Infectious disease p5
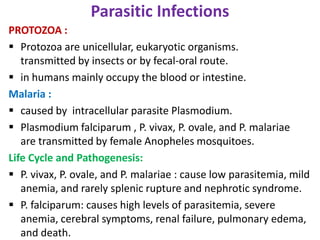
- 1. Parasitic Infections PROTOZOA : Protozoa are unicellular, eukaryotic organisms. transmitted by insects or by fecal-oral route. in humans mainly occupy the blood or intestine. Malaria : caused by intracellular parasite Plasmodium. Plasmodium falciparum , P. vivax, P. ovale, and P. malariae are transmitted by female Anopheles mosquitoes. Life Cycle and Pathogenesis: P. vivax, P. ovale, and P. malariae : cause low parasitemia, mild anemia, and rarely splenic rupture and nephrotic syndrome. P. falciparum: causes high levels of parasitemia, severe anemia, cerebral symptoms, renal failure, pulmonary edema, and death.
- 2. The infectious stage of malaria, the sporozoites, is found in salivary glands of female mosquitoes. When mosquito takes a blood meal, sporozoites are released into human's blood and within minutes attach to and invade liver cells by binding to hepatocyte receptors for serum proteins thrombospondin and properdin. Within liver cells, malaria parasites multiply rapidly, so merozoites (asexual haploid forms) are released when each infected hepatocyte ruptures. Once released from liver, merozoites bind by a parasite lectin-like molecule to sialic residues on glycophorin molecules on surface of red blood cells.
- 3. Within red blood cells, the parasites grow in a membrane-bound digestive vacuole, hydrolyzing hemoglobin through secreted enzymes. The trophozoite is first stage of parasite in red blood cell and is defined by presence of a single chromatin mass. The next stage, the schizont, has multiple chromatin masses, each of which develops into a merozoite. On lysis of red blood cell, the new merozoites infect additional red blood cells. Although most malaria parasites within red blood cells develop into merozoites, some parasites develop into sexual forms called gametocytes that infect the mosquito when it takes its blood meal.
- 4. Morphology: Initially congestion and enlargement of spleen, and there is increased phagocytic activity of macrophages in spleen. In chronic malaria infection, the spleen becomes increasingly fibrotic and brittle, with thick capsule and fibrous trabeculae. the liver becomes progressively enlarged and pigmented. Kupffer cells are heavily laden with malarial pigment, parasites, and cellular debris. Pigmented phagocytic cells may be found in bone marrow, lymph nodes, subcutaneous tissues, and lungs. In malignant cerebral malaria caused by P. falciparum, brain vessels are plugged with parasitized red cells . About the vessels, there are ring hemorrhages that are probably related to local hypoxia.
- 5. [MALARIAL PARASITES IN BLOOD]. Note the presence of two chromatin dots in each trophozoite inside red blood cells. Note also the two trophozoites in another red blood cell. The presence of two chromatin dots and two trophozoites is a feature of P. falciparum.
- 6. Leishmaniasis: Leishmaniasis is a chronic inflammatory disease of skin, mucous membranes, or viscera. caused by obligate intracellular kinetoplastid protozoan parasites transmitted through the bite of infected sandflies Pathogenesis: The life cycle of Leishmania involves two forms: the promastigote, which develops and lives extracellularly in sandfly vector. the amastigote, which multiplies intracellularly in host macrophages. Mammals, including rodents, dogs, and foxes, are reservoirs of Leishmania.
- 7. The promastigotes are phagocytosed by macrophages, and acidity within phagolysosome induces them to transform into round amastigotes that lack flagella but contain a single DNA-containing specialized mitochondrion called kinetoplast. Amastigotes proliferate within macrophages, and dying macrophages release progeny amastigotes which can infect additional macrophages Morphology: Leishmania species produce four different lesions in humans: visceral, cutaneous, mucocutaneous, and diffuse cutaneous.
- 8. visceral leishmaniasis: caused by L. donovani or L. chagasi. parasites invade macrophages throughout mononuclear phagocyte system and cause hepatosplenomegaly, lymphadenopathy, pancytopenia, fever, and weight loss. Phagocytic cells crowd the bone marrow and also may be found in lungs, gastrointestinal tract, kidneys, pancreas, and testes. there is hyperpigmentation of skin in extremities, that is why the disease is called kala-azar or "black fever" . In kidneys, there may be an immune complex-mediated mesangioproliferative glomerulonephritis. in advanced cases, there may be amyloid deposition.
