Blounts disease
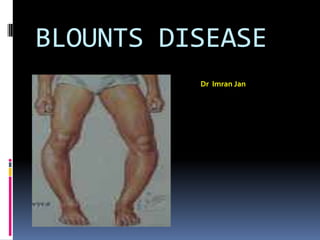
- 1. BLOUNTS DISEASE Dr Imran Jan
- 2. Definition It is an disorder of the proximal medial tibial growth plate causes progressive varus alignment of the knees (bowed legs) in children or adolescents .
- 3. synonyms Infantile tibia vara Erlacher`s disease Blount-barber disease Subepipyseal osteochondropathy Non rachitic bow legs Ostetis deformans tibia
- 5. BLOUNTS DISEASE Erlacher first description of tibia vara and internal tibial torsion (1922) Blount (1937) described tibia vara as “an osteochondrosis similar to coxa plana and Madelung's deformity but located at the medial side of the proximal tibial epiphysis.” .
- 6. Prevalence <1% of all bow legs The infantile form is more common in girls. The juvenile or adolescent form is more common in boys. The disorder is more common in African American children than those of other races.
- 7. ETIOLOGY Current concept is tibia vara is An acquired disease of the proximal tibial metaphysis of unknown cause Enchondral ossification seems to be altered.
- 8. Suggested causative factors include infection trauma osteonecrosis latent form of rickets although none of these has been proved A combination of hereditary and developmental factors is the most likely cause
- 9. The relationship of early walking and obesity to Blount disease has been clearly documented. Rarely seen in non ambulant children
- 10. BLOUNTS DISEASE COMPONENTS OF DEFORMITY Varus Internal torsion of tibia Recurvatum LLD Femoaral varus late MSC hypertrophy
- 11. PATHOLOGY islands of densely packed chondrocytes with hypertr0phy areas of almost acellular cartilage Intraphyseal ossification centers abnormal groups of capillaries. Extension of noncalcified cartilaginous bars into the proximal epiphysis and distal metaphyses
- 12. CLASSIFICATON Infantile: before 8 years of age bilateral in 60% Adolescent more than 8Yrs till skeletal fusion 1 with a cause 2 obese , black
- 13. Clinical features Bowing of legs - progressive Metaphyseal spike Knee pain +/-
- 14. Radiology medial half of the epiphysis as seen on radiographs is short, thin, and wedged the physis is irregular in contour and slopes medially. The proximal metaphysis forms a projection medially . According to Smith, however, medial metaphyseal fragmentation is pathognomonic for the development of a progressive tibia vara.
- 17. Tibio Femoral Angle Metaphysio Diaphysial angle (Levin and Drennen) MD angle
- 18. MDA ANGLE MDA < 11: normal physiologic bowing MDA 11-15: equivocal MDA >15: Blount’s
- 19. Langenskiold classification (1952) I - irregular metaphyseal ossification combined with medial and distal protrusion of the metaphysis II, III, IV - evolves from a mild depression of the medial metaphysis to a step-off of the medial metaphysis V - increased slope of medial articular surface and a cleft separating the medial and lateral epicondyle VI - bony bridge across the physis Depending on degree of metaphysial and epiphysial changes on radiograph – 6 progressive stages with increasing age
- 20. Work up findings No specific blood marker Tests to R/o Infection and Rickects CT scan in 5yrs + to detect physeal bar
- 21. Differential Diagnosis Physiologic genu varum Skeletal dysplasias (Metaphysial chondrodysplasia, SED, MED, Achondroplasia) Metabolic diseases (Renal OD,Vit D resistant rickets) Post-traumatic deformity Post-infective sequelae Proximal focal fibrocartilaginous dysplasia
- 22. Treatment Treatment choices and prognosis depend greatly on the age of the patient and radiographic stage at the time of diagnosis
- 23. Rx - Orthotics Recommended for patients < 3 years of age and < stage II disease Rainey et al recommended LOCKED KAFO that produced a valgus force by three point pressure 23 HRS /DAY Full weight bearing Risk for failure included ligamentous instability, patient weight above 90th percentile and late initiation of bracing
- 24. Corrective osteotomy options Metaphyseal Epiphyseal – metaphyseal Intra epiphyseal Fibula &Bony bar resection
- 25. Rx – Corrective Osteotomy… Rab proximal tibial oblique metaphyseal osteotomy in which single plane oblique cut allows simultaneous correction of varus and internal rotation and permits postoperative cast wedging if necessary to obtain appropriate position.
