Periapical Diseases Classification Guide
- 1. PRESENTED BY- ABHISHEK VERMA FINAL YEAR PCDS & RC, BHOPAL PERIAPICAL DISEASES AND CLASSIFICATION
- 2. CONTENTS • Introduction • Causes of the periapical diseases • Classification of the periapical disease • Symptomatic apical periodontitis • Phoenix abscess • Asymptomatic apical periodontitis • Chronic alveolar abscess • Radicular cyst • Condensing osteitis • External root resorption
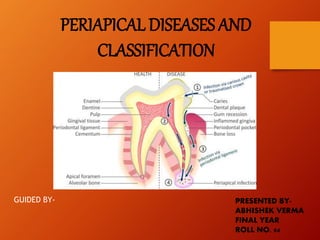
- 3. INTRODUCTION • Pulpal diseases is only one of the several possible causes of diseases of the Periradicular tissues. • Because of the inter-relationship between the pulp and the Periradicular tissues, pulpal inflammation causes inflammatory changes in the periodontal ligament even before the pulp becomes totally necrotic.
- 5. PATHWAYS OF SPREAD OF INFECTIONS
- 6. CAUSES • Bacteria and their toxins, immunologic agents, tissue debris, and products of tissue necrosis from the pulp reach the Periradicular area through the various foramina of the root canals and give rise to inflammatory and immunologic reactions. • Neoplastic disorders, periodontal conditions, developmental factors, and trauma can also cause Periradicular diseases.
- 7. CLASSIFICATION A. SYMPTOMATIC PERIRADICULAR DISEASES (a) Symptomatic apical periodontitis (previously known as acute apical periodontitis) i. Vital tooth ii. Non vital tooth (b) Acute alveolar abcess (c) Acute exacerbation of asymptomatic apical periodontitis (phoenix abscess) B. ASYMPTOMATIC PERIRADICULAR DISEASES (a) Asymptomatic apical periodontitis(previously known as chronic apical periodontitis) i. Chronic alveolar abscess ii. Cystic apical periodontitis (b) Persistent apical periodontitis
- 8. C. CONDENSING OSTEITIS D. EXTERNAL ROOT RESORPTION E. DISEASES OF THE PERIRADICULAR TISSUES OF NON ENDODONTIC ORIGIN
- 9. SYMPTOMATICPERIRADICULAR DISEASES SYMPTOMATIC APICAL PERIODONTITIS Symptomatic apical periodontitis is a painful inflammation of the periodontium as a result of trauma, irritation, or infection through the root canal, regardless of whether the pulp is vital or non vital, producing clinical symptoms including painful response to biting and percussion.
- 10. CAUSES • In a vital tooth- Abnormal occlusal contacts Recently inserted restoration extending beyond the occlusal plane Wedging of a foreign object between the teeth, such as a toothpick or food Traumatic blow to the teeth • In a non vital tooth- Sequelae of pulpal diseases Iatrogenic
- 11. • Root canal instrumentation • Forcing of irritating irrigants or medicaments through the apical foramen • Extension of obturating material through the apical foramen to impinge on Periradicular tissues • Perforation of the root • Over instrumentation during shaping and cleaning of root canals
- 12. SYMPTOMS • Pain and tenderness of the tooth • Tooth may be slightly sore, sometimes only when it is percussed in a certain direction, or the soreness may be severe. • The tooth may feel extruded and the patient may have pain on closure and mastication.