- 9. A bone marrow aspirate shows intracellular and extracellular amastigotes (A), the form of the leishmania organism that lacks an exteriorized flagellum. The kinetoplast is an independently replicating organelle in the mitochondrion of the organism. AN denotes
- 10. Cutaneous leishmaniasis: caused by L. major, L. mexicana, and L. braziliensis. The lesion (often called tropical sore) begins as itching papule surrounded by induration. changes into a shallow ulcer with irregular borders, and usually heals by involution within 6 months without treatment. On microscopic examination, the lesion is granulomatous, usually with many giant cells and few parasites.
- 11. . Histology of cutaneous leishmaniasis (H&E stain): a) Diffuse chronic inflammatory cell infiltrate in dermis with multiple non-caseating granulomata (×40); b) Tuberculoid-type granuloma with central histiocytes and peripheral inflammatory cells (×100); c) Leishman- Donovan bodies (arrows) within cytoplasm of epithelioid histiocytes (×600); d) Langhans type giant cells (arrows) within a granuloma (×600).
- 12. Mucocutaneous leishmaniasis: caused by L. braziliensis. Moist, ulcerating or nonulcerating lesions, develop in larynx and at mucocutaneous junctions of nasal septum, anus, or vulva. On microscopic examination, there is mixed inflammatory infiltrate with parasite-containing histiocytes in association with lymphocytes and plasma cells. Later, the tissue reaction becomes granulomatous, and the number of parasites declines. Eventually, the lesions remit and scar, although reactivation may occur after long intervals.
- 13. Diffuse cutaneous leishmaniasis : is a rare form of dermal infection. begins as a single skin nodule, which continues spreading until the entire body is covered by bizarre nodular lesions, which resemble keloids or large verrucae. The lesions do not ulcerate but contain vast aggregates of foamy macrophages stuffed with leishmania.
- 14. METAZOA : are multicellular, eukaryotic organisms. are contracted by eating the parasite, often in undercooked meat, and by direct invasion of host through skin and through insect bites. They dwell in many sites of body, including intestine, skin, lung, liver, muscle, blood vessels, and lymphatics Tapeworms (Cestodes): Taenia solium and Echinococcus granulosus are cestode parasites (tapeworms) that cause cysticercosis and hydatid infections, respectively. Both diseases are caused by larvae that develop following ingestion of tapeworm eggs.
- 15. T. solium: tapeworms consist of a head (scolex) that has suckers and hooklets that attach to intestinal wall, and a neck and many flat segments called proglottids that contain male and female reproductive organs. T. solium can be transmitted to humans in two ways: (1) Ingestion of undercooked pork containing larval cysts, called cysticerci, leads to development of adult tapeworms in intestine. (2) When intermediate hosts (pigs or humans) ingest eggs in food or water contaminated with humanfeces. the larvae hatch, penetrate the gut wall, disseminate hematogenously, and encyst in many organs.
- 17. Convulsions, increased intracranial pressure, and neurologic disturbances are caused by T. solium cysts in brain tissue. When cysticerci degenerate, an inflammatory response develops. Taenia saginata (the beef tapeworm), and Diphyllobothrium latum ( the fish tapeworm ). are acquired by eating undercooked meat or fish. In humans, these parasites live only in gut, and they do not form cysticerci .
- 18. Hydatid disease: caused by ingestion of eggs of echinoccal species. Echinococcus granulosus, and Echinoccus multilocularis. Humans are accidental intermediate hosts, infected by ingestion of food contaminated with eggs shed by dogs or foxes. Eggs hatch in duodenum and the larvae invade liver, lungs, or bones. Unilocular cysts caused by E. granulosus . Multilocular cysts are caused by E. multilocularis. Morphology: About two-thirds of human E. granulosus cysts are found in liver, 5% to 15% in lung, and the rest in bones and brain or other organs.
- 19. In various organs, the larvae lodge within capillaries and first incite an inflammatory reaction composed principally of mononuclear leukocytes and eosinophils. Many such larvae are destroyed, but others encyst. The cysts begin at microscopic levels and progressively increase in size, so that in 5 years or more, they may have achieved dimensions of more than 10 cm in diameter. Enclosing opalescent fluid is an inner, nucleated, germinative layer ; and an outer, opaque, nonnucleated layer. The outer nonnucleated layer has delicate laminations made up of many layers of gelatin.
- 20. Outside this layer, there is a host inflammatory reaction that produces a zone of fibroblasts, giant cells, and mononuclear and eosinophilic cells. In time, a dense fibrous capsule forms. When these cysts have been present for about 6 months, daughter cysts develop within them. These appear first as minute projections of germinative layer that develop central vesicles and thus form tiny brood capsules. Scolices of worm develop on inner aspects of these brood capsules
- 21. Histopathology of hydatid cyst.
