Multiple sclerosis
- 2. LECTURE №8 THEME : Demyelination diseases of nervous system
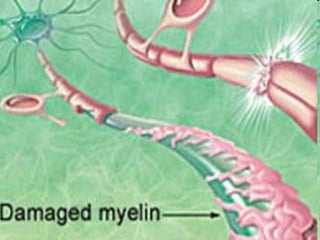
- 3. Myelinated axons Most axons are surrounded by a myelin sheath . The myelin sheaths of the central nervous system are composed of the cell membrane of oligodendroglia , which is wrapped around the axon to form a multilaminar structure.
- 4. The myelin sheath enables the axon to conduct impulses more rapidly; thus, loss of myelin lowers conduction velocity, producing clinical manifestations of neuronal dysfunction. Each layer of a myelin sheath is 7.5 microns thick and is composed of two lipoid and two proteinaceous monomolecular layers . The common feature of all diseases affecting myelin is a pathological abnormality or total destruction of myelin sheaths , primarily in the central nervous system. In the genetic myelinopathies , the primary development of myelin is deficient .
- 5. B ut, in many cases , myelin is lost later in life, in the metabolic and autoimmune demyelinating diseases . They call this group of demyelinating diseases myelinoclasthies . Myelinopathies : adrenoleikodystrophies, phenylke-tonuria, mitochondrial leukoencephalopathies, leukodys - trophies Krabbe and disease of Kanavan, disease of Alexander. The most common myelinoclasthies are multiple sclerosis, acute disseminated encephalomyelitis concentric sclerosis (Balo sclerosis), Neuromyelitis optica (Devic disease) diffuse encephalitis of Schilder and subacute leukoencephalitis of Van Bogart .
- 6. Multiple sclerosis (MS) is a chronic disease of the CNS that begins most commonly in young adults and is characterized pathologically by multiple areas of CNS white matter inflammation, demyelination, and glial scarring (sclerosis) . It usually presents with episodic neurological deficits , which, later on in the course of the disease, tend not to reverse fully, leaving increasingly severe residual deficits whose summation causes progressively severe disability . The clinical manifestations are very diverse because widely separated areas of the CNS are affected and the temporal course of the disease is variable . “Disseminated encephalomyelitis” is a synonym for multiple sclerosis.
- 7. An important characteristic of MS is that the number of lesions, or plaques, that are discovered scattered throughout the white matte (with occasional extension into gray matter) at autopsy is invariably larger than the number of lesions detected clinically or by means of laboratory tests. These silent lesions may be responsible for aspects of the disease that are poorly understood, especially mental and cognitive disturbances.
- 8. Epidemiology. MS is particularly common in northern Europe , the northern U.S.A., southern Canada, New Zealand, and southwest Australia. Although environmental factors may be important in etiology, the observation of increased risk of MS in families of an MS patient cannot be lightly dismissed; both environmental and genetic factors are probably important. There are the main of peculiriaties: 1. MS affects women more than men in a ratio of about 1.5 to 1. 2. There are also some clinical differences in different localities. 3. MS is predominantly a disease of young adults.
- 9. Pathological anatomy. There are disseminated foci of demyelination in the CNS (brain and spinal cord), sometimes with destruction of axons as well. Local, reactive gliosis is found at the sites of older foci. Thus, “sclerosis” develops at “multiple” locations, giving the disease its English name.
- 10. MRI of the brain and spinal cord in patient with MS
- 11. MRI of the brain in multiple sclerosis. a Asymmetrically scattered foci of abnormal signal, affecting only the white matter, are seen in the periventricular regions and at the anterior and posterior ends of the lateral ventricles. There is mild internal hydrocephalus. b There are typical signal abnormalities in the corpus callosum, extending into the white matter of the hemispheres.
- 13. Pathogenesis. Two major theories about the pathogenesis of MS are being pursued. The first rests on the concept of an infection (presumably by a viral agent) with a long incubation period. The other theory postulates altered immune regulation. The major histocompatibility complex (MHC) on chromosome 6 has been identified as one genetic determinant for MS. The MHS encodes the genes for the histocompatibility antigens (the human leucocyte antigen [HLA] system) involved in antigen presentation to T-cell. The class II haplotype DR15, DQ6, Dw2 is associated with increased risk of MS.