- 13. DIAGNOSIS • Pain on percussion or slight pressure • Overlying mucosa may or not be tender to percussion • Radiographic changes Non vital tooth-slight widening of apical periodontal space and loss of apical lamina dura of involved pulpless tooth Vital tooth-no radiographic changes with normal periradicular structures
- 14. Radiographic features of symptomatic apical periodontitis. “High” amalgam restoration was placed on the occlusal surface of a second mandibular molar. The periodontal ligament space is widened at the apex
- 15. DIFFERENTIAL DIAGNOSIS • Acute alveolar abscess TREATMENT • Determining the cause and relieving the symptoms • Adjustment of high points in hyper-occlusion cases • Removal of irritants in case of non vital infected pulp • When the acute phase has subsided, the tooth is treated by conservative means
- 16. ACUTE ALVEOLAR ABSCESS (ACUTE ABSCESS/ACUTE APICAL ABSCESS/ACUTE DENTOALVEOLAR ABSCESS/ACUTE PERIAPICAL ABSCESS/ACUTE RADICULAR ABSCESS) An acute alveolar abscess is an inflammatory reaction to pulpal infection and necrosis characterised by rapid onset, spontaneous pain, tenderness of the tooth to pressure, pus formation, and eventual swelling of associated tissues.
- 17. CAUSES • Bacterial invasion of dead pulp tissue • Trauma • Chemical or mechanical irritation SYMPTOMS • Tenderness of the tooth that may be relieved by continued slight pressure on the extruded tooth to push it back into the alveolus. • Later, the patient has severe, throbbing pain, with attendant swelling of the overlying soft tissue. • Tooth becomes more painful, elongated and mobile.
- 18. • At times, the pain may subside or cease entirely while the adjacent tissue continues to swell. • If left unattended, the infection may progress to chronic apical abscess wherein the contained pus may break through to form a sinus tract, usually opening in the labial or buccal mucosa. • Patient may appear pale, irritable, & weakened from pain and loss of sleep, as well as from absorption of septic products.
- 19. • Patients in mild cases may only have a slight rise in temperature whereas those in severe cases may reach several degrees above normal. • Intestinal stasis may occur, manifesting itself orally by a coated tongue and foul breath. • Patient may complain of headache and malaise.
- 20. DIAGNOSIS • Clinical examination. • Presence of diffuse & annoying pain. • Extrusion of the tooth. • Radiographically, a cavity, a defective restoration, or slight widening of the apical PDL space. • Diagnosis is confirmed by means of electric pulp and thermal testing. • The affected pulp is necrotic and does not respond to electric current or application of cold. • The tooth may be tender to percussion, or the patient may state that it hurts to chew.
- 21. Intraoral labial sinus opening in relation to the carious maxillary lateral incisor Intraoral palatal sinus opening in relation to the carious maxillary central incisor Extraoral sinus opening
- 22. Radiographic features of symptomatic apical abscess A. Localized abscess resulting from an incomplete root canal treatment on a maxillary lateral incisor. B. Cellulitis caused by a maxillary first molar with necrotic pulp.
- 23. DIFFERENTIAL DIAGNOSIS • Periodontal abscess TREATMENT • Establishing drainage and controlling systemic reaction.
- 24. ACUTE EXACERBATION OF ASYMPTOMATIC APICAL PERIODONTITIS (PHOENIX ABSCESS/EXACERBATING APICAL PERIODONTITIS) This condition is an acute inflammatory reaction superimposed on an existing asymptomatic apical periodontitis.
- 25. CAUSES • When chronic periradicular diseases, such as asymptomatic apical periodontitis are in a state of equilibrium, the periradicular tissues are asymptomatic. Sometimes, noxious stimulus from a diseased pulp can cause acute inflammatory response in these dormant lesions. • Lowering of body defences due to influx of bacterial toxins from the root canal or irritation during root canal instrumentation may also trigger acute inflammatory response.
- 26. SYMPTOMS • Initially, tooth may be tender on palpation. • As inflammation progresses, tooth gets elevated from its socket and becomes sensitive. • The mucosa over the radicular area may appear red and swollen and is sensitive to palpation.
- 27. DIAGNOSIS • The radiograph shows a well-defined periradicular lesion. • The patient gives a history of trauma that lead to discolouring of the tooth over a period of time or a post operative pain that subsided until then. • Lack of response to vitality tests diagnoses a necrotic pulp. • On rare occasions, a tooth may respond to the electric pulp test because of fluid in the root canal or in a multirooted tooth.
