. 13.5B). tractional retinal detachment, significant persistent 2. Intraretinal haemorrhages arise from the venous end vitreous haemorrhage and neovascular glaucoma. of capillaries and are located in the compact middle layers of the retina with a resultant red ‘dot/blot’ con- figuration (Fig. 13.5C). Signs 3. Deeper dark round haemorrhages represent haemor- rhagic retinal infarcts and are located within the Figure 13.3 shows the location of lesions in background middle retinal layers (Fig. 13.5D). The extent of diabetic retinopathy. involvement is a significant marker of the likelihood of progression to retinal neovascularization. Microaneurysms Exudates Microaneurysms are localized out-pouchings, mainly sac- Exudates, sometimes termed ‘hard’ exudates to distin- cular, of the capillary wall that may form either by focal guish from the older term of ‘soft’ exudates for cotton dilatation of the capillary wall where pericytes are absent, wool spots, are caused by chronic localized retinal oedema or by fusion of two arms of a capillary loop (Fig. 13.4A). and develop at the junction of normal and oedematous Q Most develop in the inner capillary plexus (inner nuclear retina. They are composed of lipoprotein and lipid-filled Kanski_Chapter 13_main.indd 536 2/11/2011 10:43:03 AM
- 5. 13 CHAPTeR Retinal Vascular Disease 537 Table 13.1 Abbreviated Early Treatment Diabetic Retinopathy Study classification of diabetic retinopathy Category/description Management Non-proliferative diabetic retinopathy (NPDR) No DR Review in 12 months Very mild Review most patients in 12 months Microaneurysms only Mild Review range 6–12 months, depending on severity of Any or all of: microaneurysms, retinal haemorrhages, signs, stability, systemic factors, and patient’s personal exudates, cotton wool spots, up to the level of moderate circumstances NPDR. No IRMA or significant beading Moderate Review in approximately 6 months • Severe retinal haemorrhages (more than ETDRS PDR in up to 26%, high-risk PDR in up to 8% within a year standard photograph 2A: about 20 medium-large per quadrant) in 1–3 quadrants or mild intraretinal microvascular abnormalities (IRMA) • Significant venous beading can be present in no more than 1 quadrant • Cotton wool spots commonly present Severe Review in 4 months The 4-2-1 rule; one or more of: PDR in up to 50%, high-risk PDR in up to 15% within a year • Severe haemorrhages in all 4 quadrants • Significant venous beading in 2 or more quadrants • Moderate IRMA in 1 or more quadrants Very severe Review in 2–3 months Two or more of the criteria for severe High-risk PDR in up to 45% within a year Proliferative diabetic retinopathy (PDR) Mild-moderate Treatment considered according to severity of signs, New vessels on the disc (NVD) or new vessels elsewhere stability, systemic factors, and patient’s personal (NVE), but extent insufficient to meet the high-risk criteria circumstances such as reliability of attendance for review. If not treated, review in up to 2 months High-risk Treatment advised – see text • New vessels on the disc (NVD) greater than ETDRS Should be performed immediately when possible, and standard photograph 10A (about 1 3 disc area) certainly same day if symptomatic presentation with good • Any NVD with vitreous or preretinal haemorrhage retinal view • NVE greater than 1 2 disc area with vitreous or preretinal haemorrhage (or haemorrhage with presumed obscured NVD/E) Advanced diabetic eye disease See text See text for description macrophages located mainly within the outer plexiform • Chronic leakage leads to enlargement of the layer (Fig. 13.6A). Hyperlipidaemia may increase the like- exudates and the deposition of cholesterol (Fig. lihood of exudate formation. 13.6E). 2. FA shows hypofluorescence due to blockage of back- 1. Signs ground choroidal and retinal capillary fluorescence. • Waxy yellow lesions with relatively distinct margins, often arranged in clumps and/or rings at Diabetic macular oedema the posterior pole, typically surrounding leaking microaneurysms (Fig. 13.6B). Diabetic maculopathy (foveal oedema, exudates or ischae- • With time number and size tend to increase (Fig. mia) is the most common cause of visual impairment 13.6C), and the fovea may be threatened or involved in diabetic patients, particularly type 2. Diffuse retinal (Fig. 13.6D). oedema is caused by extensive capillary leakage, and • When leakage ceases, exudates absorb spontane- localized oedema by focal leakage from microaneurysms ously over a period of months or years, either into and dilated capillary segments. The fluid is initially the healthy surrounding capillaries or by phagocy- located between the outer plexiform and inner nuclear layers; later it may also involve the inner plexiform and Q tosis of their lipid content. Kanski_Chapter 13_main.indd 537 2/11/2011 10:43:04 AM
