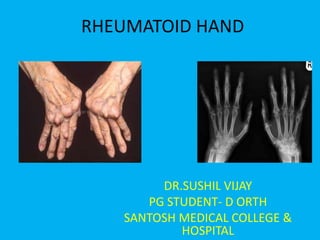
Rheumatoid hands
- 1. RHEUMATOID HAND DR.SUSHIL VIJAY PG STUDENT- D ORTH SANTOSH MEDICAL COLLEGE & HOSPITAL
- 2. Rheumatism • Rheumatism is any painful disorder affecting the loco-motor system including joints, muscles, connective tissues, soft tissues around the joints, and bones. This also includes rheumatic fever affecting heart valves.
- 3. Origin • The term ''rheumatology'' originates from the Greek word ''rheuma'', meaning “ something that which flows as a river or stream," and the suffix ''-ology'', meaning "the study of."
- 4. • Rheumatoid arthritis is a chronic, systemic, inflammatory disease, most often involving the small joints of the hands and feet, although any synovial joint can be affected
- 5. Rheumatoid arthritis : overview • It is most common* type of chronic inflammatory rheumatic disorder. • The term inflammatory rheumatic disorder covers a group of disorder that causes pain, stiffness, and swelling around joints and tendons.
- 6. Rheumatoid arthritis • Basically , it is a systemic disease of young and middle aged adults characterised by proliferative and destructive changes in synovial membrane, periarticular structures, skeletal muscles and perineural sheaths. • Eventually, joints are destroyed , fibrosed or ankylosed. It is a widespread vasculitis of the small arterioles.
- 7. Etiology • Still incompletely worked out. • Important factors in evolution are – Genetic susceptibility – An immunological reaction – An inflammatory reaction – The appearance of Rh factor in blood and synovium – Articular cartilage destruction
- 8. Genetic susceptibility • More common in first degree relatives • HLA DR4 +ve in 70% of people with RA.
- 9. Inflammatory reaction • In joints and tendon sheath. • As the APC/T cell interaction is initiated, various local factors comes into play and leads to a progressive enhancement of immune response. • There is a marked proliferation of cells in the synovium, with the appearances of new blood vessel formation. • Cytokines activate inflammatory cells like macrophage and B cells. • Some cytokines-chemokines attract other inflammatory cells to area. • Importanat cytokines are :- TNF, IL-1 and IL-6. • The resulting synovitis, both in joints and tendon sheath lining , is the hallmark of early RA.
- 10. Chronic synovitis and joint destruction • Immune complexes are deposited in synovium and on the articular cartilage, where they appear to augment the inflammatory process. • This leads to depletion of cartilage matrix and eventually damage to cartilage and underlying bone. Vascular proliferation and osteolytic activity most marked at the edges of the articular surface, may contribute further to the cartilage destruction and peri articular bone erosion.
- 11. Rheumatoid factor • B cell activation in RA leads to the production of anti – IgG autoantibodies which are detected in the blood as ‘rheumatoid factor’ • High levels are likely inflammatory in origin. Low levels may normally be present in individuals. • Other autoantibodies idenified are anti-CCP antibodies. Its presence is very specific for RA.
- 12. Pathology- Joints & tendons • 4 stages:- • Stage 1- Pre-clinical- (Only raised ESR, CRP and RF) • Stage-II- Synovitis • Stage III- Destruction • Stage IV- Deformity
- 13. Pathology • Due to synthesis of autoantibodies, against unknown antigenic antigens in the synovium, primary synovitis sets in. • Primary synovitis Pannus formation forms villus. • Villus migrates towards the joint causing its destruction and ankylosis, fibrous in early stage and bony in late stages. • Pannus- medical term for an abnormal layer of fibrovascular tissue or granulation tissue • Villus- any of the small, slender, vascular projections that increase the surface area of a membrane.
- 14. Rheumatoid arthritis = synovitis+vasculitis+granuloma SYNOVITIS GRANULOMA VASCULITIS FORMATION
- 15. Pathological process Tissue involved Results in Deformities Vasculitis Joint structures Synovitis-effusion, Swelling, stiffness, Necrosis articular cartilage instability , Fibrosis destruction, subluxation or Pericapsulitis, dislocation Ligamentous instability Arthritis Intrinsic plus deformity Plasma cell Tendon Tenosynovitis, rupture Ulnar deviation of proliferation fingers, concertina collapse of fingers. Granulation tissue and Muscle Wasting, atrophy, Contracture, ankylosis pannus formation fibrosis Synovial hypertrophy : Bone Osteoporosis-thin in joint, in tendon cortex loss of trabeculae, cyst formation- subchondral erosions, destruction
- 17. RA:- Clinical features • Insideous onset • Ocassionally acute • Early stages:- polysynovitis, soft tissue swelling and stiffness. • Female predominance • Swelling and loss of mobility in PIP of fingers. • Other joints involved-wrists, feet, knees and shoulders in order of frequency.
- 18. RA:-Clinical features • Another classic feature generalised stiffness after period of inactivity and especially after rising from bed in the early morning, usually lasts longer than 30 minutes. • Physical signs may be minimal, but usually there is symmetrically distributed swelling and tenderness of the MCP joints, the PIP and the wrists. • Tenosynovitis is common in the extensor compartments of the wrist and flexor sheath of the fingers, diagnosed by feeling thickness , tenderness and crepitations over back of the wrist or the palm while passively moving the fingers.
