Toxicol Sci -2016-Korte CNS admin
- 1. CONTEMPORARY REVIEW Safety Evaluation of CNS Administered Biologics— Study Design, Data Interpretation, and Translation to the Clinic Brian R. Vuillemenot,*,1 Sven Korte,† Teresa L. Wright,‡ Eric L. Adams,§ Robert B. Boyd,§ and Mark T. Butt¶ *Genentech, Inc, South San Francisco, California; † Covance Laboratories GmbH, Mu¨ nster, Germany; ‡ Dimension Therapeutics, Cambridge, Massachusetts; § Northern Biomedical Research, Muskegon, Michigan; and ¶ Tox Path Specialists, Frederick, Maryland 1 To whom correspondence should be addressed at Genentech, Inc., 1 DNA Way, South San Francisco, California 94080. Fax: 650-866-2621. E-mail: vuillemb@gene.com. ABSTRACT Many central nervous system (CNS) diseases are inadequately treated by systemically administered therapies due to the blood brain barrier (BBB), which prevents achieving adequate drug concentrations at sites of action. Due to the increasing prevalence of neurodegenerative diseases and the inability of most systemically administered therapies to cross the BBB, direct CNS delivery will likely play an increasing role in treatment. Administration of large molecules, cells, viral vectors, oligonucleotides, and other novel therapies directly to the CNS via the subarachnoid space, ventricular system, or parenchyma overcomes this obstacle. Clinical experience with direct CNS administration of small molecule therapies suggests that this approach may be efficacious for the treatment of neurodegenerative disorders using biological therapies. Risks of administration into the brain tissue or cerebrospinal fluid include local damage from implantation of the delivery system and/or administration of the therapeutic and reactions affecting the CNS. Preclinical safety studies on CNS administered compounds must differentiate between the effects of the test article, the delivery device, and/or the vehicle, and assess exacerbations of reactions due to combinations of effects. Animal models characterized for safety assessment of CNS administered therapeutics have enabled human trials, but interpretation can be challenging. This manuscript outlines the challenges of preclinical intrathecal/intracerebroventricular/intraparenchymal studies, evaluation of results, considerations for special endpoints, and translation of preclinical findings to enable first-in-human trials. Recommendations will be made based on the authors’ collective experience with conducting these studies to enable clinical development of CNS-administered biologics. Key words: CNS administration; intrathecal; intracerebroventricular; neurodegeneration; enzyme replacement therapy. Neurodegenerative diseases represent a major health burden and inadequately met medical need. This burden includes Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis, Huntingdon’s disease, lysosomal storage diseases (LSDs), and other diseases. Systemically administered biologics have not yet been effective in treating these diseases, largely due to the challenges in achieving adequate concentrations at key sites of action in the central nervous system (CNS). Direct CNS administration circumvents the barriers that keep large molecules out of the CNS and introduces potential therapies VC The Author 2016. Published by Oxford University Press on behalf of the Society of Toxicology. All rights reserved. For Permissions, please e-mail: journals.permissions@oup.com 3 TOXICOLOGICAL SCIENCES, 152(1), 2016, 3–9 doi: 10.1093/toxsci/kfw072 Contemporary Review atLibraryonJune27,2016http://toxsci.oxfordjournals.org/Downloadedfrom
- 2. close to sites of action, and is likely to play an increasingly large role in addressing these unmet medical needs. Preclinical devel- opment of CNS-administered therapeutics faces a number of challenges not typically encountered with systemically admin- istered therapeutics. The objective of this article is to review the main challenges of preclinical safety assessment of CNS admin- istered molecules. Recommendations for the translation of these studies to enable first-in-human trials will also be made. Current experience with protein-based therapeutics ad- ministered directly to the CNS is limited. CNS-administered biologics have been evaluated preclinically and/or clinically to treat pain, cancer, neurodegenerative diseases, and lyso- somal storage diseases (LSDs)]. A summary is presented in Table 1. The only currently marketed biologic developed specifically for direct CNS administration is Ziconitide, a cone snail derived peptide to treat pain (Williams et al., 2008). Baclofen, a marketed small molecule therapy approved for treatment of muscle spasms, was also developed for intrathecal (IT) administration (Richard and Menei, 2007). Several monoclonal antibodies have been administered to the cerebrospinal fluid (CSF) off label with evidence of efficacy in different cancers. In contrast, attempts to develop therapies for neurodegenerative diseases using CNS administration of growth and neurotrophic factors have so far been unsuccessful. LSDs may be caused by genetic deficiency of lysosomal enzymes, with over two-thirds involving CNS disease (Schultz et al., 2011). Systemically administered enzyme replace- ment therapies (ERTs) have been successful in treating nonCNS symptoms of these diseases, but not the neurological compo- nents (Hollak and Wijburg, 2014). Several of the approved ERTs have been used