- 6. A B C D E F Fig. 13.4 Retinal microaneurysm. (A) Two arms of a capillary loop are not yet fused to become a microaneurysm – flat preparation of Indian ink-injected retina; (B) an area of capillary non-perfusion and adjacent microaneurysms – flat preparation of Indian ink-injected retina; (C) microaneurysm with endothelial cell proliferation (cellular microaneurysm) Q – trypsin digest preparation; (D) thrombosed microaneurysm – PAS and haematoxylin stain; (E) microaneurysms at the posterior pole; (F) FA shows scattered hyperfluorescent spots in the posterior fundus (Courtesy of J Harry and G Misson, from Clinical Ophthalmic Pathology, Butterworth-Heinemann 2001 – fig. A; J Harry – figs B–D) Kanski_Chapter 13_main.indd 538 2/11/2011 10:43:12 AM
- 7. 13 CHAPTeR Retinal Vascular Disease 539 A B C D Fig. 13.5 Retinal haemorrhages. (A) Histology shows blood lying diffusely in the retinal nerve fibre and ganglion cell layers and as globules in the outer layers; (B) retinal nerve fibre layer haemorrhages; (C) deep dot and blot haemorrhages; (D) deep dark haemorrhages (Courtesy of J Harry and G Misson, from Clinical Ophthalmic Pathology, Butterworth-Heinemann 2001 – fig. A; Moorfields Eye Hospital – fig. C) nerve fibre layers, until eventually the entire thickness of 3. OCT shows retinal thickening and, if present, cystoid the retina becomes oedematous. With further accumula- spaces (Fig. 13.7B). OCT is also useful in assessing tion of fluid the fovea assumes a cystoid appearance response to treatment. (cystoid macular oedema – CMO). 1. Signs. Retinal thickening is best detected by slit-lamp Focal maculopathy biomicroscopy with a contact lens, though high- 1. Signs. Well-circumscribed retinal thickening associ- resolution non-contact lenses are also effective. ated with complete or incomplete rings of exudates 2. FA shows diffuse late hyperfluorescence due to retinal (Fig. 13.8A). capillary leakage, and may have a flower-petal pattern 2. FA shows late, focal hyperfluorescence due to leakage, Q if CMO is present (Fig. 13.7A). and good macular perfusion (Fig. 13.8B). Kanski_Chapter 13_main.indd 539 2/11/2011 10:43:24 AM
- 8. Clinical Ophthalmology 540 A S y S T e m AT I C A P P RoAC H A B C D Fig. 13.6 Exudates. (A) Histology shows irregular eosinophilic deposits mainly in the outer plexiform layer; (B) small exudates and microaneurysms; (C) incomplete ring of exudates and a few small haemorrhages; (D) exudates involving the fovea; (E) plaque of exudates at the macula E associated with cholesterol deposition Q (Courtesy of J Harry – fig. A) Kanski_Chapter 13_main.indd 540 2/11/2011 10:43:37 AM
- 9. 13 CHAPTeR Retinal Vascular Disease 541 A A B Fig. 13.7 Macular oedema. (A) FA shows diffuse hyperfluorescence with a central flower-petal configuration due to CMO; (B) OCT shows retinal thickening and cystoid spaces (Courtesy of Moorfields Eye Hospital – fig. A; Oxford Eye Hospital – fig. B) Diffuse maculopathy 1. Signs. Diffuse retinal thickening, which may be asso- ciated with cystoid changes. Landmarks are obliter- B ated by severe oedema which may render localization of the fovea impossible (Fig. 13.9A). Fig. 13.8 Focal diabetic maculopathy. (A) A ring of hard 2. FA shows late diffuse hyperfluorescence (Fig. 13.9B) exudates temporal to the macula; (B) FA late phase shows which may assume a central flower-petal pattern if focal area of hyperfluorescence due to leakage CMO is present. corresponding to the centre of the exudate ring Ischaemic maculopathy 1. Signs are variable and the macula may look relatively normal despite reduced visual acuity. In other cases • Exudates within 500 µm of the centre of the macula, PPDR may be present (Fig. 13.10A). if associated with retinal thickening (which may be 2. FA shows capillary non-perfusion at the fovea (an outside the 500 µm – Fig. 13.11, upper right). enlarged FAZ) and frequently other areas of capillary • Retinal thickening one disc area (1500 µm) or larger, non-perfusion at the posterior pole and periphery any part of which is within one disc diameter of the (Fig. 13.10B). centre of the macula (Fig. 13.11, lower centre). Clinically significant macular oedema Cotton wool spots Clinically significant macular oedema (CSMO) was defined in the ETDRS (Fig. 13.11): Cotton wool spots are composed of accumulations of neu- ronal debris within the nerve fibre layer. They result from • Retinal thickening within 500 µm of the centre of the disruption of nerve axons, the swollen ends of which are Q macula (Fig. 13.11, upper left). known as cytoid bodies, seen on light microscopy as Kanski_Chapter 13_main.indd 541 2/11/2011 10:43:44 AM