- 19. RA:- Clinical features • If larger joints are involved, local warmth, synovial hypertrophy and intraarticular effusion may be obvious. • In late stages:- joint deformity increases and the acute pain of synovitis is replaced by the more constant ache of progressive joint destruction. • The combination of the joint instability and the tendon rupture produces the typical ‘rheumatoid deformities, ulnar deviation of the fingers, radial, and volar displacement of the wrists, valgus knees, valgus feet and clawed toes.
- 20. RA:- Clinical features • Joint movements are restricted and often very painful. • Cervical spine may be involved • Daily activities hampered.
- 22. Extra articular manisfestations • mercer
- 24. Investigations • 1. CBC- Hb low, normochromic hypochromic anemia. WBC’s or normal, lymphocytes and ESR . • 2. Serological tests :- • Rheumatoid factor:- this in presence of gamma globulins agglutinates certain strains of streptococci sensitized by sheep cells and latex prticles.
- 25. • Latex fixation test:- Unknown serum + 7- globulin latex suspension. agglutination +ve when If –ve , do more sensitive serum has test as there is less RA abundant RAF factor in the serum
- 26. • Inhibition test :- This test uses the characterstics of Euglobulin from unknown serum. Euglobulin from normal serum neutralise the rheumatoid factor thereby inhibiting agglutination. • Euglobulin from rheumatoid serum has no effect on the rheumatoid factor and agglutination occurs. • This is most sensitive test , positive even with minute amounts of RA factor.
- 27. RA serum of known high agglutination activity + Unknown euglobulin + Standard 7-globulin latex suspension Agglutination occurs Unknown serum -ve latex test +ve inhibition test RA SLE (Le cell phenomenon)
- 28. Others • C reactive proteins (inc.) • Alkaline phosphatase (Inc) • Platelets( Inc) • Serum albumin (Dec) • Anti CCP • ANA may be +nt.
- 29. • Synovial fluid – not for diagnosis but to rule out other causes of infection. • Fluid in RA is typically yellow, turbid and watery due to high WBC and low sugar content. • MRI :- Info about extent of soft tissue involvement and damage
- 30. Classification criteria • Different classification systems have evolved for the diagnosis of rheumatoid arthritis with time.
- 31. 1987 criteria
- 34. Treatment • 1. General measures • 2. Splints • 3. Drugs • 4. Surgical intervention
- 35. 1. General measures • Aims to improve G.C of the patient and to keep joints properly splinted in functional position to guard against the ensuing ankylosis. • Rest in bed • Good diet, rich in proteins and minerals • Correct anemia- hematinics or transfusion • Hormones to improve bone stock • Removal of any infective foci.
- 36. 2. Splints • Splinting in functional position helps avoid ankylosis. • Removed daily • Hot packs given or Hubbard tanks used and joints are put into full range of motion • With splints , muscle setting exercises advocated and after removal of splints resistance exercises begun.
- 37. Hubbard tanks
- 38. 3. Drugs • Three classes used:- • 1. Analgesics • 2. Anti inflammatory • 3. Disease modifying drugs
- 39. • No treatment is ideal and it is important to assess the patient's response so that the most effective regimen is adopted. • Commonly used methods of assessment include; duration of early morning stiffness, number of tender swollen joints. Functional assessment ESR, radiographs, etc.
- 40. • First Line of Drugs: NSAIDs • These are aspirin/ibuprofen/ketoprofen/diclofenac sodium/ naproxen/piroxicam, etc.
- 41. Second Line of Drugs • Second line of drugs are used only if an adequate trial of first line drugs have failed to relieve symptoms satisfactorily or if there is radiological evidence of progressive disease. Second line drugs are alternatively known as disease-modifying antirheumatic drugs (DMARD) and are slow acting drugs. When second line therapy is introduced, sympto- matic NSAIDs need to be continued in parallel
- 42. Commonly prescribed drugs include: • • Injectable gold and oral gold (sodium aurothiomalate). This is no longer preferred. • Penicillamine • Sulphasalazine • Antimalarial drugs (e.g. chloroquine) • Dapsone and levamisole. • The choice of the drug to be given first will depend on the experience of the doctor and on the facilities available for monitoring. There is little evidence to suggest which drug should be prescribed first. Methotrexate has now emerged as the drug of choice due to its higher efficacy. Early institution and escalation of MTX to its maximum tolerable dose is the latest mantra.
- 43. Antimalarial Drugs • They do not require intensive blood monitoring and if these facilities are limited, chloroquine or hydroxy chloroquine can be particularly used. • Other agents known to have second line drug effect include levamisole and dapsone. Levamisole is not freely available in some countries and its toxicity seems to be greater than that of gold and penicillamine. Dapsone has a high toxicity
- 44. Quick facts of second line drugs • Used only if first line fails. • • Known as DMARD. • To be continued for at least 6 months. • Parallel NSAID is to be used. • Choice of drugs is based on clinicians' experience. • Antimalarial drugs are used if proper blood monitoring is not available. • All drugs are toxic.