off label for direct CNS administration (Mu~noz- Rojas et al., 2008, 2010). Several clinical trials are in progress for CNS-administered ERTs to treat neurodegenerative LSDs (Katz et al., 2014; Muenzer et al., 2016). Gene therapy strategies using IT administration have been described in Beutler et al. (2005) and Hirai et al. (2014). Direct CNS delivery of antisense oligonu- cleotides (ASOs), used to regulate target mRNA, is also in devel- opment (Miller et al., 2013). Intracerebroventricular (ICV) and IT administration of ASOs has resulted in neuronal uptake in mon- eys and dogs. BREACHING THE BLOOD BRAIN BARRIER The blood brain barrier (BBB) represents the primary obstacle to achieving CNS distribution of large molecule therapeutics ad- ministered systemically. The BBB consists of tight junctions be- tween capillary endothelial cells that provide a physical barrier to the entry of large molecules (Bauer et al., 2014; Tajes et al., 2014). Numerous transporters in the BBB tightly regulate move- ment of molecules from the bloodstream to the CNS (Fricker and Miller, 2004). Through the physical barrier provided by the tight junctions and the transport barrier, virtually all large mol- ecules are excluded from the CNS when administered into the systemic circulation. Physically breaching the BBB by administering a therapy into the CSF is one means of achieving CNS distribution. CSF plays multiple roles including providing brain buoyancy, protecting the brain from sudden impacts, regulation of solute concentra- tions and pressure, and elimination of wastes (Sakka et al., 2011). CSF is secreted continuously at a rate of approximately 0.3 ml/min in adults primarily by choroid plexus ependymal cells in the ventricles (Oreskovic and Klarica, 2010). It flows out through the ventricular system into the subarachnoid space, and around the external surfaces of the brain and spinal cord (Greitz, 1993). CSF circulates through the brain parenchyma along perivascular spaces surrounding arteries via the glym- phatic pathway; this brain-wide perivascular network facilitates solute exchange between the CSF and interstitial fluid (Iliff et al., 2012; Yang et al., 2013). The continuous movement of CSF can distribute therapeutics in the CNS after IT or ICV administra- tion. The total CSF volume in an adult human is approximately 150 ml, with a total of approximately 500 ml of CSF secreted per day. Drainage into the systemic circulation via the arachnoid granulations and lymphatics (Bulat and Klarica, 2011) allows for maintenance of a stable volume. TABLE 1. Representative Biological Therapies that Have Been Used for Direct CNS Administration Indication Molecule Route Development Phase/Results References Pain Ziconitide (Prialt) IT-L Approved Williams et al. (2008) Breast cancer brain metastasis Trastuzumab (Herceptin) IT-L Off label/P1/2 Oliveira et al. (2011) Leukemia Rituximab (Rituxan) IT-L P1/2 Jaime-Perez et al. (2009) Non-Hodgkins lymphoma ICV Off label/P1/2 Rubenstein et al. (2007) Multiple sclerosis IT-L P2 Bonnan et al. (2014) Alzheimer’s disease Nerve growth factor (NGF) ICV Off label Eriksdotter Jonhagen et al. (1998) Parkinson’s disease Glial derived neurotrophic factor (GDNF) ICV, IP Clinical trials stopped after P2 Nutt et al. (2003), Patel et al. (2005) Amyotrophic lateral sclerosis Brain derived neurotrophic factor (BDNF) IT-L No efficacy in P3 Beck et al. (2005) Vascular endothelial growth factor (VEGF) ICV P1/2 Storkebaum et al. (2005) Mucopolysaccharidosis I Laronidase (Aldurazyme) IT-L Off label Munoz-Rojas et al. (2008) Mucopolysaccharidosis II Idursulfase-IT IT-L P2/3 Felice et al. (2011), Muenzer et al. (2016) Mucopolysaccharidosis IIIA Heparan-N-sulfatase IT-L P1/2 Pfeifer et al. (2012) Mucopolysaccharidosis IIIB Alpha-N-acetylglucosaminidase ICV Preclinical Kan et al. (2014) Mucopolysaccharidosis VI Galsulfase (Naglazyme) IT-L Off label Mu~noz-Rojas et al. (2010) Metachromatic leukodystrophy Arylsulfatase A IT-L P1/2 Patil and Maegawa (2013) CLN2 disease (a form of Batten Disease) Tripeptidyl peptidase I ICV P1/2 Katz et al. (2014), Vuillemenot et al. (2015) ICV, intracerebroventricular; IP, intrapanenchymal; IT-L, intrathecal lumbar. 4 | TOXICOLOGICAL SCIENCES, 2016, Vol. 152, No. 1 atLibraryonJune27,2016http://toxsci.oxfordjournals.org/Downloadedfrom
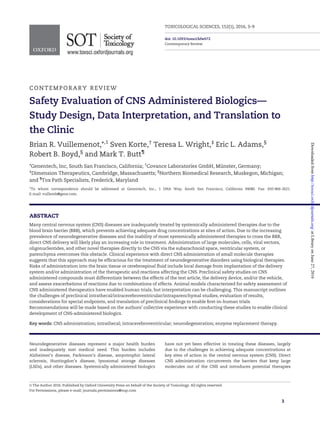
- 3. ROUTES OF DIRECT ADMINISTRATION TO THE CNS There are several routes of direct CNS administration, either via the CSF or directly to tissue. IT administration introduces the therapeutic into the CSF in the subarachnoid space, between the arachnoid and pia mater. This is most frequently accom- plished via the implantation of a catheter into the IT lumbar (IT-L) space. IT-L administration has a potential disadvantage that the administered biologic needs to travel a longer distance to reach the brain than via other direct routes to the CNS. However, IT-L administration studies in multiple nonclinical species have demonstrated adequate brain distribution to achieve pharmacological activity of the therapeutic when ad- ministered in a large dose volume or with a subsequent catheter flush with buffer (Dickson et al., 2007; Felice et al., 2011; Xu et al., 2011). With test articles more dense than CSF, body posture dur- ing IT-L dose administration (supine vs upright) may lead to dif- ferences in brain distribution, particularly in semi-bipedal