- 10. Clinical Ophthalmology 542 A S y S T e m AT I C A P P RoAC H A A B B Fig. 13.9 Diffuse diabetic maculopathy. (A) Dot and blot Fig. 13.10 Ischaemic diabetic maculopathy. (A) Dot and blot haemorrhages; (B) FA late phase shows extensive haemorrhages and cotton wool spots; (B) FA venous phase hyperfluorescence at the posterior pole due to leakage shows hypofluorescence due to capillary non-perfusion at the macula and elsewhere (Courtesy of Moorfields Eye Hospital) globular structures in the nerve fibre layer (Fig. 13.12A). As cotton wool spots heal, debris is removed by autolysis and phagocytosis. 1. Signs. Small, whitish, fluffy superficial lesions which ‘beading’ (focal narrowing and dilatation – Fig. 13.13B) obscure underlying blood vessels and are clinically and ‘sausage-like’ segmentation (Fig. 13.13C). The extent evident only in the post-equatorial retina, where the of the retinal area exhibiting venous changes correlates nerve fibre layer is of sufficient thickness to render well with the likelihood of developing proliferative them visible (Fig. 13.12B). disease. 2. FA shows focal hypofluorescence due to blockage of background choroidal fluorescence, frequently associ- Intraretinal microvascular abnormalities ated with adjacent capillary non-perfusion. Intraretinal microvascular abnormalities (IRMA) are arteriolar-venular shunts that run from retinal arterioles Venous changes to venules, thus bypassing the capillary bed and are there- Venous anomalies seen in ischaemia consist of general- fore often seen adjacent to areas of marked capillary Q ized dilatation and tortuosity, ‘looping’ (Fig. 13.13A), hypoperfusion (Fig. 13.14A). Kanski_Chapter 13_main.indd 542 2/11/2011 10:43:51 AM
- 11. 13 CHAPTeR Retinal Vascular Disease 543 Fovea A Fig. 13.11 Clinically significant macular oedema 1. Signs. Fine, irregular, red intraretinal lines that run from arterioles to venules (Fig. 13.14B), without cross- ing major blood vessels. 2. FA shows focal hyperfluorescence associated with adjacent areas of capillary closure (’dropout’) but without leakage. Arterial changes Subtle retinal arteriolar dilatation may be an early marker of ischaemic dysfunction. When significant ischaemia is present these include peripheral narrowing, silver-wiring and obliteration (Fig. 13.15), similar to the late appearance following a branch retinal artery occlusion. B Proliferative retinopathy Fig. 13.12 Cotton wool spots. (A) Histology shows cytoid bodies in the nerve fibre layer; (B) clinical appearance It has been estimated that over one-quarter of the retina (Courtesy of J Harry – fig. A; K Slowinski – fig. B) must be non-perfused before PDR develops. Although preretinal new vessels may arise anywhere in the retina, they are most commonly seen at the posterior pole. Fibrous tissue, initially fine, gradually develops in asso- ciation as vessels increase in size. Treatment 1. New vessels at the disc (NVD) describes neovascu- Argon laser treatment of clinically significant larization on or within one disc diameter of the optic nerve head (Fig. 13.16A–C). macular oedema 2. New vessels elsewhere (NVE) describes neovascu- 1. Indications larization further away from the disc (Fig. 13.17A and • All eyes with CSMO should be considered for laser B) that may be associated with fibrosis (Fig. 13.17D) if photocoagulation irrespective of the level of visual long-standing. acuity, because treatment reduces the risk of visual 3. New vessels on the iris (NVI), also known as rubeosis loss by 50%. However, options should always be iridis, carry a high likelihood of progression to neo- discussed with the patient, and if visual acuity is vascular glaucoma. good some authorities prefer to recommend careful 4. FA, although not required to make the diagnosis, observation, as macular laser is not without risk, highlights neovascularization during the early phases and oedema sometimes resolves spontaneously. of the angiogram (see Fig. 13.16D) and shows hyper- • Pre-treatment FA is useful to delineate the area fluorescence during the later stages due to intense and extent of leakage, and to detect ischaemic Q leakage of dye from neovascular tissue (Fig. 13.17D). maculopathy (see Fig. 13.10) which carries a poor Kanski_Chapter 13_main.indd 543 2/11/2011 10:44:00 AM