- 14. Therefore, different infectious agents or other environmental factors may cause or predispose to autoimmune attack upon central myelin. The result of this process is myelin destruction. At the beginning of the process auto-allergic processes prevail over the other ones. Then immunodeficiency is developed. Restoration of a balance between immunosuppressor and cytotoxic cells might induce clinical remission.
- 16. New data on the ontogeny of human immunity indicate that adult levels of humoral and cellular immunity develop gradually during childhood and may not be mature until the second half of the first decade. In childhood, when there is a natural imbalance of immune components, individuals may be particularly susceptible to a demyelinating type of host response.
- 18. Clinical forms I. Cerebral forms: - cortical (epileptic attacks, psychiatric disorders) - visual - brain stem - cerebellar II. Spinal forms: - cervical - thoracic - lumbar-sacral - pseudotabes III. Cerebrospinal
- 19. The course of the disease: - remittent (exacerbation and remission without progression) - remitting-progressive - secondary progressive (by episodic worsening at first with 2-3 remission, followed by steady progression) - primary progressive ( by steady progression from the beginning ). The periods of the disease: - exacerbation - remission (complete, incomplete) - stable periods
- 20. Clinical manifestations and neurological findings. The neurological deficits present in each individual patient depend on the number and location of the demyelinating foci. Exacerbations and remissions occur frequently. The main characteristics of the symptoms of MS are : - multiplicity - the tendency to vary in nature - severity with the passage of time - complete remission of the first symptoms occurs frequently but, with subsequent attacks, remissions do not occur or are incomplete. - the clinical course extends for one or many decades in most cases, but a few may terminate in death within a few months of onset.
- 21. The following are among the more characteristic disease manifestations and physical findings: - retrobulbar neuritis - disturbances of ocular motility - Lhermitte sign - p yramidal tract signs - cerebellar signs - gait impairement - sensory deficits - bladder dysfunction - ictal phenomena - mental disturbances
- 22. Retrobulbar neuritis is usually unilateral. Over the course of a few days, the patient develops an impairment of color vision , followed by a marked impairment of visual acuity (finger counting is barely possible). Orbital pain is often present and the patient may see flashes of light on movement of the globe . These problems begin to improve in one or two weeks and usually resolve completely. The temporal side of the optic disc becomes pale three or four weeks after the onset of symptoms. Retrobulbar neuritis rarely affects both eyes, either at the same time or in rapid succession. Recurrences are rare.
- 23. If retrobulbar neuritis is an isolated event in a patient otherwise free of neurological disease, the probability that other clinical signs of multiple sclerosis will appear in the future is roughly 50%. This probability is greater if pathological changes are seen in the CSF or on an MRI scan. Temporal papillary atrophy (after optic neuritis)
- 24. Disturbances of ocular motility. Diplopia , particularly due to abducens palsy , is a common early symptom but nearly always resolves spontaneously. Later, typical findings are nystagmus (often dissociated) and internuclear ophthalmoplegia , often without any subjective correlate. Internuclear ophthalmoplegia in a young patient is relatively specific for multiple sclerosis. This condition is caused by a lesion of the medial longitudinal fasciculus (MLF). When the patient attempts to look away from the side of the lesion, the ipsilateral (adducting) eye cannot fully adduct, and the contralateral (abducting) eye exhibits end-gaze nystagmus.
- 25. The inability of the ipsilateral eye to adduct is not due to a lesion of the oculomotor n. nucleus, as is demonstrated by a preserved ability to adduct (converge) in the near reflex. Internuclear ophthalmoplegia (INO) can also be bilateral if the MLF is damaged on both sides. Right internuclear ophthalmoplegia in a patient with multiple sclerosis. In the initial phase of leftward gaze (upper photograph), only the left eye is abducted. The right eye follows, after a delay (lower photograph).
- 26. Test for visual field defects (confrontation test) Central scotoma
- 27. Lhermitte sign (positive neck-flexion sign). Active or passive forward flexion of the neck induces an “electric” paresthesia running down the spine and/or into the limbs. Retrobulbar neuritis, disturbances of ocular motility, sensory deficits, and Lhermitte sign are common early findings in multiple sclerosis. Pyramidal tract signs and exaggerated intrinsic muscle reflexes may be present early in the course of the disease. The abdominal cutaneous reflexes are absent . Later on, in almost all patients, spastic paraparesis or quadriparesis develops.