species, such as monkeys. Delivering test articles to the CSF in closer proximity to the brain can also be achieved by adminis- tering into the cisterna magna within the cerebromedullary cis- tern (IT-cisternal, IT-C). IT-C administration is not often used clinically because of safety risks but is sometimes used in pre- clinical studies. Catheters and dosing ports have been im- planted to the lumbar spine to enable repeat IT-L infusion administration in multiple animal models. IT-C administration is typically conducted as a bolus injection. In rodents, IT cathe- ters terminating in the lumbar space may be introduced through the cerebromedullary cistern. ICV administration introduces the therapeutic into the lat- eral ventricle, in close proximity to the primary CSF production. The outward flow of CSF from the ventricles may result in wider CNS distribution than that achieved by IT-L administration (Vuillemenot et al., 2014). ICV administration is usually accom- plished by infusion via an implanted catheter and dosing port. Intraparenchymal (IP) administration introduces the therapy di- rectly to the brain tissues. Convection enhanced delivery can be used to increase the distribution achieved with IP administra- tion through increased pressures (Barua et al., 2014). As com- pared with IP administration, introducing the therapeutic to the CSF by IT or ICV administration may produce a broader distribu- tion pattern. Both bolus and continuous administration may be utilized with these different routes. Infusions lasting from several hours to continuous may be preferable to bolus injection to achieve the required concentration of therapeutic in the brain safely. If the rate of infusion is less than the normal turnover of CSF, then no appreciable changes in CSF volume will result, and safety concerns due to excessive intracranial pressure can be minimized. When selecting an appropriate clinical route, it is important to consider the optimal CNS distribution in the in- tended patient population. Whenever possible, the intended clinical route of administration should be used for any pivotal preclinical safety studies, although alternate routes are often employed for preliminary studies, and occasionally for pivotal toxicology studies. CONSIDERATIONS FOR DESIGN OF NONCLINICAL CNS ADMINISTRATION STUDIES Nonclinical studies involving direct CNS administration are fun- damentally different than studies with more conventional routes and several important points should be considered. Adverse ef- fects in CNS delivery studies are generally not due to the biologic per se, but changes due to the delivery device alone or with an ad- ditive effect related to the therapeutic may occur. Inclusion of ve- hicle and/or device-only control groups is critical to sort out the causes of any findings. Due to the often limited group size of these studies, a thorough review of historical control data may be the only accurate means of assessing study findings. Recently, the Society of Toxicologic Pathologists published updated recommendations for sampling the CNS for general toxicity studies (Bolon et al., 2012). Although possibly sufficient for general toxicity studies where there is no reason to suspect an effect on the nervous system, these schemes are not ade- quate for a study involving direct CNS delivery. The trimming/ embedding/staining scheme for a direct CNS delivery study should be customized to allow for a thorough assessment of the local effects on the various structures/cell types of the brain and spinal cord that may be due to the placement/presence of the drug and/or the delivery device, as well as more distant effects that may be due to the device, or distribution of the drug. Assessment of pharmacokinetics (PK), exposure, and immu- nogenicity are important for evaluating the dose response of any pharmacology or toxicity of a CNS administered biologic. A significant fraction of the test article that is not distributed into the CNS will enter the systemic circulation within a few hours via the arachnoid granulations and/or lymphatics. This occurs through natural CSF turnover and via outflow caused by increased pressure (Bulat and Klarica, 2011). CSF also drains to cervical lymph nodes via the glymphatic system, a dural lym- phatic network (Aspelund et al., 2015). Systemic exposure to CNS-administered biologics can lead to an immune response. Anti-drug antibody (ADA) formation may occur when adminis- tering a human protein to animals. This response may result in decreased exposure and/or activity or hypersensitivity reactions. Administering a biologic to the CNS via slow infusion may reduce the maximal systemic concentrations and reduce the likelihood of immunogenicity. In addition, pretreatment with antihistamines has been efficacious in reducing the incidence of hypersensitivity (Kim et al., 2008; Vuillemenot et al., 2011). Sufficient sampling of both plasma and CSF should be in- cluded to characterize standard PK parameters, while ADAs may be monitored in serum and/or CSF. To enable collection of serial samples, a dual catheter/access port setup may be useful, with one catheter used for dose administration and the other catheter for CSF collection (Figure 1). CSF samples collected from the ventricles versus the lumbar region have been shown to differ in composition and cellularity (Provencio et al, 2005; Rubalcava and Sotelo, 1995; Torres-Corzo et al., 