- 45. Third Line of Drugs • Azathioprim, cyclophosphamide and chlorambucil can exert a second line effect inpatients with rheumatoid arthritis
- 46. • Corticosteroids: Cyclosporine has been tried in patients with rheumatoid arthritis. The fact that it does not affect WBC is a theoretical advantage in patients with Felty's syndrome.
- 47. Newer Drugs for Rheumatoid Arthritis • Tumor Necrosis Factor (INF u-blockers) For example: a. Etanarcept (25 mg/subcutaneous, twice a week) b. Infliximab (2 mg/kg at 0, 6, 8 and weekly. IV infusions combined with oral methotrexate). c. Interleukin- 1 receptor antagonist (IL-IRA) Dose-100 mg/day by subcutaneous injection. Indications • Failure of at least two standard DMARD drugs one of which is always methotrexate despite adequate trials (i .e. 6 months). • Leflunomide (Immunomodulatory drug) Indicated dose is 100 mg/day for 3 days then 20 mg/ day.
- 48. 4. Surgical intervention: Goals • Goals of surgery are to relieve pain, restore function, correct or prevent deformity, and inhibit disease progression
- 49. • A consideration in surgical intevention of rheumatoid arthritis is the risk of anesthesia. Most hand and wrist procedures can be performed under regional anesthesia which are generally safer, allow a quicker recovery and provide better post op pain relief than gen anesthesia. If a GA is considered than lateral flexion and extension radiograph of cervical spine must be obtained to rule out C1-C2 instability.
- 50. Treatment • Procedures usually considered for patients with rheumatoid arthritis include • tenosynovectomy, • tendon repair or realignment, • synovectomy, • arthroplasty, and • arthrodesis.
- 51. Modus operandi of surgical procedures in rheumatoid arthritis • Synovectomy - Failed chemotherapy - Joint destruction should be minimal - Useful in knee/ankle • Osteotomy - Less than 60 years of age - When joint is partially damaged - Commonly done at hip (Intertrochanteric osteotomy and abduction osteotomy) • Arthrodesis - Long-term relief -Reserved for peripheral joints where arthroplasty results in pain -Causes secondary osteoarthritis in bigger joints • Arthroplasty -Advanced stages in hip and knee
- 52. Rheumatoid Hand
- 53. Rheumatoid Wrist • After MCP joints , most common site for RA.
- 54. Pathology • Early stage:- Synovitis of joint and tendon sheath. • If disease persist:- DRUJ, R-C joints and intercarpal joints eroded attenuation of ligaments and tendons unstable wrist & hand.
- 55. • The ulnar side of carpus goes into flexion and ulnar subluxation, causing head of ulna to jut out prominently on dorsum of wrist. • Proximal carpal row slides ulnarwards & the metacarpal bone deviate radialwardsreciprocal ulnar deviation of fingers cardinal feature of rheumatoid hand. • Scaphoid falls into flexion d/t erosion of interosseus lig and loss of carpal height. • This combination of instability and erosive tenosynovitis eventually leads to tendon rupture-typically one or more of extensors tendons.`
- 56. Clinical features • Early-Pain, swelling and stiffness of wrist. • Swelling initially localised to common extensor tendon sheath or extensor carpi ulnaris, but as time progresses the joint becomes thickened and tender. • Swelling of synovium in carpal tunnel may cause median nerve compression. • Articular surface erode + ligament attenuated unstable wrist. • Early infiltration of tendons may lead to weakness of wrist extension and flexion.
- 57. • Piano key sign- Instability of DRUJ aggravates dorsal protrusion of the ulnar head, which can be often jogged up and down by pressing upon it with thumb. • Tendon lesions in late stage. • First to rupture EDM EC of little and ring finger. • EPL is vulnerable. • Flexor tendons may also rupture in digital sheaths or in carpal tunnel.
- 58. X rays • Peri articular osteoporosis + erosion of ulnar styloid and the radio carpal and IP joints
- 59. Treatment • Early stage :- Objective is to relieve pain and counteract synovitis. • Systemic treatment + intermittent splintage + intrasynovial injections of corticosteroids.
- 60. Established disease:- After joint erosion starts focus should be on joint stability and prevention of deformity. Extensor tenosynevectomy and soft tissue stabilization of the wrist may forestall further deterioration. Through a dorsal longitudinal incision the extensor retinaculum is expose and carefully dissected but left attached at the radial side. The thickened synovium around the extensor tendons, as well as any bony protrusions on the back of the wrist, are removed. The preserved extensor retinaculum is then placed beneath the tendons to further reduce the risk of later tendon rupture.
- 61. • If the radio-ulnar joint is involved, svnovectomv can be combined with excision of the ulnar head and trans position of the extensor carpi radialis longus to the ulnar side of the wrist (to counteract the tendency to radial deviation). • Fusion of the Iunate to the radius (chamay procedure) prevents ulnar slide of the carpus.
- 62. • Flexor tenosynovitis is not as obvious as extensor tendon involvement. • May present as carpal tunnel syndrome (median nerve compression by swollen tendons in the carpal tunnel) which requires open release of the flexor retinaculum and tenosynovectomv.
- 63. • Obvious bony protrusions in the floor of the carpal tunnel (due to carpal collapse) should be removed and the raw area covered with a soft-tissue flap. • Median nerve symptoms in patients with rheumatoid arthritis may be caused by pathology in the proximal part of the limb or the cervical spine, so these patients should always undergo nerve conduction studies and electromyography before the carpal tunnel decompression.