- 22. Schistosomiasis : caused by Schistosoma mansoni , Schistosoma japonicum, Schistosoma mekongi, and Schistosoma haematobium. Pathogenesis: Infectious schistosome larvae (cercariae) swim through fresh water and penetrate human skin with the aid of powerful proteolytic enzymes that degrade the keratinized layer. Schistosomes migrate into peripheral vasculature, traverse to lung, and settle in portal or pelvic venous system, where they develop into adult male and female schistosomes. Females produce hundreds of eggs per day, around which granulomas and fibrosis form.
- 23. Some schistosome eggs are passed from portal veins through intestinal wall into colonic lumen, are shed with feces, and release into freshwater miracidia that infect snails to complete the life cycle. Morphology: In mild S. mansoni or S. japonicum infections, white, pin head-sized granulomas are scattered throughout gut and liver. At the center of granuloma is schistosome egg, which contains a miracidium; this degenerates over time and calcifies. The granulomas are composed of macrophages, lymphocytes, neutrophils, and eosinophils.
- 24. Histopathology of schistosomiasis haematobia, bladder Histopathology of bladder shows eggs of Schistosoma haematobium surrounded by intense infiltrates of eosinophils.
- 25. The surface of liver is bumpy, whereas cut surfaces reveal granulomas ,and a widespread fibrous portal enlargement without distortion of intervening parenchyma. Because these fibrous triads resemble the stem of a pipe, the lesion is named pipe-stem fibrosis. these portal triads , causing portal hypertension and severe congestive splenomegaly, esophageal varices, and ascites. In S. haematobium infection, bladder inflammatory patches due to massive egg deposition and granulomas appear early, and when they erode, they cause hematuria.
- 26. Later, the granulomas calcify and develop a "sandy" appearance, which, if severe, may line the wall of bladder and cause a dense concentric rim (calcified bladder) on radiographic films. The most frequent complication of S. haematobium infection is inflammation and fibrosis of ureteral walls, leading to obstruction, hydronephrosis, and chronic pyelonephritis. There is also an association between urinary schistosomiasis and squamous cell carcinoma of bladder. Lymphatic Filariasis : transmitted by mosquitoes and caused by nematode Wuchereria bancrofti. filariasis causes a spectrum of diseases: (1) asymptomatic microfilaremia. (2) chronic lymphadenitis with swelling of dependent limb or scrotum (elephantiasis). (3) tropical pulmonary eosinophilia.
- 27. Pathogenesis: Infective larvae released by mosquitoes during blood meal develop within lymphatic channels into adult males and females, which mate and release microfilariae that enter into bloodstream. When mosquitoes bite infected individuals, they can take up the microfilariae and transmit the disease. adult filariae secrete factors that are capable of causing lymphatic dilation, lymphedema, and elephantiasis. In contrast, microfilariae, even in massive numbers are not directly toxic to host.
- 28. adult filariae factors include: (1) surface glycoproteins with antioxidant function. (2) cysteine protease inhibitors, which impair MHC class II antigen-processing pathway; (3) serine protease inhibitors, which inhibit neutrophil proteases (4) homologues of TGF-β, which can bind to TGF-β receptors and downregulate inflammatory responses. In chronic lymphatic filariasis damage to lymphatics is caused directly by adult parasites and by a TH1-mediated immune response, which stimulates formation of granulomas around adult parasites.
- 29. Finally, IgE-mediated hypersensitivity to microfilariae result in tropical pulmonary eosinophilia. IgE and eosinophils may be stimulated by IL-4 and IL-5, respectively secreted by filaria-specific TH2 helper T cells. Tropical pulmonary eosinophilia results in restrictive lung disease. Morphology: Chronic filariasis is characterized by persistent lymphedema of scrotum, penis, vulva, leg, or arm . Frequently, there is hydrocele and lymph node enlargement. In severe and long-lasting infections, chylous weeping of enlarged scrotum may ensue, or a chronically swollen leg may develop.
- 30. Elephantoid skin shows dilation of dermal lymphatics with widespread lymphocytic infiltrates and focal cholesterol deposits. the epidermis is thickened and hyperkeratotic. Adult filarial worms—live, dead, or calcified—are present in scrotal draining lymphatics or nodes, surrounded by (1) mild or no inflammation, (2) intense eosinophilia with hemorrhage and fibrin, or (3) granulomas. Lung involvement by microfilariae is marked by • eosinophilia caused by TH2 responses and cytokine production (tropical eosinophilia); or by • dead microfilariae surrounded by stellate, hyaline, eosinophilic precipitates embedded in small epithelioid granulomas (Meyers-Kouvenaar bodies).
- 31. Lymphatic filariasis (LF) is caused by filarial nematodes Wuchereria bancrofti, Cross-sectional view of a filarial nematode in spermatic cord, with surrounding intense eosinophilic inflammatory infiltrate . U = uterine tubes. M = musculature. I = intestine. C = cuticle.
- 32. THANK YOU