2009), which should be considered when interpreting CSF data and compar- ing between studies. As a backup to lumbar sampling, direct cis- terna magna sampling may be used to obtain CSF for analysis, although this is a technically challenging procedure in nonclini- cal species due to the small volume of this space and close prox- imity to the spinal cord. The CNS distribution should be also evaluated to guide the clinical dose regimen. This can be accomplished through dedi- cated biodistribution studies or by sampling CNS tissues in pharmacology and/or toxicology studies to analyze for drug concentrations. Understanding the relationship between CSF/ systemic PK and CNS exposure is important when designing the clinical dosing regimen. This is best assessed in animal models, as serial CSF sampling is generally not possible in clinical studies. VUILLEMENOT ET AL. | 5 atLibraryonJune27,2016http://toxsci.oxfordjournals.org/Downloadedfrom
- 4. A very important final consideration is the selection of ap- propriate in vivo models to assess the safety, PK, and pharmaco- logical activity. The species selected should express a similar target as that in human patients. When administering a human protein to animals, the molecule should display activity against the homologous target in the animals. Differences in the activ- ity or receptor density in the species tested should be consid- ered when interpreting the results. When developing therapies for neurodegenerative diseases where the CNS is undergoing changes that may affect the safety, distribution, and/or activity of the molecule, it may be informative to conduct safety assess- ments in an animal disease model undergoing similar changes. Non-affected controls of the same species can be assessed alongside to get an idea of the toxicity on a non-diseased CNS background. NONCLINICAL SPECIES SELECTION/ INTERPRETATION When interpreting in vivo data, the relevance of the CNS in the nonclinical species to the human should be carefully consid- ered. Biologics have been administered directly to the CNS in all of the common lab animal species, including mice, rats, dogs, monkeys, sheep, and pigs. CNS differences between these spe- cies and human must be considered when designing and inter- preting direct CNS administration studies. A summary of different parameters affecting the pharmacology and safety of CNS-administered molecules is presented in Table 2. Differences in brain mass are an important limitation of ani- mal models. The nonclinical species have a significantly smaller brain than humans. Smaller brains have a higher sur- face area to volume ratio, potentially increasing relative uptake from CSF. In addition, the smaller the brain, the less distance a therapeutic is required to travel to reach all sites of activity within the CNS. Smaller brains may also display a more severe reaction to CNS delivery devices, and there is less area in which to implant these devices. Achieving precise targets within the smaller brains of animals is more challenging because of the smaller relative size of these targets. For example, the lateral ventricle has a mean volume of approximately 25 ml in hu- mans, but only 0.25 ml in monkeys (Akdogan et al., 2010). Total CSF volume is also less in the nonclinical species than human. However, the rate of CSF turnover is similar between dog, mon- key, and human, but several-fold higher in rodents. Differences in CSF volume and turnover must be taken into account when interpreting PK data and scaling to human patients. MORPHOLOGIC ASSESSMENT OF CNS TISSUES Morphologic assessment of the nervous system in a study uti- lizing a direct delivery device requires particular scrutiny in the areas traversed by the device and the site of deposition of the therapeutic. Synergy may be observed between the test article and the delivery system. Complications of surgery or the device are common, and even in vehicle/device only control animals there may be numerous microscopic changes (Butt, 2011a). These changes must be differentiated from what is caused by the test article. When evaluating nervous system tissues from a direct CNS deliver study, the timing of the necropsy, tissue processing, and staining must be carefully considered. Timing of tissue collec- tion must capture the full spectrum of potential changes occur- ring. It is important to assess effects acutely, as early toxicities may be completely resolved at later times (Switzer, 2011). Single-dose pilot studies should include multiple tissue collec- tion times. Morphological assessment is complicated because there must be sufficient time between device implantation and dosing to allow for the changes from surgery to resolve. It is common to observe neuronal necrosis at the site of catheter in- sertion into the brain, but this should not be confused with an effect of the tested therapeutic. Design of the CNS morphological evaluation should be based on the study objectives, delivery methods, and any knowledge of the effects of the test article. In addition to brain and spinal cord, nerves and ganglia may warrant evaluation. Changes to one part of the nervous system may manifest as changes in other parts, and all may need to be examined. The brain and spinal cord should be sectioned to allow for an evaluation that provides sufficient confidence that any effects on the CNS have FIG. 1. Dual port catheter system in the cynomolgus