- 64. LATE DISEASE • Tendon ruptures at the wrist, joint destruction, instability and deformity may require reconstructive surgery • Ruptured extensor tendons can seldom be repaired; side-to-side suture of a distal tendon stump to an adjacent tendon, tendon grafting or tendon transfer gives a satisfactory if not perfect result.
- 65. • Rupture of the flexor pollicis longus tendon in the carpal tunnel may be caused by scuffing of the tendon against the distal pole of the scaphoid or the edge of the trapezium - the so-called `Mannerfelt lesion'.
- 66. • Painful joint destruction, instability and deformity can be dealt with by either joint replacement or arthrodesis. • Arthroplasty using a silicone `spacer' has a high failure rate; silicone synovitis and the difficulty of revision have led to it being abandoned. • Total wrist replacement with a metal- polyethylene device is becoming more reliable, but is only suitable for those with well- preserved bone stock.
- 67. • Arthrodesis is widely considered to be the best option for dealing with painful instability in the radio-carpal joint. • If the wrist is already 'fusing' itself spontaneously, simple stabilization with a Steinman pin passed between the second and third metacarpals, across the carpus and into the distal radius is all that is needed.
- 68. • Bone grafts are not necessarily added but can be taken from the ulnar head if it is excised. For patients with better bone stock, pin fixation is inadequate; formal arthrodesis with a wrist fusion plate is preferable. In this group, ulnar head replacement rather than ulnar head excision should be considered.
- 69. • As a general rule, wrist deformities should be corrected before hand deformities. • Furthermore the dominant wrist should, if possible, be fused in slight extension to provide reliable power grip, while the non- dominant wrist is fused in some flexion (or replaced) so as to provide the posture needed for perineal care.
- 70. Wrist arthroplasty Two types • 1. Resection arthroplasty with or without soft tissue interposition and • 2. Implant arthroplasty • Palmar shelf arthoplasty* a type of resection arthroplasty.
- 71. Palmar shelf arthroplasty • In this the distal radius is resected so that it is perpendicular to the longitudinal axis of radius in AP and lateral planes. • Shallow socket is then created in the distal radius with a small volar lip to keep the carpus from subluxating anteriorly. • The carpus is reduced into socket and held with k wires temporarily. • The volar capsule is detached proximally and sutured to the dorsal rim of the radius which creates a soft tissue interposition that discourages volar carpal dislocation. • The dorsal capsule is repaired , any necessary extensor tendon procedures are performed and the skin is closed over a drain.
- 72. CAPUT ULNAE SYNDROME • Involvement of DRUJ. (blackdahl, 1963) • Characterised by prominent appearing distal ulna. • Develops as the supporting ligaments around the distal ulna deteriorate and the extensor carpi ulnaris subluxates anteriorly causing flexion and supination of the carpus. • Infact the prominence of distal ulna is in part secondary to the combined anterior subluxation and supination of the carpus.
- 73. Cont:- • C/o pain over ulnar border of wrist Aggravated by pronation and supination. • O/e swelling & tenderness over ulnar head. • Combination of prominence of distal ulna & tenosynovitis leads to rupture of EDQ and the EDC tendons to ring and small fingers.
- 74. • Surgical Tt. Depends on degree of involvement. • Synevctomy, reconstruction of supporting ligaments and ECQ translocation alone rarely. (if no evidence of articular cartilage destruction.) • Usually head impossible to save . • Thus distal ulna resected with ligament reconstruction & ECU translocation. • After resection ulnar translocation, volar sublux & supination of carpus.
- 75. RA -HAND
- 76. RA-Hand • The hand – most common site. • The early stage is characterized by synovitis of the joints and tendon sheaths. • As disease progresses joint and tendon erosions mechanical derangement. • In late stage joint destruction, attenuation of the ligaments and tendon rupturesinstability and progressive deformity.
- 77. Clinical features • Stiffness and swelling of the fingers are early symptoms. • Sometimes the first symptoms are typical of carpal tunnel compression, caused by flexor tenosynovitis at the wrist
- 78. On examination • Swelling of the MCP and PIP joints, giving the fingers a spindle shape. • Usually bilaterally similar. • Swelling of tendon sheaths is usually seen on the dorsum of the wrist and along the ulnar border (extensor carpi ulnaris). • Thickened flexor tendons may also felt on the volar aspect of the proximal phalanges. • Joints are tender and crepitus may be felt on moving the tendons. Joint mobility and grip strength diminished.
- 79. • As the disease progresses:- • slight radial deviation of the wrist and ulnar deviation of the fingers, • correctable swan neck deformities of some fingers. • an isolated boutonniere or the sudden appearance of a drop-finger or mallet thumb (from extensor tendon rupture).
- 80. • In late stage, after inflammation subsides, established deformities are the rule. • the carpus settles into radial tilt and volar subluxation. • there is marked ulnar drift of the fingers and volar dislocation of the MCP joints, often associated with multi swan-neck and boutonniere deformities. • These rheumatoid deformities' are so characteristic that they allow the diagnosis to be made at first glans. When the abnormalities become fixed, functional loss may be so severe that patients can no longer dress and feed themselves.