- 28. A, Radiograph of lower anterior teeth with periapical lucency. B, Upon opening the central incisors, copious amounts of pus drained through the canals. The diagnosis is phoenix abscess.
- 29. DIFFERENTIAL DIAGNOSIS • Acute alveolar abscess TREATMENT • Establishing drainage and controlling systemic reaction.
- 30. ASYMPTOMATIC PERIRADICULAR DISEASES ASYMPTOMATIC APICAL PERIODONTITIS (PREVIOUSLY KNOWN AS CHRONIC APICAL PERIODONTITIS) Asymptomatic apical periodontitis is the symptomless sequelae of symptomatic apical periodontitis and is characterised radiographically by periradicular radiolucent changes and histologically by the lesion dominated with macrophages, lymphocytes and plasma cells.
- 31. CAUSES • It may be seen as a chronic, low grade defensive reaction of the alveolar bone to the irritation from the root canal. • Develops only some time after the pulp has died. • Asymptomatic apical periodontitis is a cell mediated response to pulpal bacterial products. SYMPTOMS • May not produce any subjective reaction, except in rare cases when it breaks down and undergoes suppuration.
- 33. DIAGNOSIS • Discovered by routine radiographic examination. The area of rarefaction is well defined, with lack of continuity of the lamina dura. • An exact diagnosis can be made only by microscopic examination. • Mucosa over the root may or may not be tender to palpation. • Tooth does not respond to thermal or electric pulp tests. • Patient may give a history of pulpalgia that subsided.
- 34. Chronic apical periodontitis in an asymptomatic poorly obturated mandibular molar Radiographic appearance of asymptomatic apical periodontitis. Two distinct lesions are present at the periradicular regions of a mandibular first molar with necrotic pulp.
- 35. DIFFERENTIAL DIAGNOSIS • Cannot be differentiated from other periradicular diseases unless the tissue is examined histologically. TREATMENT • Root canal therapy • Removal of the cause of inflammation is usually followed by resorption of the granulomatous tissue and repair with trabeculated bone.
- 36. CHRONIC ALVEOLAR ABSCESS (CHRONIC SUPPURATIVE APICAL PERIODONTITIS/SUPPURATIVE PERIRADICULAR PERIODONTITIS/CHRONIC APICAL ABSCESS/CHRONIC PERIRADICULAR ABSCESS/CHRONIC PERIAPICAL ABSCESS) A chronic alveolar abscess is a long standing, low grade infection of the periradicular alveolar bone generally symptomless and characterised by the presence of an abscess draining through a sinus tract.
- 37. CAUSES • Source of infection is in the root canal • It is a natural sequelae of death of the pulp with extension of the infective process periapically or it may result from a pre existing acute abscess. SYMPTOMS • Generally asymptomatic or only mildly painful. • At times detected only during routine radiographic examination or because of the presence of sinus tract which can either be intraoral or extraoral.
- 38. DIAGNOSIS • The first sign of osseous breakdown is radiographic evidence seen during routine examination or discoloration of the crown of the tooth. • A radiograph taken after the insertion of a gutta percha cone into the sinus tract often shows the involved tooth by tracing the sinus tract to its origin. • When an open cavity is present in the tooth, drainage may occur by way of root canal. • The PDL is thickened.
- 39. • The rarefied area may be so diffuse as to fade indistinctly into normal bone. • When asked, the patient may remember a sudden sharp pain that subsided and has not recurred, or he or she may relate a history of traumatic injury. • Clinical examination may show a cavity, a composite or a metallic restoration, or a full coverage crown under which the pulp may have died without causing symptoms. • In other cases the patient may complain of slight pain in relation to the tooth, particularly during mastication. • Tooth does not react to electric pulp tests.