monkey. In this setup, the animal was surgically implanted with access ports and catheters terminating in the lumbar spine and the cisterna magna. The lumbar catheter/access port, which has a dosing needle inserted in this picture, was used for dose adminis- tration, while the cisternal device enabled repeat CSF sampling for toxicokinetic and other analyses. TABLE 2. CNS Parameters of Nonclinical Species Compared with Human Species Mouse Rat Dog Monkey Human Brain mass (fold human) 0.4 g (0.0004) 2 g (0.002) 72 g (0.072) 100 g (0.1) 1000–1500 g CSF volume (fold human) 0.04 ml (0.0004) 0.15 ml (0.0015) 12 ml (0.12) 15 ml (0.15) 100–150 ml CSF turnovers/day (fold human) 12.5 Â (2.5) 28.8 Â (5.76) 5.75 Â (1.15) 4 Â (0.8) 5Â Posture Quadrupedal Quadrupedal Quadrupedal Semi-bipedal Bipedal From Pardridge (1991). 6 | TOXICOLOGICAL SCIENCES, 2016, Vol. 152, No. 1 atLibraryonJune27,2016http://toxsci.oxfordjournals.org/Downloadedfrom
- 5. been determined. For the brain, that involves at least 3 trans- verse or sagittal sections through the site of administration and the region traversed by the device, with sufficient additional sections to characterize any distant effects. It is useful to pro- duce full transverse sections including both hemispheres in studies where a device traverses the brain. In general, at least 8–10 full transverse sections are required to evaluate the main brain regions in any species. For IT studies, multiple sections near the catheter tip will allow for a complete evaluation of changes. Inspection of the spinal cord for IT granuloma (Allen et al., 2006; Butt, 2011a) should be performed. Evaluating trans- verse and oblique sections of spinal cord increase the sensitivity for detecting changes. Typically, the spinal cord should be sec- tioned to include cervical, thoracic, catheter tip, and spinal cord/cauda equina caudal to the catheter tip regions. The objectives of the histological evaluation should be taken into account when determining the choices of tissue preserva- tion and staining reagents. Intravascular perfusion is recommended to minimize artifactual changes that often com- plicate microscopic interpretation (Garman, 2011). Peripheral nerves are best immediately fixed with a fixative containing glutaraldehyde to preserve myelin. Tissue sections may be em- bedded in paraffin or resin or frozen. Although paraffin allows for more detail than frozen, frozen sectioning may allow for im- proved immunohistochemistry and use of specialized stains (Switzer, 2000). Resin embedding is useful for optimal cross sec- tioning to preserve myelin. For all studies, paraffin embedded or frozen sections should be stained with hematoxylin and eosin (H&E) for general evalu- ation. In the brain and spinal cord, immunohistochemical stains to reveal astrocyte and microglial reactions can demon- strate glial cell changes not detectable by H&E. In acute studies, a stain that increases the sensitivity of detection of neuronal necrosis should be used, such as Fluoro-Jade (Schmued et al., 2005) or Cupric silver (Switzer, 2000). Other potentially useful stains include non-selective silver stains for axons, Luxol fast blue for myelin, neurofilament protein immunohistochemistry, and stains for specific neuronal populations. The combination of a longitudinal section in paraffin (H&E stain) and a cross sec- tion that has been osmicated, resin embedded, and stained with toluidine blue provides assessment of axonal degenera- tion, regeneration, and myelin alterations (Butt, 2011b). It is virtually impossible to prevent local damage when im- planting a CNS catheter. Inflammation, haemorrhage, and glio- sis are frequently encountered adjacent to the delivery device. Accumulation of fluid around the catheter track may be due to edema, and/or excess test article. Microscopic changes due to the delivery device are seldom associated with clinical signs and are not necessarily adverse, as they may be an unavoidable consequence of the mode of administration in the animal model and irrelevant to the intended clinical population. It can be challenging to differentiate the relative contributions of the test article and each component of the delivery system, even in properly controlled studies. USING NONCLINICAL STUDIES TO ENABLE FIRST IN HUMAN TRIALS The intended clinical regimen should guide the nonclinical pro- gram, with pivotal nonclinical studies should use the same route as that in the first in human trial. Distribution of the bio- logic to the target tissues/cells at pharmacologically active con- centrations should be demonstrated if possible. In addition, disposition of drug into the systemic compartment, and the re- lationship between CNS and systemic PK, should be character- ized. Toxicities revealed in the nonclinical studies should be monitored for in the clinic. For example, the presence of CNS in- flammation and elevated CSF white blood cells in nonclinical studies may lead to monitoring CSF cell counts clinically. The nonclinical studies should provide information about the ef- fects of the administration procedure, delivery device, vehicle, and test article, alone and in combination. It is expected that there will be a local reaction to CNS administered biologics, so consideration of the risk/benefit profile in the context of the pa- tient population is important. A safe starting dose can be determined using an appropriate safety factor