- 28. Motor disturbances (central paresis, spasticity, abnormal fatigability)
- 29. Cerebellar signs are practically always present in advanced MS, incl u ding impaired coordination , ataxia , and, frequently, a very characteristic intention tremor Gait impairment often becomes severe early in the course of the disease. Typically, the combination of spastic paraparesis and ataxia results in a spastic−ataxic, uneven, uncoordinated, and stiff gait .
- 30. Sensory deficits are found early in the course of the disease in about half of all patients. Vibration sense in the lower limbs is nearly always impaired. Pain is not uncommon; sometimes there is even a dissociated sensory deficit. Bladder dysfunction is present in about three-quarters of all patients (generally in association with spasticity); disturbances of defecation are much rarer. Bladder dysfunction is sometimes an early manifestation of the disease.
- 31. Urge incontinence is highly characteristic, i. e., a sudden, almost uncontrollable need to urinate, perhaps leading to “accidents” and bedwetting. Patients often do not mention bladder dysfunction until they are directly asked about it.
- 32. Ictal phenomena of various types are not uncommon. About 1.5% of persons with MS suffer from trigeminal neuralgia , which may alternate from one side to the other. Acute dizzy spells can occur, as can paroxysmal dystonia , dysarthria , or ataxia. The characteristic so - called tonic brainstem seizures consist of paroxysmal, often painful, tonic stiffness of the muscles on one side of the body. The lower limb is hyperextended, the upper limb flexed (Wernicke−Mann posture).
- 33. Mental disturbances are not severe early in the course of the disease. Later on, however, ma - ny patients develop psychoor - ganic changes and psycho - re - active and depressive distur - bances. Psychosis is very rare.
- 35. Intention tremor (fingeer-nose test and heel-to-knee test)
- 36. Nystagmus Internuclear ophthalmoplegia
- 39. MS degree: I – patient has difficulty to walk only after physical training II – patient has difficulty to walk and weakness on 2-3 km III – patient has spastic-paretic gait, difficulty to walk and weakness on 200-300m IV – patient can not to walk without help V – patient can not to walk or has blindness
- 41. MRI in patient with MS
- 42. Evoked potentials. Visual evoked potential (VEP) studies reliably detect optic nerve lesions, VEP reveals prolongation of the P100 latency in one eye and/or an abnormally large discrepancy between the latencies in the two eyes in roughly 40% of MS patients without known optic neuritis, and in almost half of those with early optic neuritis. Somatosensory evoked potential (SEP) studies of the median or tibial nerve typically reveal prolonged latencies in MS. Low amplitude of evoked potentials, on the other hand, often indicates a pathological process of another type, e. g. tumor. SEP abnormalities are found in up to 60% of MS patients with predominantly sensory manifestations.
- 43. Auditory evoked potential (AEP) studies are less sensitive in MS than VEP or SEP. The most common AEP change is prolongation of latency. AEP studies are helpful for the further classification of vertigo, tinnitus, and hearing loss. Motor evoked potential (MEP) studies reveal prolonged central conduction times when CNS lesions involve the pyramidal pathway. The sensitivity of MEP in MS is approximately the same as that of SEP. MEP studies can provide supporting evidence for MS in patients with latent paresis, gait disturbances, abnormal reflexes, or movement disorders that are difficult to classify.
- 44. Tests of bladder function. The residual urine volume can be measured by ultrasound. It should not exceed 100 ml in patients with a normal bladder capacity of 400–450 ml; in general, it should normally be 15–20% of the cystomanometrically determined bladder volume. Urodynamic electromyography (EMG) provides more specific data concerning bladder dysfunction.
- 45. CSF examination. CSF abnormalities are found in more than 95% of MS patients. The cell count rarely exceeds 20 cells/mm3. The total protein concentration is elevated in ca. 40% of patients, and intrathecal IgG synthesis (IgG index) in ca. 90%. Oligoclonal IgG is found in 95% of MS pati - ents, and antibodies to mumps, measles and herpes zoster in 80%. Oligoclonal bands in the serum (a) and CSF (b) of a patient with multiple sclerosis ; compare with the serum ( c ) and CSF ( d ) of a normal control subject.
- 46. Differential Diagnosis There is no single clinical test, imaging study, or laboratory finding that alone establishes the diagnosis of MS. A meticulous differential diagnostic evaluation is needed in every case. (Cerebral) Vasculitis. Systemic lupus erythematosus, Sjögren syndrome, Behçet syndrome, granulomatous angiitis, polyarteritis nodosa, antiphospholipid syndrome, chronic inflammatory demyelinating polyradiculoneuro - pathy.
