Fasial palsy
- 1. Presented by Dr. Nishant Kumar
- 2. NERVE FIBER COMPONENTS • Endoneurium • Surrounds each axon • Adherent to Schwann cell layer • Vital for regeneration • Perineurium • Encases endoneural tubules • Tensile strength • Barrier to infection • Epineurium (nerve sheath) • Outermost layer • Houses vasa nervosum for nutrition
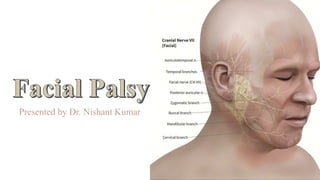
- 3. Nerve of the 2nd branchial arch Has two roots. A large motor and a smaller mixed sensory and parasympathetic (nervus intermedius) Facial nerve
- 4. Functional components • Brancial motor(special visceral efferent)- Supplies; Stapedius , Stylohyoid, posterior belly of digastric muscle and the muscles of facial expression. • Visceral motor(general visceral efferent) Parasympathetic innervations of the lacrimal, submandibular, and sublingual glands, as well as mucous membranes of nasopharynx, hard and soft palate. • Special sensory(special afferent)-Taste sensation from the anterior 2/3 of tongue; hard and soft palates. • General sensory(general somatic afferent)-General sensation from the skin of the concha of the auricle and from a small area behind the ear.
- 5. • Facial nerve is the seventh cranial nerve • Nerve of facial expression • Facial function plays an integral part in our everyday lives • When a facial nerve is either non- functioning or missing, the muscles in the face do not receive the necessary signals in order to function properly. • Facial paralysis is devastating on many levels • Functional • Cosmetic • Fortunately, a plethora of techniques are available to treat the paralyzed
- 6. • The term facial palsy generally refers to weakness of the facial muscles, mainly resulting from temporary or permanent damage to the facial nerve • Facial palsy not only cause a paresis of the target muscles, but as the nerve is responsible for a range of facial expressions, it causes serious disturbances in social life, facial expression being so important in transferring emotion.
- 7. Functions of the facial nerve • Contraction of the muscles of the face • Production of tears from a gland (lacrimal gland) • Conveying the sense of taste from the front part of the tongue (via the chorda tympani nerve) • The sense of touch at auricular conchae
- 8. Level of nerve injury and symptoms
- 9. Facial palsy • Facial paralysis represents the end result of a wide array of disorders and heterogeneous etiologies, including congenital, traumatic, infectious, neoplastic, and metabolic causes. • Thus, facial palsy has a diverse range of presentations, from transient unilateral paresis to devastating permanent bilateral paralysis. although not life-threatening, facial paralysis remains relatively common and can have truly severe effects on one's quality of life, with important ramifications in terms of psychological impact and physiologic burden.
- 10. Facial paralysis Nuclear- from destruction of the nucleus Central or cerebral or Supranuclear Peripheral- from a lesion of the nerve
- 11. Nuclear lesions Supranuclear lesions- usually a part of hemiplegia, only the lower part of the face is paralysed. The upper part (frontalis and part of orbicularis oculi)escapes due to bilateral representation in the cerebral cortex. Infranuclear lesions- entire face is paralysed, as seen in bell’s palsy
- 12. Differences between UMN and LMN type Upper motor neuron Lower motor neuron Upper face is unaffected Both upper and lower face is affected Emotional movements are not affected in unilateral cases .The whole half of the face is paralyzed affecting the emotional movements in bilateral cases Emotional movements are lost . Bells phenomenon is absent Present No atrophy of the facial muscles Atrophy of the affected side is seen Taste sensation is retained Taste sensation is lost. Corneal reflex is not affected Absent Hemiplegia is ipsilateral Hemiplegia is always crossed
- 13. Etiologic Classification Of Facial Palsy • Various classification have been suggested in this respect. • Course of the nerve • Various etiologic causes • Degree of dysfunction observed
- 14. • Vascular abnormalities • CNS degenerative diseases • Tumours of the intracranial cavity • Trauma to the brain • Congenital abnormalities and agenesis Intracranial (central) causes
- 15. • Bacterial and viral infection • Cholesteatoma • Trauma- blunt temporal bone trauma, longitudinal and horizontal fractures of the temporal bone and gunshot wounds. • Tumours invading the middle ear, mastoid and facial nerve • Iatrogenic causes Intratemporalcauses
- 16. • Malignant tumours of the parotid gland • Trauma • Iatrogenic causes • Primary tumours of the facial nerve • Malignant tumours of the ascending ramus of the mandible, pterygoid region and skin. Extracranial causes
- 17. Rainer schmelzeisen classification • Congenital • Moebius syndrome • Myotonic dystrophy • Melkersson rosenthal syndrome • Congenital cholesteatoma • Birth injuries • Osteopetrosis • Neurologic • Myasthenia gravis • Multiple sclerosis • Guillain barre syndrome • Neoplastic • Facial nerve tumours • Glomus tumours • Meningiomas, acoustic • Neuroma • Parotid tumours • Temporal bone/external auditory meatus tumours • Infections • Otitis media, mastoiditis • Bacterial causes • Viral causes
- 18. HOUSE-BRACKMAN(1985) CLASSIFICATION • Grade I-normal function without weakness. • Grade II-mild dysfunction with sligth facial asymmetry with a minor degree of synkinesis. • Grade III-moderate dysfunctions-obvious, but not disfiguring, asymmetry with contracture and/or hemifacial spasm, but residual forehead motion and incomplete eye closure. • Grade IV-moderately severe dysfunction- obvious, disfiguring asymmetry with lack of forehead motion and incomplete eye closure. • Grade V-severe dysfunction-asymmetry at rest and only slight facial movement. • Grade VI-total paralysis-complete absence of tone or motion.