and the pivotal nonclinical no observed adverse ef- fect level (NOAEL). For CNS administered biologics, brain mass or CSF volume can be used to normalize doses between species. If CSF volume is used, differences in the rates of turnover be- tween the different species should be considered (Table 2). An example of clinical safety factors determined based on a mon- key NOAEL scaled for differences in brain mass is illustrated in Table 3 (Felice et al., 2011; USFDA, 2005). Additional nonclinical studies may be needed to support the use of a delivery device in combination with the therapeutic. Utilizing the same or similar device in the nonclinical and clini- cal studies is desirable to demonstrate the safety of the drug- device combination. For developmental and reproductive toxicology studies, if warranted, the IV route should be used (Skov et al., 2007). FUTURE DIRECTIONS CNS administration of biologics is likely to play an increasing role in treating neurodegenerative disease in the future. Careful consideration of nonclinical program design will insure the suc- cess of these efforts. Nonclinical studies to enable clinical trials of CNS administered drugs must consider the clinical regimen, assessment of exposure in CSF, plasma, and/or CNS tissue, CNS effects, and the relevance of animal models to human patients. Nonclinical programs should be designed on a case-by-case ba- sis, carefully considering the clinical plan and the risk/benefit profile in the intended patient population. Interpretation of di- rect CNS administration studies is complicated by the histologi- cal changes attributable to the route of administration and presence of delivery devices in the CNS. Therefore, inclusion of applicable control groups is essential. CNS sampling for histo- pathological evaluation must be extensive, and may involve TABLE 3. Calculation of Clinical Safety Factors based on NOAEL from Pivotal Monkey Study Human (Pediatric; Brain 5 1 kg) Monkey (Brain 5 0.1 kg) Safety margin Clinical dose, mg mg/kg brain weight Nonclinical NOAEL, mg mg/kg brain weight 10 10 100 1000 100-fold 100 100 100 1000 10-fold VUILLEMENOT ET AL. | 7 atLibraryonJune27,2016http://toxsci.oxfordjournals.org/Downloadedfrom
- 6. serial sectioning of the entire brain as well as thorough sam- pling of spinal cord, dorsal nerve roots, and ganglia. In addition, use of multiple stains to illuminate specific neuronal changes is recommended. Prior to entry into first in human trials, a non- clinical program should describe the safety findings of the bio- logic in conjunction with the delivery device and vehicle, support the likely efficacy in the patient population, character- ize the PK and distribution, and provide rationale for inclusion of clinical endpoints of safety and efficacy. Therefore, a strong nonclinical data package is required to support these challeng- ing but increasingly worthwhile clinical trials. REFERENCES Akdogan, I., Kiroglu, Y., Onur, S., and Karabuluti, N. (2010). The volume fraction of brain ventricles to total brain volume: A computed tomography stereological study. Folia Morphol. 69, 193–200. Allen, J., Horais, K., Tozier, N., Wegner, K., Corbeil, J., Mattrey, R., Rosi, S., and Yaksh, T. (2006). Time course and role of mor- phine dose and concentration in intrathecal granuloma for- mation in dogs. Anesthesiology 105, 581–590. Aspelund, A., Antila, S., Proulx, S. T., Karlsen, T. V., Karaman, S., Detmar, M., Wiig, H., and Alitalo, K. (2015). A dural lymphatic vascular system that drains brain interstitial fluid and mac- romolecules. J. Exp. Med. 29, 991–999. Barua, N. U., Gill, S. S., and Love, S. (2014). Convection-enhanced drug delivery to the brain: Therapeutic potential and neuro- pathological considerations. Brain Pathol. 24, 117–127. Bauer, H. C., Krizbai, I. A., Bauer, H., and Traweger, A. (2014). “You Shall Not Pass”-tight junctions of the blood brain bar- rier. Front. Neurosci. 8, 392. Beck, M., Flachenecker, P., Magnus, T., Giess, R., Reiners, K., Toyka, K. V., and Naumann, M. (2005). Autonomic dysfunc- tion in ALS: A preliminary study on the effects of intrathecal BDNF. Amyotroph. Lateral Scler. Other Motor Neuron. Disord. 6, 100–103. Beutler, A. S., Banck, M. S., Walsh, C. E., and Milligan, E. D. (2005). Intrathecal gene transfer by adeno-associated virus for pain. Curr. Opin. Mol. Ther. 7, 431–439. Bolon, B., Garman, R., Pardo, I., Jensen, K., Butt, M., et al. (2012). STP position paper: Recommended practices for sampling and processing the nervous system (brain, spinal cord, nerve and eye) during nonclinical general toxicity studies. Toxicol. Pathol 41, 1028–1048. Bonnan, M., Ferrari, S., Bertandeau, E., Demasles, S., Krim, E., Miquel, M., and Barroso, B. (2014). Intrathecal rituximab ther- apy in multiple sclerosis: Review of evidence supporting the need for future trials. Curr. Drug Tar. 15, 1205–1214. Bulat, M., and Klarica, M. (2011). Recent insights into a new hy- drodynamics of the cerebrospinal fluid. Brain Res. Rev. 1, 99–112. Butt, M. T. (2011a). Morphologic changes associated with intra- thecal catheters for direct delivery to the central nervous system in preclinical studies. Toxicol. Pathol. 