- 12. Clinical Ophthalmology 544 A S y S T e m AT I C A P P RoAC H A B C Fig. 13.13 Venous changes. (A) Looping; (B) beading; (C) severe segmentation prognosis and if severe is a relative contraindica- macula and 500 µm from the temporal margin of tion to treatment. the optic disc. 2. Focal treatment (Fig. 13.18A) • The spot size is 100 µm and exposure time • Burns are applied to microaneurysms and micro- 0.1 second giving a very light intensity burn. vascular lesions in the centre of rings of exudates • Treatment should be lighter if significant macular located 500–3000 µm from the centre of the ischaemia is present. macula. 4. Results. Approximately 70% of eyes achieve stable • The spot size is 50–100 µm and exposure time visual acuity, 15% show improvement and 15% sub- 0.1 second with sufficient power to obtain gentle sequently deteriorate. Since it may take up to 4 months whitening or darkening of the microaneurysm. for the oedema to resolve, re-treatment should not be • Treatment of lesions up to 300 µm from the considered prematurely. centre of the macula may be considered if 5. Poor prognostic factors CSMO persists despite previous treatment and a. Ocular factors include significant macular ischae- visual acuity is less than 6/12. In these cases mia, exudates involving the fovea, diffuse macular a shorter exposure time of 0.05 second is oedema, CMO and severe retinopathy at recommended. presentation. 3. Grid treatment (Fig. 13.18B) b. Systemic factors include uncontrolled hyperten- • Burns are applied to areas of diffuse retinal thick- sion, renal disease, poorly-controlled blood glucose Q ening more than 500 µm from the centre of the (elevated HbA1c levels). Kanski_Chapter 13_main.indd 544 2/11/2011 10:44:03 AM
- 13. 13 CHAPTeR Retinal Vascular Disease 545 A Fig. 13.15 Peripheral arteriolar occlusion b. Micropulse diode laser in which short duration (microseconds) burns are applied to the RPE without significantly affecting the outer retina and choriocapillaris. 2. Intravitreal anti-vascular endothelial growth factor (anti-VEGF) agents. A large multicentre trial (The Diabetic Retinopathy Research Network Laser- Ranibizumab-Triamcinolone Study) recently showed that intravitreal injection of 0.5 mg ranibizumab, initially given monthly for 3 months, with prompt or deferred (≥24 weeks) macular laser had significantly superior visual and OCT outcomes to laser alone in eyes with diabetic macular oedema involving the B fovea. It is likely that intravitreal VEGF inhibitors will play an increasingly prominent role in the treatment Fig. 13.14 Intraretinal microvascular abnormalities. of diabetic retinopathy. (A) Histology shows arteriolar-venular shunt and a few 3. Intravitreal triamcinolone. The study described above microaneurysms within a poorly perfused capillary bed – flat also investigated the effect of intravitreal triamci- preparation of Indian ink-injected retina; phase contrast nolone injection, finding that in pseudophakic eyes microscopy; (B) clinical appearance steroid injection followed by prompt laser may be as (Courtesy of J Harry – fig. A; Moorfields Eye Hospital – fig. B) effective as ranibizumab at improving vision and reducing retinal thickening. However, there was a sig- Other treatments for maculopathy nificant risk of an elevation of intraocular pressure. No corresponding visual benefit above laser was shown Argon laser remains the primary therapeutic modality, for phakic eyes, which also had a substantially but numerous other forms of treatment have shown increased rate of cataract surgery by 2 years. promising results. 4. Pars plana vitrectomy may be indicated when macular 1. Other lasers oedema is associated with tangential traction from a a. Frequency-doubled Nd:YAG laser offers the poten- thickened and taut posterior hyaloid. It has also tial of a less destructive retinal effect than argon, been suggested that some eyes without a taut poste- in which the energy employed is the lowest capable rior hyaloid may benefit from vitrectomy. Clinically, of producing barely visible burns at the level of a taut thickened posterior hyaloid is characterized by the RPE. The ‘Pattern Scan Laser’ (Pascal) uses an increased glistening of the pre-macular vitreous frequency-doubled micropulse YAG in single shot face. FA typically shows diffuse leakage and promi- mode or in a predetermined array of up to 56 shots nent CMO, but OCT is usually the definitive applied in less than a second. This greatly improves assessment. patient comfort as compared with conventional 5. Lipid-lowering drugs may reduce the requirement for Q argon laser. laser treatment, and studies are ongoing. Kanski_Chapter 13_main.indd 545 2/11/2011 10:44:10 AM