- 81. General features • 1. Weakness:- Rheumatoid hands are weak because of combination of generalized muscular weakness, pain inhibition, tendon malalignment or rupture, joint stiffness and nerve compression. • 2. Rheumatoid nodules:- These arc associated with aggresive disease in seropositive patients. They tend occur at pressure areas (e.g. the pulps of the fingers and the radial side of the index finger).
- 82. • 3. Z-collapse :- If one of two adjacent joints changes direction, then the overlying long tendons will pull the other joint into the opposite direction.
- 83. • 4. Deformities – Intrinsic plus deformity – Swan neck deformity – Boutonniere’s deformity
- 84. Intrinsic plus deformity • caused by tightness and contracture of the intrinsic muscles • the proximal interphalangeal joint cannot be flexed while the metacarpophalangeal joint is fully extended • volar subluxation of the metacarpophalangeal joints and ulnar deviation of the fingers may be associated.
- 85. • Bunnell test for intrinsic tightness is done.
- 86. Swan-Neck Deformity • Swan-neck deformity is described as a flexion posture of the distal interphalangeal joint and hyperextension posture of the proximal interphalangeal joint, at times with flexion of the metacarpophalangeal joint. • It is caused by muscle imbalance and may be passively correctable, depending on the fixation of the original and secondary deformities. Although usually associated with rheumatoid arthritis, swan-neck deformity may occur in patients with lax joints and in patients with conditions such as Ehlers-Danlos syndrome.
- 89. A, Terminal tendon rupture may be associated with synovitis of distal interphalangeal joint, leading to distal interphalangeal joint flexion and subsequent proximal interphalangeal joint hyperextension. Rupture of flexor digitorum superficialis tendon can be caused by infiltrative synovitis, which can lead to decreased volar support of proximal interphalangeal joint and subsequent hyperextension deformity. B, Lateral-band subluxation dorsal to axis of rotation of proximal interphalangeal joint. Contraction of triangular ligament and attenuation of transverse retinacular ligament are depicted.
- 90. Types of swan neck deformities in RA • Type I :- PIP joint flexible, independent of MCP position (i.e. Bunnell's test negative). Due to palmar plate failure at PIP joint ± failure of FDS • Type II :- PIP joint flexibility dependent on MCP position. Intrinsic muscle tightness. Bunnell's test: with MCP joint passively extended, passive PIP joint flexion limited • Type III:- PIP joint stiff regardless of MCP position. Due to contracture of joint • Type IV :- Destruction of PIP joint -
- 91. Tt. Swan neck deformity • Type I require dermodesis, flexor tenodesis of the proximal interphalangeal joint, fusion of the distal interphalangeal joint, and reconstruction of the retinacular ligament. • Type II require intrinsic release in addition to one or more of the aforementioned procedures. • Type III require joint manipulation, mobilization of the lateral bands, and dorsal skin release. • Type IV arthrodesis of the proximal interphalangeal joint or, in the ring and small fingers, with Swanson implant arthroplasty of the proximal interphalangeal joint.
- 92. Buttonhole, or Boutonnière, Deformity • flexed proximal interphalangeal joint, with a hyperextended distal interphalangeal joint • it is thought to be caused by synovitis of the proximal interphalangeal joint with a stretching out of the central slip, forcing the lateral bands to begin subluxating volarward.
- 94. • As the deformity progresses, the lateral bands are forced farther over the condyles of the proximal interphalangeal joint and become tightened by their new course and by pressure from the underlying swollen joint. • They finally become fixed in a subluxated position volar to the transverse axis of the joint and act as flexors of the proximal interphalangeal joint. • This tightening causes a secondary hyperextension deformity of the distal interphalangeal joint. The flexion deformity of the proximal interphalangeal joint is compensated for by an extension of the metacarpophalangeal joint. The metacarpophalangeal joint deformity does not become fixed, as do the distal two joints.
- 95. Clinically • In mild buttonhole deformities,The flexion deformity at the proximal interphalangeal joint is passively correctable from a position of approximately 15 degrees of flexion. (normal-appearing radiographs) In these deformities, treatment may consist of releasing the lateral tendons near their insertion into the distal phalanx. • A moderate buttonhole deformity has an approximately 40-degree flexion contracture of the proximal interphalangeal joint, most of which is passively correctable.. (satisfactory preservation of joint space radiographcally) To correct this deformity, there must be functional restoration of the central slip and correction of the subluxation of the lateral bands. • A fixed buttonhole deformity passively uncorrectable flexion contracture of the proximal interphalangeal joint. Combined procedures on both joints, usually metacarpophalangeal joint arthroplasty or fusion with interphalangeal joint release or fusion, are necessary.
- 96. • Boutonnière deformity. A, Primary synovitis of proximal interphalangeal (PIP) joint can lead to attenuation of overlying central slip and dorsal capsule and increased flexion at PIP joint. Lateral band subluxation volar to axis of rotation of PIP joint can lead in time to hyperextension. Contraction of oblique retinacular ligament, which originates from flexor sheath and inserts into dorsal base of distal phalanx, can lead to extension contracture of distal interphalangeal joint. • B, Clinical photograph illustrates flexion posture of PIP joint and hyperextension posture of distal interphalangeal joint in boutonnière deformity.