39, 213–219. Butt, M. T. (2011b). Evaluation of the adult nervous system. In Fundamental Neuropathology for Pathologists and Toxicologists: Principles and Techniques (B Bolon and M Butt, Eds.), pp. 321–338. Wiley and Sons, Hoboken, NJ. Dickson, P., McEntee, M., Vogler, C., Le, S., Levy, B., Peinovich, M., Hanson, S., Passage, M., and Kakkis, E. (2007). Intrathecal en- zyme replacement therapy: Successful treatment of brain disease via the cerebrospinal fluid. Mol. Genet. Metab. 91, 61–68. Eriksdotter Jo¨nhagen, M., Nordberg, A., Amberla, K., B€ackman, L., Ebendal, T., Meyerson, B., Olson, L., Seiger, Shigeta, M., Theodorsson, E., et al. (1998). Intracerebroventricular infu- sion of nerve growth factor in three patients with Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 9, 246–257. Felice, B. R., Wright, T. L., Boyd, R. B., Butt, M. T., Pfeifer, R. W., Pan, J., Ruiz, J. A., Heartlein, M. W., and Calias, P. (2011). Safety evaluation of chronic intrathecal administration of idursulfase-IT in cynomolgus monkeys. Toxicol. Pathol. 39, 879–892. Fricker, G., and Miller, D. S. (2004). Modulation of drug transpor- ters at the blood-brain barrier. Pharmacology 70, 169–176. Garman, R. (2011). Common histological artifacts in nervous sys- tem tissues. In Fundamental Neuropathology for Pathologists and Toxicologists Principles and Techniques. (B Bolon and M Butt, Eds.), pp 191–201. J Wiley and Sons, Hoboken, NJ. Greitz, D. (1993). Cerebrospinal fluid circulation and associated intracranial dynamics. A radiologic investigation using MR imaging and radionuclide cisternography. Acta Radiol. Suppl. 386, 1–23. Hirai, T., Enomoto, M., Kaburagi, H., Sotome, S., Yoshida-Tanaka, K., Ukegawa, M., Kuwahara, H., Yamamoto, M., Tajiri, M., Miyata, H., et al. (2014). Intrathecal AAV serotype 9-mediated delivery of shRNA against TRPV1 attenuates thermal hyper- algesia in a mouse model of peripheral nerve injury. Mol. Ther. 22, 409–419. Hollak, C. E., and Wijburg, F. A. (2014). Treatment of lysosomal storage disorders: Successes and challenges. J. Inherit. Metab. Dis. 37, 587–598. Iliff, J. J., Wang, M., Liao, Y., Plogg, B. A., Peng, W., Gundersen, G. A., Benveniste, H., Vates, G. E., Deane, R., Goldman, S. A., et al. (2012). A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial sol- utes, including amyloid b. Sci. Transl. Med. 4, 147ra111. Jaime-Pe´rez, J. C., Rodrıguez-Romo, L. N., Gonzalez-Llano, O., Chapa-Rodrıguez, A., and Gomez-Almaguer, D. (2009). Effectiveness of intrathecal rituximab in patients with acute lymphoblastic leukaemia relapsed to the CNS and resistant to conventional therapy. Br. J. Haematol. 144, 794–795. Kan, S. H., Aoyagi-Scharber, M., Le, S. Q., Vincelette, J., Ohmi, K., Bullens, S., Wendt, D. J., Christianson, T. M., Tiger, P. M., Brown, J. R., et al. (2014). Delivery of an enzyme-IGFII fusion protein to the mouse brain is therapeutic for mucopolysac- charidosis type IIIB. Proc. Natl. Acad. Sci. U S A 111, 4870–14875. Katz, M. L., Coates, J. R., Sibigtroth, C. M., Taylor, J. D., Carpentier, M., Young, W. M., Wininger, F. A., Kennedy, D., Vuillemenot, B. R., and O’Neill, C. A. (2014). Enzyme replacement therapy attenuates disease progression in a canine model of late- infantile neuronal ceroid lipofuscinosis (CLN2 disease). J. Neurosci. Res. 92, 1591–1598. Kim, K. H., Decker, C., and Burton, B. K. (2008). Successful man- agement of difficult infusion-associated reactions in a young patient with mucopolysaccharidosis type VI receiving re- combinant human arylsulfatase B (galsulfase [Naglazyme). Pediatrics 121, e714–e717. Miller, T. M., Pestronk, A., David, W., Rothstein, J., Simpson, E., Appel, S. H., Andres, P. L., Mahoney, K., Allred, P., Alexander, K., et al. (2013). An antisense oligonucleotide against SOD1 delivered intrathecally for patients with SOD1 familial amyo- trophic lateral sclerosis: A phase 1, randomised, first-in-man study. Lancet Neurol. 12, 435–442. Muenzer, J., Hendriksz, C. J., Fan, Z., Vijayaraghavan, S., Perry, V., Santra, S., Solanki, G. A., Mascelli, M. A., Pan, L., Wang, N., 8 | TOXICOLOGICAL SCIENCES, 2016, Vol. 152, No. 1 atLibraryonJune27,2016http://toxsci.oxfordjournals.org/Downloadedfrom
- 7. et al. (2016). A phase I/II study of intrathecal idursulfase-IT in children with severe mucopolysaccharidosis II. Genet. Med. 18, 73–81. Munoz-Rojas, M. V., Vieira, T., Costa, R., Fagondes, S., John, A., Jardim, L. B., Vedolin, L. M., Raymundo, M., Dickson, P. I., Kakkis, E., et al. (2008). Intrathecal enzyme replacement ther- apy in a patient with mucopolysaccharidosis type I and symptomatic spinal cord compression. Am. J. Med. Genet. 146A, 2538–2544. Mu~noz-Rojas, M. V., Horovitz, D. D., Jardim, L. B., Raymundo, M., Llerena, J. C., Jr, de Magalh~aes Tde, S., Vieira, T. A., Costa, R., Kakkis, E., and Giugliani, R. (2010). Intrathecal administration of recombinant human N-acetylgalactosamine 4-sulfatase to a MPS VI patient with pachymeningitis cervicalis. Mol. Genet. Metab. 99, 346–350. Nutt, J. G., Burchiel, K. J., Comella, C. L., Jankovic, J., Lang, A. E., Laws, E. R., Jr, Lozano, A. M., Penn, R. D., Simpson, R. K., Jr, Stacy, M., et al. (2003). Implanted intracerebroventricular. Glial cell line-derived neurotrophic factor. Randomized, dou- ble-blind trial of glial cell line-derived neurotrophic factor (GDNF) in PD. Neurology 60, 69–73. Oliveira, M., Braga, S., Passos-Coelho, J. L., Fonseca, R., and Oliveira, J. (2011). Complete response in HER2þ leptomenin- geal carcinomatosis from breast cancer with intrathecal tras- tuzumab. Breast Cancer Res. Treat. 