- 14. Clinical Ophthalmology 546 A S y S T e m AT I C A P P RoAC H A B C D Fig. 13.16 Disc new vessels. (A) Mild; (B) severe; (C) very severe; (D) FA early phase highlights the vessels (Courtesy of P Gili) 1. Indications. Laser therapy is aimed at inducing the Laser photocoagulation involution of new vessels and thereby preventing for proliferative retinopathy visual loss; see Table 13.1 for specific indications. It should be noted that: The Diabetic Retinopathy Study (DRS) established the • PRP influences only the vascular component of the characteristics of high-risk proliferative disease and fibrovascular process. Eyes in which new vessels investigated the effect of panretinal photocoagulation have regressed leaving only fibrous tissue should (PRP). The benefits demonstrated included: not be re-treated. • If CSMO is also present, laser for this should pref- • Mild NVD with haemorrhage carries a 26% risk of erably be carried out prior to PRP or at the same visual loss, which is reduced to 4% with treatment. session; the intensity and amount of PRP should be • Severe NVD without haemorrhage carries a 26% risk of kept to the lowest level likely to be effective, and visual loss, which is reduced to 9% with treatment. may be spread over multiple sessions; adjunctive • Severe NVD with haemorrhage carries a 37% risk of intravitreal steroid or an anti-VEGF agent may visual loss, which is reduced to 20% with treatment. improve the outcome in this situation. Q • Severe NVE with haemorrhage carries a 30% risk of 2. Informed consent. Patients should be advised that visual loss, which is reduced to 7% with treatment. PRP may occasionally cause visual field defects of Kanski_Chapter 13_main.indd 546 2/11/2011 10:44:26 AM
- 15. 13 CHAPTeR Retinal Vascular Disease 547 A B C D Fig. 13.17 New vessels elsewhere. (A) Mild; (B) severe; (C) associated with fibrosis; (D) FA late phase shows capillary non- perfusion and hyperfluorescence due to leakage (Courtesy of C Barry – fig. D) sufficient severity to legally preclude driving a motor inadvertently photocoagulate the posterior pole vehicle; they should also be made aware that there is through the former. some risk to central vision, and that night and colour b. Duration of the burn is 0.05–0.1 second. vision may be affected. c. Power should be sufficient to produce only a light 3. Laser settings intensity burn (Fig. 13.19A), with the intention of a. Spot size depends on the contact lens used. With stimulating the retinal pigment epithelium rather the Goldmann lens spot size is set at 200–500 µm, than ablating the retina (Fig. 13.19B). but with a panfundoscopic-type lens it is set at 4. Initial treatment involves 1500–2000 burns in a scatter 100–300 µm because of induced magnification pattern extending from the posterior fundus to cover (varies with exact lens used). The main effect is the peripheral retina in one or more sessions; PRP related to surface area of retina treated rather completed in a single session carries a slightly higher than the number of burns; a small variation in the risk of complications. The amount of treatment it is size of the laser burn therefore has a pronounced possible to apply during one session is governed by effect on area treated (area = πr2). In the beginner’s the patient’s pain threshold; discomfort tends to be Q hands, a panfundoscopic lens is perhaps safer least at the posterior pole and greatest in the periphery than the Goldmann, as it is more difficult to and over the horizontal neurovascular bundle, and Kanski_Chapter 13_main.indd 547 2/11/2011 10:44:30 AM