- 97. Swanson technique • A, Swan-neck deformity of fingers. B, Central tendon is separated from lateral tendons by dividing connecting fibers. Central tendon is step-cut transversely and dissected proximally, lengthening it. C, Lateral tendons relocate palmarward. After insertion of implant, cut ends of central tendon are approximated with interrupted sutures. Knots are buried.
- 98. • A, Buttonhole deformity of index finger with swan-neck deformity of other fingers. B and C, Lengthened central tendon is advanced, and lateral tendons are released and relocated dorsally by suturing their connecting fibers
- 99. X-rays • Early stage :- soft-tissue swelling and osteoporosis around the joints. • Later :- Joint space narrowing and small peri- articular erosions; these are commonest at the MCP joints and in the styloid process of the ulna. • In advanced cases, articular destruction may be marked, affecting the MCP, PIP and wrist joints almost equally.
- 100. Treatment • EARLY STAGE DISEASE :- is directed essentially at controlling the systemic disease and the local svnovitis. • In addition to general measures, static splints may reduce pain and swelling. • These splints are not corrective but are designed to rest inflamed joints and tendons; in mild cases they are worn only at night, in more active cases during the day as well. • Persistent synovitis of a few joints or tendon sheaths may benefit from local injections of corticosteroid with local anaesthetic
- 101. Established disease • If disease progressesprevent deformity. • Uncontrolled synovitis of joints or tendons requires operative svnovectomy followed by physiotherapy.
- 102. • Excision of the distal end of the ulna, synovectomy of the common ex- tensor sheath and the wrist, and reconstruction of the soft tissues on the ulnar side of the wrist may arrest joint destruction and progressive deformity. • Early instability and ulnar drift at the MCP joints can be corrected by excising the inflamed synovium, tightening the capsular structures and releasing the ulnar pull of the intrinsic tendons. • Mobile boutonniere and swan-neck deformities can be treated with splints; if they progress or are fixed, then surgery may be needed. Isolated tendon ruptures are repaired or bypassed by appropriate tendon transfers. These procedures are followed by splin tage and hand therapy. • Destruction of the MCP joints without ulnar drift can be treated with surface replacement (chromepolyethylene or pyrocarbon)
- 103. Late disease There is Deformity + articular destruction so soft-tissue correction alone will not suffice. For the MCP and IP joints of the thumb arthrodesis gives predictable pain relief, stability functional improvement. The MCP joints of thefinger can be excised and replaced with Silastic spacerswhich improve stability and correct deformity Replacement of IP joints gives less predictable results if deformity is very disabling (e.g. a fixed swan-neck it may be better to settle for arthrodesis in a in functional position.
- 104. • At the wrist, painless stability be regained by fusion of the radio-carpal, midcarpal and CMC joints. • Wrist replacement with Silastic metal-plastic implants may fail; due to the loss of bone stock that accompanies failure means that salvage can be very difficult.
- 105. • Souter recommended starting with a procedure that is likely to succeed, beginning with the least involved hand. He grouped hand procedures from the most effective (group I) to the least effective (group V). In addition, Souter advocated correcting significant disease and deformity in the elbow and shoulder before correcting hand deformities.
- 107. The thumb in rheumatoid arthritis • The combination of soft-tissue failure and joint erosion leads to characteristic deformities of the thumb: – rupture of flexor pollicis longus tendon, – a boutonniere lesion at the MCP joint, – CMC instability swan- neck deformity – Ulnar collateral ligament instability. • Depending on the deformity, the patient's demands and the condition of the rest of the hand, treatment may involve various combinations of splintage, tendon repair, joint fusion, excision arthroplasty and joint replacement.
- 108. RH THUMB • Pain free thumb with stability and mobility is very imp. • All three trapezio-metacarpal, MCP and IP joints may be involved. • Deformity of wrist affects more distal part, so if Tr-Mc joint deformity compensatory deformity at MCP and IP joints and MCP disease leads to IP deformity. • Thus most proximal affected joint must be addressed first.
- 109. • synovitis beginning in the thumb MCP joint frequently leads to a boutonnière deformity of the thumb, with palmar subluxation and flexion of the proximal phalanx with hyperextension of the interphalangeal joint. • When synovitis begins in the thumb carpometacarpal joint, the deformity includes dorsal subluxation of the metacarpal base and hyperextension of the metacarpophalangeal joint (swan-neck deformity).
- 110. • Another thumb deformity caused by synovitic destruction of the capsuloligamentous supports on the ulnar side of the metacarpophalangeal joint is the gamekeeper thumb, which results from laxity of the ulnar collateral ligament of the thumb at the metacarpophalangeal joint. • Involvement of the metacarpophalangeal joint also can result in laxity of the capsuloligamentous structures in the volar plate, leading to hyperextension of the metacarpophalangeal joint and interphalangeal hyperflexion, but with a stable carpometacarpal joint. Other, more severe deformities of the fingers and thumb can be caused by an erosive rheumatoid disease, leading to the “main en lorgnette” (opera glass hand).
- 113. Rh thumbs-types • By Nalebuff into 5 types • Type I- MCP flexion def with sec compensatory IP hyperextension (due to synovitis at MCP joints which causes attenuation of the EPB tenson and extensor hood , leading to extensor lag at MCP joints. The EPL tendon subluxates in an ulnar and volar direction functioning as an MCP flexor and IP extesnor.