- 27. RAB’S OBLIQUE PROX. TIBIAL OSTEOTOMY
- 28. Rx – Corrective Osteotomy… Greene Chevron open- closing wedge osteotomy in which opening and closing wedges can be made so that the limb length deformity present in moderate to severe tibia vara will not be increased. He prefers a crescent shaped osteotomy using one half lateral closing wedge and using the graft medially in an opening wedge to maintain length.
- 29. GREEN CHEVRON
- 30. Rx – Corrective Osteotomy… In children older than 9 years with more severe involvement, osteotomy alone, with bony bar resection, or with epiphysiodesis of the lateral tibial and fibular physes may be indicated For older children in whom bracing and tibial osteotomy have failed to prevent progressive deformity, Ingram, Siffert and others have suggested an intraepiphyseal osteotomy to correct severe joint instability and a valgus metaphysial osteotomy to correct the varus angulation
- 31. Rx – Corrective Osteotomy… Schoenecker et al – elevation of medial tibial plateau with metaphysial wedge osteotomy Gregosiewics – double elevating osteotomies; intraepiphyseal and metaphyseal Zayer – hemicondylar tibial osteotomy through the epiphysis into the tibial intercondylar notch Bell, Coogan – recommended Ilizarov’s technique Uniplanar external fixator for isolated frontal one plane deformity
- 32. SIFFERT’S I E OSTEOTOMY
- 34. Rx in a nut shell AGE STAGE Rx < 2 1-11 observation 2-3 1-11 Modified locked KAFO 3-8 11-111 Oblique / chevron o-y 9 + 1v + Resection of bony / physeal bar +osteotomy+ epiphyseal elevaton +/-lateral tibial epiphyseodesis
- 35. COMPLICATIONS Common peroneal nerve palsy Compartment syndrome Anterior tibial artery occlusion Recurrence
- 36. Not yet over
- 37. CONGENITAL METATARSUS ADDUCTUS Definition Metatarsus adductus is a congenital foot deformity consists of adduction of the forefoot in relation to the midfoot and hindfoot presenting as in-toeing in children.
- 39. Transverse crease along medial border of foot Widening of 1st web space
- 41. CONGENITAL METATARSUS ADDUCTUS It can occur as an isolated anomaly or in association with clubfoot. Among individuals with metatarsus adductus, 1% to 5% also have developmental dysplasia of the hip or acetabular dysplasia
- 42. Metatarsus adductus may be seen as a residual deformity in patients previously treated surgically or nonsurgically for congenital clubfoot. This residual metatarsus adductus can be rigid, indicating fixed positioning of the forefoot on the midfoot and hindfoot, or it can be dynamic, caused by imbalance of the anterior tibial tendon during gait.
- 43. CONGENITAL METATARSUS ADDUCTUS BLECK classified as mild moderate severe In the mild form, the forefoot can be clinically abducted to the midline of the foot and beyond The moderate form has enough flexibility to allow abduction of the forefoot to the midline only In rigid metatarsus adductus, the forefoot cannot be abducted at all.
- 46. Treatment MILD mild deformities resolve Reassurance Observation Serial stretching and casting can be tried
- 47. MODERATE - SEVEREtype Serial stretching and casting for 2-3 months
- 48. Rx SURGICAL INDICATIONS severe deformity uncorrected by conservative treatment pain Objectionable appearance Difficulty in fitting shoes
- 49. SURGICAL OPTIONS Less 4 yrs of age Tarsometatarsal capsulotomies (Heyman, Herndon, and Strong) Beyond 4 yrs of age Multiple metatarsal osteotomies (Berman and Gartland) Medial cuneiform, lateral cuboid double osteotomy
- 51. DOUBLE OSTEOTOMY
- 55. CCV foot Ccv presents Marked dorsiflexion at ankle Hind foot valgus Dorsum of foot against anterior surface of distal leg Ankle ROM till neutral or lessat birth with a dramatic
- 56. CCV foot - causes Uterine packing Oligohyraminos Primipara Twin/triplets
- 57. Ccv Foot Rx Spontaneous recovery with 2-3 months Stretching advisable Serial casting +/- Allay parental anxiety
- 58. THANK YOU