127, 841–844. Oreskovic, D., and Klarica, M. (2010). The formation of cerebro- spinal fluid: Nearly a hundred years of interpretations and misinterpretations. Brain Res. Rev. 64, 241–262. Pardridge, W. M. (1991). Peptide Drug Delivery to the Brain. Raven Press, New York. Patel, N. K., Bunnage, M., Plaha, P., Svendsen, C. N., Heywood, P., and Gill, S. S. (2005). Intraputamenal infusion of glial cell line-derived neurotrophic factor in PD: A two-year outcome study. Ann. Neurol. 57, 298–302. Patil, S. A., and Maegawa, G. H. (2013). Developing therapeutic approaches for metachromatic leukodystrophy. Drug Des. Devel. Ther 7, 729–745. Pfeifer, R. W., Felice, B. R., Boyd, R. B., Butt, M. T., Ruiz, J. A., Heartlein, M. W., and Calias, P. (2012). Safety evaluation of chronic intrathecal administration of heparan N-sulfatase in juvenile cynomolgus monkeys. Drug Deliv. Transl. Res. 2, 187–200. Provencio, J. J., Kivisakk, P., Tucky, B. H., Luciano, M. G., and Ranshoff, R. M. (2005). Comparison of ventricular and lumbar cerebrospinal fluid T cells in non-inflammatory neurological disorder (NIND) patients. Neuroimmunology 163, 179–184. Richard, I., and Menei, P. (2007). Intrathecal baclofen in the treat- ment of spasticity, dystonia and vegetative disorders. Acta Neurochir. 97, 213–218. Rubenstein, J. L., Fridlyand, J., Abrey, L., Shen, A., Karch, J., Wang, E., Issa, S., Damon, L., Prados, M., McDermott, M., et al. (2007). Phase I study of intraventricular administration of rituximab in patients with recurrent CNS and intraocular lymphoma. J. Clin. Oncol. 25, 1350–1356. Rubalcava, M. A., and Sotelo, J. (1995). Differences between ven- tricular and lumbar cerebrospinal fluid in hydrocephalus secondary to cysticercosis. Neurosurgery 37, 668–671. Sakka, L., Coll, G., and Chazal, J. (2011). Anatomy and physiology of cerebrospinal fluid. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 128, 309–316. Schmued, L., Stowers, C., Scallet, A., and Xu, L. (2005). Fluoro- Jade results in ultra high resolution and contrast labelling of degenerating neurons. J. Brain Res. 1035, 24–31. Schultz, M. L., Tecedor, L., Chang, M., and Davidson, B. L. (2011). Clarifying lysosomal storage diseases. Trends Neurosci. 34, 401–410. Skov, M. J., Beck, J. C., de Kater, A. W., and Shopp, G. M. (2007). Nonclinical safety of ziconotide: An intrathecal analgesic of a new pharmaceutical class. Int. J. Toxicol. 26, 411–421. Storkebaum, E., Lambrechts, D., Dewerchin, M., Moreno- Murciano, M. P., Appelmans, S., Oh, H., Van Damme, P., Rutten, B., Man, W. Y., De Mol, M., et al. (2005). Treatment of motoneuron degeneration by intracerebroventricular deliv- ery of VEGF in a rat model of ALS. Nat. Neurosci. 8, 85–92. Switzer, R. (2000). Application of silver degeneration stains for neurotoxicity testing. Toxicol. Pathol. 28, 70–83. Switzer, R. (2011). Fundamentals of neurotoxicity detection. In Fundamental Neuropathology for Pathologists and Toxicologists Principles and Techniques. (B Bolon and M Butt, Eds.), pp. 139–157. Wiley and Sons, Hoboken, NJ. Tajes, M., Ramos-Fernandez, E., Weng-Jiang, X., Bosch-Morato, M., Guivernau, B., Eraso-Pichot, A., Salvador, B., Fernandez- Busquets, X., Roquer, J., and Mu~noz, F. J. (2014). The blood- brain barrier: Structure, function and therapeutic approaches to cross it. Mol. Membr. Biol. 31, 152–167. Torres-Corzo, J. G., Tapia-Pe´rez, J. H., Sanchez-Aguilar, M., Della Vecchia, R. R., Chalita Williams, J. C., and Cerda-Gutie´rrez, R. (2009). Comparison of cerebrospinal fluid obtained by ventric- ular endoscopy and by lumbar puncture in patients with hy- drocephalus secondary to neurocysticercosis. Surg. Neurol. 71, 376–379. USFDA. 2005. Guidance for industry: Estimating the maximum safe starting dose in initial clinical trials for therapeutics in adult healthy volunteers. http://www.fda.gov/downloads/ Drugs/.../Guidances/UCM078932.pdf Vuillemenot, B. R., Katz, M. L., Coates, J. R., Kennedy, D., Tiger, P., Kanazono, S., Lobel, P., Sohar, I., Xu, S., Cahayag, R., et al. (2011). Intrathecal tripeptidyl-peptidase 1 reduces lysosomal storage in a canine model of late infantile neuronal ceroid lipofuscinosis. Mol. Genet. Metab. 104, 325–337. Vuillemenot, B. R., Kennedy, D., Reed, R. P., Boyd, R. B., Butt, M. T., Musson, D. G., Keve, S., Cahayag, R., Tsuruda, L. S., and O’Neill, C. A. (2014). Recombinant human tripeptidyl pepti- dase-1 infusion to the monkey CNS: Safety, pharmacokinet- ics, and distribution. Toxicol. Appl. Pharmacol. 277, 49–57. Vuillemenot, B. R., Kennedy, D., Cooper, J. D., Wong, A. M., Sri, S., Doeleman, T., Katz, M. L., Coates, J. R., Johnson, G. C., Reed, R. P., et al. (2015). Nonclinical evaluation of CNS-administered TPP1 enzyme replacement in canine CLN2 neuronal ceroid lipofuscinosis. Mol. Genet. Metab. 114, 281–293. Williams, J. A., Day, M., and Heavner, J. E. (2008). Ziconotide: An update and review. Exp. Opin. Pharmacother. 9, 575–583. Xu, S., Wang, L., El-Banna, M., Sohar, I., Sleat, D. E., and Lobel, P. (2011). Large-volume intrathecal enzyme delivery increases survival of a mouse model of late infantile neuronal ceroid lipofuscinosis. Mol. Ther. 19, 1842–1848. Yang, L., Kress, B. T., Weber, H. J., Thiyagarajan, M., Wang, B., Deane, R., Benveniste, H., Iliff, J. J., and Nedergaard, M. (2013). Evaluating glymphatic pathway function utilizing clinically rele- vant intrathecal infusion of CSF tracer. J. Transl. Med. 11, 107. VUILLEMENOT ET AL. | 9 atLibraryonJune27,2016http://toxsci.oxfordjournals.org/Downloadedfrom