- 114. • Type II- Primary TMJ d’s with Sec. IP joint hyperextension and instability. Tt- TMJ must be reconstructed followed by IP arthrodesis.
- 115. • Type III- Second most common deformity. • Primary TMJ instability followed by compensatory hyperextension deformity at MCP joints. • Synovitis of the TMJ leads to laxity of the palmar oblique ligament with dorsoradial suluxation of the metacarpal base. • Combined forces of APL and Adductor pollicis lead to adduction of first metacarpal and narrowing of first web space.
- 116. • Hyperextension deformity at the MCP joint develops due to the first metacarpal adduction contracture. • As patient attempt to extend the thumb and grasp objects, extension force is transmitted to MCP joint instead of the metacarpal which is fixed. Progressive volar plate laxity develops, leading to a MCP hyperextension deformity.
- 117. • Treatment :- • Aimed primarily at TMJ • Arthroplasty+ ligament stabilization procedures like ligament reconstruction combined with a silicone , fascial or tendon interposition arthroplasty. • Adduction contracture bone resection +/- web space z plasty for abduction.
- 118. • Indication for MCP fusion at the time of TMJ arthroplasty include either 20 degree of passive hyperextension or 30 degree of valgus instability. • If the MCP joint is only mildly unstable, volar tenodesis or capsuplasty instead of fusion.
- 119. • Type IV- Same as type III, except that the MCP joint develops valgus instability. • Type V- not original, added later • Volar plate laxity at MCP joint and IP joint flexion deformity. Primary pathology at MCP joint • Tt- Mcp joint capsulodesis or fusion.
- 120. • Thumb IP arthrodesis- 0-10 deg flex, neutral abd-add, 5 deg pronation. • MCP- 15 deg flex, 15 deg abd, and 15 deg of pronation.
- 121. Management of thumb deformities • 1. Ruptured FPL – If painless: leave alone – If painful: tendon graft, flexor digitorum sublimus transfer or IP fusion • 2. Simple boutonniere deformity – If passively correctible: cortisone injection to MCP joint and splintage – MCP joint synovectomy and extensor realignment unreliable – If MCP joint fixed but IP joint passively correctible and CMC joint mobile: fuse MCP joint – If MCP joint and IP joint fixed: fuse IP joint and either fuse or replace MCP joint • 3. Boutonniere with CMC joint failure – Trapeziectomy and CMC joint stabilization, with MCP joint and IP joint treated as above
- 122. 4. Swan-neck deformity - CMC joint failure causes adduction contracture of thumb base and MCP joint hyperextension - If deformity severe: trapeziectomy with soft-tissue reconstruction or fusion of MCP joint 5. Failure of ulnar collateral ligament (like 'gamekeeper's thumb) Synovitis attenuates ulnar collateral ligament. Pinch grip causes increasing deformity Ligament reconstruction (if bone and soft-tissue quality allow) or MCP joint fusion 6. Swan-neck with MCP joint and CMC joint preserved Synovitis of MCP joint causes hyperextension v, secondary passive flexion of IP joint – Treat by palmar plate advancement or, if soft tissues tenuous, MCP fusion 7. Arthritis mutilans – Arthrodesis with interposition bone graft
- 123. RA-MCP JOINTS
- 124. Metacarpo-phalangeal deformities • Chronic synovitis of the MCP joints results in failure of the palmar plate and the collateral ligaments. • The powerful flexor tendons drag the proximal phalanx palmarwards, causing subluxation of the joint. • The deformity may be aggravated by primary or secondary intrinsic muscle tightness
- 125. • Most obvious deformity :- ulnar deviation of the MCP joints. • Reasons for this: palmar grip and thumb pressure naturally tend to push the index finger ulnarwards; weakening of the collateral ligaments and the first dorsal interosseous muscle reduces the normal resistance to this force; the wrist is usually involved and, as it collapses into radial deviation, the MCP joints automatically veer in the opposite direction (the ,so-called zig zag mechanism).
- 126. Treatment RA-MCP • Early stage before joint destruction and soft-tissue instabilitysynovectomy • When ulnar drift has started splintage • With marked deformity but little joint damage a soft-tissue reconstruction (reefing of the radial sagittal bands, tightening of the radial collateral ligament with intrinsic muscle release and transfer) • If marked damage to the joint surface, replacement with a Silastic spacer, along with the soft-tissue reconstruction, is recommended. • There is no point in correcting the MCP joints unless any wrist deformity is also corrected; the tendency to zig-zag deformity will otherwise lead to recurrence of the ulnar drift.
- 127. Tenosynovitis and tendon rupture • Extensor tendons :- Extensor tendon rupture is a common complication of chronic svnovitis. • Tenosynovitis presents with mass over dorsum of the hand with pain and limited motion. • Extensor digiti minimi is usually the first to go and predicts rupture of the other tendons.
- 128. • The extrinsic extensor tendons are the primary extensors of the MCP joints, whereas the intrinsics are the primary extensors of the interphalangeal joints. • As a result, extrinsic extensor tendon ruptures only lead to a lag at the MCP joint level.