- 40. DIFFERENTIAL DIAGNOSIS • Abscess due to presence of a diffuse area • Asymptomatic apical periodontitis due to a circumscribed area • Cyst due to a sclerotic bony outline • Cannot be differentiated from other periradicular diseases unless the tissue is examined histologically. TREATMENT • Elimination of infection in root canal. • Once this end is accomplished and the root canal is filled, repair of the periradicular tissues generally take place.
- 41. RADICULAR CYST (CYSTIC APICAL PERIODONTITIS) Cyst is a closed cavity or sac internally lined with epithelium, the centre of which is filled with fluid or semisolid material. Cysts of the jaws are divided into: • ODONTOGENIC CYSTS arise from odontogenic epithelium and are classified as follicular, arising from the enamel organ or follicle, and radicular arising from the cell rests of mallasez.
- 42. •NON ODONTOGENIC CYSTS are classified as either fissural, arising from epithelial remnants entrapped in the fusion of the facial processes, or nasopalatine, arising from the remnants of nasopalatine duct. •PSEUDOCYSTS or NON EPITHELIAL CYSTS are bony cavities that are not lined with epithelium and therefore, are not truly cysts. They are divided into traumatic cysts, idiopathic bone cavities, and aneurysmal bone cysts.
- 44. CAUSES A radicular cyst presupposes physical, chemical, or bacterial injury resulting in death of the pulp, followed by stimulation of the epithelial rests of mallasez, which are normally present in the PDL. Two distinct categories of radicular cysts were described by Nair: a) periapical pocket cyst b) periapical true cyst
- 45. • PERIAPICAL POCKET CYST-The cyst contains an epithelial lined cavity that is open towards the root canal of the affected tooth. It was originally designated as bay cyst and is now redesignated as the periapical pocket cyst. • PERIAPICAL TRUE CYST-The cyst is characterised by cavities that are completely enclosed in epithelial lining and are totally independent of the root canal of the affected tooth.
- 46. SYMPTOMS No symptoms are associated with the development of a cyst, except incidental to necrosis of the pulp. The pressure of the cyst may be sufficient to cause movement of the affected teeth, owing to accumulation of cystic fluid.in such cases, the root apices of the involved tooth becomes spread apart,so the crowns are forced out of alignment. The teeth may also become mobile. If left untreated,a cyst may continue to grow at the expense of the maxilla or mandible.
- 47. DIAGNOSIS • Tooth does not react to electrical or thermal stimuli,and results of other clinical tests are negative,except the radiograph. • Radiographically, one sees loss of continuity of the lamina dura with an area of rarefaction. • The radiolucent area is generally round in outline,except when it approximates adjacent teeth, in which case it may be flattened and may have an oval shape. • The radiolucent area may be larger than a chronic apical abscess and may include more than one tooth.
- 49. DIFFERENTIAL DIAGNOSIS • Asymptomatic apical periodontitis • Normal bone cavity such as an incisive foramen • Globulomaxillary cyst • Traumatic bone cyst • Lateral periodontal cyst TREATMENT • The treatment of choice is non surgical root canal therapy alone,followed by periodic observation. • Surgical teatment is indicated if a lesion fails to resolve or if symptoms develop.
- 50. CONDENSING OSTEITIS Condensing osteitis is a diffuse radiopaque lesion believed to represent a localised bony reaction to a low grade inflammatory stimulus, usually seen at the apex of a tooth in which there has been a long standing pulpal pathosis.
- 51. CAUSES • It is a mild irritation from pulpal disease that stimulates osteoblastic activity in the alveolar bone. SYMPTOMS • Usually asymptomatic • Discovered during routine radiographic examination DIAGNOSIS • Made from radiographs • Appears as a localised area of radiopacity surrounding the affected root.
- 52. • It is an area of dense bone with reduced trabecular pattern. • The mandibular posterior teeth are most frequently affected.