- 47. Inflammatory diseases. Neurosarcoidosis, neuroborreliosis, neurosyphilis, Whipple disease, postinfectious acute disseminated encephalomyelitis (ADEM), progressive multifocal leukoencephalopathy (PML), subacute sclerosing panencephalitis (SSPE), HIV infection, HTLV-1 infection. Neurovascular disorders. Arteriovenous fistula of spinal dura mater, cavernoma. Hereditary/metabolic disorders. Adrenoleukodystro - phy, endocrine diseases, mitochondrial encephalo - myelopathy, vitamin B12 deficiency (funicular myelosis).
- 48. Tumors of the brain or spinal cord ( lymphoma, glioma,meningioma). Skull base anomalies . Arnold–Chiari malformation, platybasia. Myelopathy . Cervical myelopathy (spinal stenosis). Somatoform disturbances in the context of mental illness. Prognosis Favorable prognostic indicators in MS include onset b e- fore age 40, monosymptomatic onset, absence of cere - bellar involvement at onset, rapid resolution of the initial symptom(s), a relapsing-remitting course, short duration of relapses, and long-term preservation of the ability to walk.
- 49. A relatively favorable course is also predicted if, after the first 5 years of illness, the MRI reveals no more than a few, small lesions without rapid radiological progression and the clinical manifestations of cerebellar disease and central paresis are no more than mild. A benign course , defined as a low frequency of recurrences and only mild disability in the first 15 years of illness, is seen in 20–30% of patients. The disease takes a malignant course , with major disability within 5 years, in fewer than 5% of patients. Half of all MS patients have a second relapse within 2 years of disease onset.
- 53. Symptomatic therapy/rehabilitation. Medications, physical, occupational, and speech therapy, social, psychological, and dietary counseling, and mechanical aids (e. g., walking aids, wheelchair) are provided as needed. The possible benefits of oligodendrocyte precursor cell transplantation for remyelination, and of growth factors and immunoglobulins for the promotion of endogenous remyelination, are currently under investigation in both experimental and clinical studies.
- 54. Gait problems are the most common disability of MS; the problems respond to treatment if spasticity is the major cause. In these cases, careful use of baclofen is helpful, but if too much is administered, spasticity gives way to excessive flaccidity and makes the gait disorder worse. Intention tremor occasionally responds to propranolol 320 mg per day in divided dosage. Cryothalamotomy has been used, but the complication of pseudobulbar palsy makes this too hazardous.
- 55. Diffuse encephalitis of Schilder. The diagnostic criteria established by Poser in 1985 require 6 elements: 1. One or 2 roughly symmetrical large plaques are manifest, and if more than 1 is present, 1 should be in each brain hemisphere, chiefly in the centrum semiovale. 2. No other lesions are demonstrable by clinical, paraclinical, or imaging data. 3. No abnormalities of the peripheral nervous system are demonstrable. 4. Results of adrenal function studies are normal. 5. Serum very long chain fatty acids are normal. 6. Pathological analysis by autopsy or biopsy demonstrates histologic changes consistent with subacute or chronic myelinoclastic diffuse sclerosis, changes which in essence cannot be distinguished from those of multiple sclerosis.
- 56. No features of the general examination are characteristic features of the presentation of Schilder disease. Aphasia , memory disturbances , mental dullness , irritability , changes in personality , confusion, disorientation , and behavioral disturbances are not infrequently encountered. Patients may appear to be psychotic . Deafness is common. Other brainstem or cerebellar deficits that are encountered include vertigo ; paresis of eye movements , including internuclear ophthalmoplegia and nystagmus ; facial palsy ; dysarthria ; or dysphagia .
- 57. Peripheral cranial nerve abnormalities that are sometimes encountered include optic neuritis and optic atrophy. Cortical blindness is common, and various field cuts may be found, particularly hemianopsia. Hemiparesis or cortical sensory deficits may be found. Seizures may occur but are not common. Some patients manifest psychosis. Extrapyramidal manifestations are rare but have been described. Findings of variable or uncertain localization include generalized spasticity and incontinence of bowel and bladder function. Malnutrition and cachexia are commonly reported in the middle or late chronic stages of illness, especially in instances where patients fall to a low level of neurologic function such as a chronic vegetative state.
- 58. Thank you for your attention !