- 129. • The extensor pollicis tendon is a common tendon rupture in the rheumatoid patient because of tension and friction as the tendon passes around Lister's tubercle. • Rupture of the EPL does not lead to a complete lack of extension at the IP joint because of the attachments of the APB and adductor pollicis (ADD) tendons to the dorsal expansion. • Instead, EPL rupture is best diagnosed by the inability of the patient to extend the thumb while the hand is held flat on a table, palm side down.
- 130. • Rupture of a single EDC tendon is treated by side-to-side repair to an adjacent EDC tendon. • Similarly, isolated EDQ rupture is treated by side- to-side repair to EDC. • Rupture of both EDQ and EDC to small is best treated by EIP transfer to both tendon stumps. • Rupture of EDC to ring and small is usually treated by side-to-side transfer of EDC long to EDC ring and transfer of EIP to EDC small. • Rupture of EDC of long, ring, and small can be treated by side-to- side transfer of EDC long to EDC index, and EIP to EDC ring and EDC small.
- 131. • It can also be treated by EIP to EDC long and FDS ring to EDC ring and small. • Rupture of all of the extrinsic finger extensors (II-V) is usually repaired using FDS tendons. FDS long is transferred to EDC index and FDS ring is transferred to EDC long, ring, and small. • The tension of the tendon transfers is critical for optimal function. The tendon transfer for finger extension is set with the wrist in maximal extension and the fingers in full flexion. This ensures that the transfer will not be too tight and thereby limit finger
- 132. • In those with a wrist fusion, the tendon transfer is set with the interphalangeal joints in full extension and the MCP joints flexed 25- 30°.
- 133. Flexor tendons • Flexor tendons :- Flexor tenosvnovitis one of the earliest features. • FPL and profundus to small finger is commonest to rupture • The restriction of finger movement is easily mistaken for arthritis; however, careful palpation of the palm and the nearby joints will quickly show where the swelling and tenderness are located. • Secondary problems include carpal tunnel syndrome, triggering of one or more fingers and tendon rupture Synovitis of the flexor digitorum superficialis also con- tributes to the swan-neck deformity
- 134. • If carpal tunnel release is needed, the operation should include a flexor tenosvnovectomy. • If the flexor tendons are bulky (best felt over the proximal phalanges) and joint movement is limited, then flexor tenosynovectomv should improve movement and, just as important, should prevent tendon rupture. • Triggering, likewise, should be treated by tenosynovectomy rather than simple splitting of the sheath.
- 135. • Rupture of flexor digitorum profundus is best treated by distal IP joint fusion. • Rupture of flexor pollicis longus (due to attrition against the underside of distal radius or flexor svnovitis) can be treated eitherby tendon grafting or by fusion of the thumb IP joint.
- 136. • Surgical synectomy only after 6 months- if conservative management fails. • Primary repair is generally not possible for flexor tendon injuries in these patients. Instead if rupture occurs at level of the palm, it is repaired side to side fashion to an intact flexor tendon. • If the rupture occurs at a digital level , then the superficialis tendon from another finger is used as a transfer.
- 137. To Summarize….. • General principles of orthopaedic care in RA are:- • 1. Maintaining position and function of all joints by physiotherapy and splintage. • 2. Treating the soft tissue and joint processes as they develop by injections, by principles of rest and, where necessary by early surgery. • 3. Correcting established deformity and attempting to restore function- but this does not mean the severely deformed ‘burned out’ rheumatoid hand in which there is little motor power left.
- 141. RA Vs. OA Rheumatoid arthritis Osteoarthritis • It is an autoimmune disease and often strikes • It is an age-related disease due to wear and in the prime of life. tear of the cartilage. • It is usually seen between the ages of 25 and • It usually affects people after 40 years of age. 50 years of age but can also occur in children and infancy. • It affects joints on both sides of the body and • It usually affects isolated joints, or joints on has a only one side of the body at first. bilateral presentation. • It causes redness, warmth and swelling of • It usually does not cause redness and the joints. warmth of the joints. • It affects many joints usually small joints of • It most commonly affects weightbearing the hands joints or joints that are overused (e.g. knees and feet, and may affect the elbow, shoulders, and hip). wrist, hip, knee and ankles. • It can affect the entire system, with general • Discomfort is usually related to the affected feeling of joint. sickness and fatigue, as well as weight loss. • There is history of prolonged morning • Brief morning stiffness. stiffness.
- 143. • Rheumatoid arthritis (RA) • Features • Mnemonic: RHEUMATISM • R Rheumatoid factor (RF) +ve in 80%/Radial deviation of wrist • H HLA-DR1 and DR-4 • E ESR/Extra-articular features (restrictive lung disease, subcutaneous nodules) • U Ulnar deviation of fingers • M Morning stiffness/MCP+PIP joint swelling • A Ankylosis/Atlanto–axial joint subluxation/Autoimmune/ANA +ve in 30%T T-cells (CD4)/TNF • I Inflammatory synovial tissue (pannus)/IL-1 • S Swan-neck deformity, Boutonniere deformity, Z-deformity of thumb • M Muscle wastage of small muscles of hand
- 144. • Management • DMARDs (Disease-Modifying Anti-Rheumatic Drugs) • Mnemonic: Most Sufferers Can Get Appropriate Pain Control • M Methotrexate • S Sulfasalazine • C Ciclosporin • G Gold • A Azathioprine • P Penicillamine • C HydroxyChloroquine