- 53. A. Apical condensing osteitis associated with chronic pulpitis. Endodontic treatment has just been completed. Obvious condensation of alveolar bone (black arrow) is noticeable around the mesial root of the first molar. Radiolucent area is evident at the apex of the distal root of the same tooth. The retained primary molar root tip (open arrow) lies within the alveolar septum mesial to the molar. B, Resolution (arrow) of apical condensing osteitis shown in A, 1 year after endodontic treatment.
- 54. TREATMENT • Removal of the irritant stimulus • Endodontic treatment should be initiated if signs and symptoms of irreversible pulpitis are diagnosed.
- 55. EXTERNAL ROOT RESORPTION External root resorption is a lytic process occurring in the cementum and dentin of the roots of teeth.
- 56. CLASSIFICATION TOOTH RESORPTION EXTERNAL INTERNAL EXTERNAL SURFACE RESORPTION EXTERNAL INFLAMMATORY ROOT RESORPTION EXTERNAL REPLACEMENT RESORPTION OR ANKYLOSIS
- 57. CAUSES Although unknown, the suspected cause is- • Periradicular inflammation due to trauma • Excessive forces • Granuloma • Cyst • Central jaw tumors • Replantation of teeth • Bleaching of teeth • Impaction of teeth • Systemic diseases • If no cause is evident, the disorder is called idiopathic resorption
- 58. SYMPTOMS • Asymptomatic • When the root is completely resorbed,the tooth may become mobile • If the external root resorption extends into the crown, it will give appearance of “pink tooth” seen in internal resorption • Root resorption of the type called replacement resorption or ankylosis, in which the root is gradually replaced by bone, renders the tooth immobile, in infra occlusion, and with a high metallic percussion sound.
- 59. DIAGNOSIS • Small areas of resorption cannot be seen radiographically and histologically • External inflammatory root resorption is usually diagnosed by radiographs. External resorption appears as concave or ragged areas on the root surface or as blunting of the apex. • Areas of inflammatory resorption caused by the pressure of a growing granuloma, cyst or tumour have an area of root resorption adjacent to the area of radiolucency. • Areas of ankylosis have a resorbed root with no PDL space and with bone replacing the defects.
- 60. DIFFERENTIAL DIAGNOSIS • Internal resorption • In external resorption the radiograph shows a blunting of apex,a ragged area, a “scooped out” area on the side of the root. • In internal resorption one sees a root canal with a well demarcated, enlarged “ballooning” area of resorption.
- 61. TREATMENT • Root canal therapy if caused by extension of pulpal disease • By reducing the excessive forces if caused by orthodontic appliance • In cases of external cervical root resorption, intervention in the form of surgical exposure of the defect and restoration with a suitable restorative material is the treatment of choice before the resorptive defect invades the pulp tissue.
- 62. PERSISTANT APICAL PERIODONTITS It is a post treatment apical periodontitis in an endodontically treated tooth. CAUSES • Apical periodontitis may persist basically because of anatomical complexity of pulp space system with regions that cannot be reached with instruments or with irrigants or intracanal medicaments. • Nair had highlighted certain extra radicular factors that contribute to persistent apical periodontitis. These are- -apical biofilms or periapical plaque -actinomycotic infection
- 63. -Cholesterol crystals -Foreign body reaction to gutta percha -Cellulose granuloma -Periapical scar tissue
- 64. CONCLUSION The periapical diseases are a result of the noxious stimuli in pulp which may be mechanical, thermal, physical or chemical. A tooth affected by periapical diseases should always be treated, it cannot just be ignored. There are two available treatment options, namely to extract the tooth or to perform endodontic treatment and retain the tooth.
- 65. REFERENCES • Grossman’s Endodontic Practice (13th Edition) • Textbook of Oral Pathology by Shafer, Hine & Levy (4th Edition). • Textbook of Endodontics- Nisha Garg. (3rd Edition)
Editor's Notes
- Tender on palpation.