- 16. Clinical Ophthalmology 548 A S y S T e m AT I C A P P RoAC H A A B Fig. 13.19 (A) Appropriate laser burns; (B) appearance several weeks after completion of treatment (Courtesy of C Barry – fig. B) c. Step 3. Nasal to the disc (Fig. 13.22A and B); com- pletion of posterior pole treatment (Fig. 13.22C). Many practitioners leave two disc diameters untreated at the nasal side of the disc, to preserve B paracentral field. d. Step 4. Peripheral treatment (Fig. 13.23A and B) Fig. 13.18 Laser photocoagulation for clinically significant until completion (Fig. 13.23C). macular oedema. (A) Appearance several weeks following In very severe PDR it is advisable to treat the inferior focal laser photocoagulation shows laser scars and fundus first, since any vitreous haemorrhage will absence of hard exudates; (B) appearance immediately gravitate inferiorly and obscure this area, precluding following grid laser photocoagulation further treatment. 5. Follow-up is after 4–6 weeks. In eyes with severe NVD, 3000 or more burns may be required. Occasion- tends to worsen with successive sessions. Topical ally complete elimination of NVD may be difficult but anaesthesia is adequate in most patients, although once the tips of the vessels start to undergo fibrosis peribulbar or sub-Tenon anaesthesia may be neces- they pose much less of a threat to vision. sary. A suggested treatment sequence is as follows: 6. Signs of involution consist of regression of neovascu- a. Step 1. Close to the disc (Fig. 13.20A); below the larization leaving ‘ghost’ vessels or fibrous tissue (Fig. inferior temporal arcades (Fig. 13.20B and C). 13.24), decrease in venous changes, absorption of b. Step 2. Protective barrier around the macula (Fig. retinal haemorrhages and disc pallor. In most eyes, 13.21A) to prevent inadvertent treatment of the once the retinopathy is quiescent, stable vision is fovea; above the superotemporal arcade (Fig. maintained. In a few eyes, recurrences occur despite 13.21B and C). If necessary, the retina just inside an initial satisfactory response, and patients should Q the arcades can be treated. remain under observation. Kanski_Chapter 13_main.indd 548 2/11/2011 10:44:39 AM
- 17. 13 CHAPTeR Retinal Vascular Disease 549 A B C Fig. 13.20 PRP technique – step 1 A A B C Fig. 13.21 PRP technique – step 2 A B C Fig. 13.22 PRP technique – step 3 B Fig. 13.24 Treatment of proliferative diabetic retinopathy. (A) Severe proliferative disease; (B) 3 months later new vessels have regressed and there is residual fibrosis at the disc (Courtesy of S Milewski) encourage the resolution of persistent vitreous haemor- A B C rhage, avoiding vitrectomy in some patients. Fig. 13.23 PRP technique – step 4 Advanced diabetic eye disease Advanced diabetic eye disease is a serious vision- 7. Treatment of recurrences may involve further laser threatening complication of DR that occurs in patients in photocoagulation filling in any gaps between previous whom treatment has been inadequate or unsuccessful. laser scars or utilizing indirect laser to treat very Occasionally, advanced disease is evident at, or prompts, peripheral retina. presentation. 8. Fibrosis associated with neovascularization (see Fig. 13.17C) is important, since significant fibrous prolif- eration, although less likely to bleed carries an Diagnosis increased risk of tractional retinal detachment. 1. Haemorrhage may be preretinal (retrohyaloid, Fig. 13.25A), intragel (Fig. 13.25B) or both. Intragel haem- orrhages usually take longer to clear than preretinal VEGF inhibition for proliferative retinopathy haemorrhages because the former are usually the Intravitreal anti-VEGF injection is likely to have an result of a more extensive bleed. In some eyes, altered increasing role in the treatment of PDR, probably as an blood becomes compacted on the posterior vitreous Q adjunct to laser. A particular indication may be to face to form an ‘ochre membrane’. Patients should Kanski_Chapter 13_main.indd 549 2/11/2011 10:44:42 AM
- 18. Clinical Ophthalmology 550 A S y S T e m AT I C A P P RoAC H A B C D Fig. 13.25 Advanced diabetic eye disease. (A) Retrohyaloid haemorrhage; (B) intragel haemorrhage; (C) tractional retinal detachment; (D) rubeosis iridis (Courtesy of C Barry – figs A and D) be warned that bleeding may be precipitated by severe In the absence of rubeosis iridis, vitrectomy has tradi- physical exertion or straining, hypoglycaemia and tionally been considered within 3 months of the initial direct ocular trauma. Ultrasonography is used in eyes vitreous haemorrhage in type 1 diabetics and in most with dense vitreous haemorrhage to detect the possi- cases of bilateral haemorrhage. However, the availa- bility of associated retinal detachment (see Fig. 17.1D). bility of intravitreal anti-VEGF injections may modify 2. Tractional retinal detachment (Fig. 13.25C) is caused this approach. by progressive contraction of fibrovascular membranes 2. Progressive tractional RD threatening or involving over areas of vitreoretinal attachment. Posterior vitre- the macula must be treated without delay (Fig. 13.26A). ous detachment in eyes with PDR is often incomplete However, extramacular tractional detachments may due to the strong adhesions between cortical vitreous be observed, since they often remain stationary for and areas of fibrovascular proliferation (see Ch. 16). prolonged periods. 3. Tractional retinoschisis with or without retinal 3. Combined tractional and rhegmatogenous RD detachment may also occur. should be treated urgently, even if the macula is not 4. Rubeosis iridis (iris neovascularization – Fig. 13.25D) involved, because subretinal fluid is likely to spread may occur in eyes with PDR, and if severe may lead quickly to involve the macula. to neovascular glaucoma. Rubeosis is particularly 4. Premacular subhyaloid haemorrhage, if dense (Fig. common in eyes with severe retinal ischaemia or per- 13.26B) and persistent should be considered for vitrec- sistent retinal detachment following unsuccessful pars tomy because, if untreated, the internal limiting mem- plana vitrectomy. brane or posterior hyaloid face may serve as a scaffold for subsequent fibrovascular proliferation and conse- quent tractional macular detachment or macular Indications for pars plana vitrectomy epiretinal membrane formation. Some cases of suc- 1. Severe persistent vitreous haemorrhage that pre- cessful dispersion with YAG lazer (hyaloidotomy) Q cludes adequate PRP is the most common indication. have been reported. Kanski_Chapter 13_main.indd 550 2/11/2011 10:44:48 AM
- 19. 13 CHAPTeR Retinal Vascular Disease 551 arteriole and its corresponding vein share a common adventitial sheath, thickening of the arteriole appears to compress the vein. This causes secondary changes, includ- ing venous endothelial cell loss, thrombus formation and potential occlusion. Similarly, the central retinal vein and artery share a common adventitial sheath at arteriovenous crossings posterior to the lamina cribrosa so that atherosclerotic changes of the artery may com- press the vein and precipitate central retinal vein occlu- sion (CRVO). It therefore appears that both arterial and venous disease contribute to retinal vein occlusion. Venous occlusion causes elevation of venous and capil- lary pressure with stagnation of blood flow. Stagnation results in hypoxia of the retina drained by the obstructed vein, which, in turn, results in damage to the capillary endothelial cells and extravasation of blood constituents. A The tissue pressure is increased, causing further stagna- tion of the circulation and hypoxia, so that a vicious cycle is established. Predisposing factors Common 1. Age is the most important factor; over 50% of cases occur in patients over the age of 65 years. 2. Hypertension is present in up to 73% of RVO patients over the age of 50 years and in 25% of younger patients. It is most prevalent in patients with BRVO, particularly when the site of obstruction is at an arte- riovenous crossing. Inadequate control of hyperten- sion may also predispose to recurrence of RVO in the same or fellow eye. 3. Hyperlipidaemia (total cholesterol >6.5 mmol/l) is B present in 35% of patients, irrespective of age. Fig. 13.26 Indications for pars plana vitrectomy. (A) Tractional 4. Diabetes mellitus is present in about 10% of cases detachment involving the macula; (B) large premacular over the age of 50 years but is uncommon in younger subhyaloid haemorrhage patients. This may be due to an associated higher prevalence of other cardiovascular risk factors such as hypertension which is present in 70% of type 2 Visual results of pars plana vitrectomy diabetics. Visual results depend on the specific indications for 5. Oral contraceptive pill. In younger females the contra- surgery and the complexity of pre-existing vitreoretinal ceptive pill is the most common underlying association, abnormalities. In general, about 70% of cases achieve and should not be taken following retinal vein occlu- visual improvement, about 10% are made worse and the sion. The risk may be exacerbated by thrombophilia. rest are unchanged. It appears that the first few postop- 6. Raised intraocular pressure increases the risk of erative months are vital. If an eye is doing well after 6 CRVO, particularly when the site of obstruction is at months, then the long-term outlook is good because the the edge of the optic cup. incidence of subsequent vision-threatening complications 7. Smoking. Current smoking may be associated with is low. Favourable prognostic factors include: an increased incidence of RVO, though studies have shown inconsistent results. • Good preoperative visual function. • Age 40 years or less. • Absence of preoperative rubeosis and glaucoma. Uncommon • Previous PRP to at least one-quarter of the fundus. Uncommon predispositions (listed below) may assume more importance in patients under the age of 50 years. RETINAL VENOUS OCCLUSIVE DISEASE 1. Myeloproliferative disorders • Polycythaemia. Pathogenesis • Abnormal plasma proteins (e.g. myeloma, Wal- denström macroglobulinaemia). Arteriolosclerosis is an important causative factor for 2. Acquired hypercoagulable states Q branch retinal vein occlusion (BRVO). Because a retinal • Hyperhomocysteinaemia. Kanski_Chapter 13_main.indd 551 2/11/2011 10:44:52 AM
- 20. Clinical Ophthalmology 552 A S y S T e m AT I C A P P RoAC H • Lupus anticoagulant and antiphospholipid 1. Chest X-ray. Sarcoidosis, tuberculosis, left ventricular antibodies. hypertrophy in hypertension. • Dysfibrinogenaemia. 2. C-reactive protein (CRP). Sensitive indicator of 3. Inherited hypercoagulable states inflammation. • Activated protein C resistance (factor V Leiden 3. ’Thrombophilia screen’. By convention refers to herit- mutation). able thrombophilias; might typically include thrombin • Protein C deficiency. time, prothrombin time and activated partial throm- • Protein S deficiency. boplastin time, antithrombin functional assay, protein • Antithrombin deficiency. C, protein S, activated protein C resistance, factor V • Prothrombin gene mutation. Leiden mutation, prothrombin G20210A mutation; • Factor Xll deficiency. anticardiolipin antibody (IgG and IgM), lupus 4. Inflammatory disease associated with occlusive anticoagulant. periphlebitis 4. Autoantibodies. Rheumatoid factor, anti-nuclear anti- • Behçet syndrome. body, anti-DNA antibody. • Sarcoidosis. 5. Serum angiotensin-converting enzyme (ACE). • Wegener granulomatosis. Sarcoidosis. • Goodpasture syndrome. 6. Fasting plasma homocysteine level. To exclude 5. Miscellaneous hyperhomocysteinaemia. • Chronic renal failure. 7. Treponemal serology. Local testing preference should • Causes of secondary hypertension (e.g. Cushing be discussed with the microbiology team. syndrome) or hyperlipidaemia (e.g. hypothy- 8. Carotid duplex imaging to exclude ocular ischaemic roidism). syndrome. • Orbital disease. • Dehydration may be significant, particularly in Branch retinal vein occlusion younger patients and in hot countries Factors that appear to decrease the risk of venous occlu- Classification sion include increased physical activity and moderate alcohol consumption. 1. Major branch retinal vein occlusion (BRVO) at the disc (Fig. 13.27A) and away from the disc (Fig. 13.27B). 2. Macular BRVO involving only a macular branch (Fig. Systemic assessment 13.27C). All patients 1. Blood pressure. 2. Erythrocyte sedimentation rate (ESR) or plasma vis- cosity (PV). B 3. Full blood count (FBC). 4. Random blood glucose. Further assessment for diabe- tes if indicated. 5. Random total and HDL cholesterol. Additional lipid C testing may be considered. 6. Plasma protein electrophoresis. To detect dysprotei- naemias such as multiple myeloma. 7. Urea, electrolytes and creatinine. Chronic renal F failure is a rare cause of RVO, but renal disease may occur in association with hypertension. 8. Thyroid function tests. Patients with RVO have a higher prevalence of thyroid disease than the general population. Thyroid dysfunction is also associated A with dyslipidaemia. 9. ECG. To detect left ventricular hypertrophy second- ary to hypertension; required for the Framingham D equation used in the calculation of cardiovascular risk. Selected patients according to clinical indication E Patients in whom these might be considered are those under the age of 50, those with bilateral RVO, a history Fig. 13.27 Classification of retinal branch vein occlusion of previous thromboses or a family history of thrombosis, according to site of blockage. (A) Major at the disc; (B) and possibly in other patients in whom investigation for major away from the disc; (C) minor macular; (D–F) Q the common associations is negative. peripheral not involving the macula Kanski_Chapter 13_main.indd 552 2/11/2011 10:44:54 AM