- 19. Bell’s palsy • It is defined as an idiopathic paresis or paralysis of the facial nerve of sudden onset. • The name was ascribed to sir charles bell, who in 1821 demonstrated the separation of motor and sensory innervation of face.
- 20. • Incidence-15-40 cases per 1 lakh cases • Sex predilection- women more affected than men.3.3 more times common in pregnancy and in the third trimester. • Age- can occur at any age, common in middle aged people. • Side involvement- can be equally seen, usually unilateral.
- 21. The palsy is not Bell's if one of the following is present • Signs of tumour • Bilateral simultaneous palsy • Vesicles • Involvement of multiple motor cranial nerves • History and findings of trauma • Ear infection • Signs of central nervous system lesion • Facial palsy noted at birth • Triad of infectious mononucleosis (fever, sore throat, cervical lymphadenopathy).
- 22. Clinical features • There is sudden onset, usually pt gives h/o occurrence after awakening early morning. • Unilateral involvement of entire side of the face. • Abrupt loss of muscular on one side of face. • Inability to smile, close the eye or raise the eyebrow on affected side. • Whistling is not possible.
- 23. • In an attempt to close eyelid, the eyeball rolls upward. • Inability to wrinkle forehead or elevate upper or lower lip. • Obliteration of nasolabial fold. • Face appears distorted and mask like appearance to the facial features. • Speech becomes slurred. • Occasionally there is loss or alternative of taste.
- 24. • Partial paralysis always resolves completely within a few weeks. • Recovery from complete paralysis takes longer (months) and is complete in only about 60-70% of cases. • Approximately 15% of patients are left with troublesome residual palsy and or synkinesis. Course and prognosis
- 25. Psychological Trauma • The most significant complication is the social isolation these patients often succumb to.
- 26. • The most serious complication is corneal damage. • One of the greatest problems with Bell's palsy is the involvement of the eye if the lid fissure remains open. • In this case, eye care focuses on protecting the cornea from dehydration, drying, or abrasions due to insufficient lid closure or tearing Facial paralysis severely hinders: • Normal facial expressions • Mastication • Speech production • Eye protection. Complication
- 27. Assessment and planning • Cause of facial paralysis • Functional deficit/extent of paralysis • Time course/duration of paralysis • Likelihood of recovery • Other cranial nerve deficits • Patient’s life expectancy • Patient’s needs/expectations
- 28. History: • A detailed and careful history • The onset of symptoms , duration, rate of progress, chronology of events and associated features. • History of prior episodes, family history, medical history, history of trauma , and surgical history . Physical examination : • Head and neck examination • Detailed examination of ears, eyes, precise palpation of parotid gland • Complete neurological examination Diagnostic evaluation of facial palsy
- 29. Bell's palsy (1) Acute onset of unilateral facial palsy (2) Numbness or pain of ear, face, neck, or tongue (50%) (3) Viral prodroma (60%) (4) Recurrent facial palsy (12%) (ipsilateral 36%, alternating 64%) (5) Positive family history (14%) (6) Loss of ipsilateral tearing and/or submandibular salivary flow (10%) (7) Decrease in or loss of ipsilateral stapes reflex (90%) (8) Self-limiting and spontaneously remitting
- 30. Herpes zoster cephalicus (1) Same as for Bell's, except pain more common and severe (2) Vesicles on pinna, face, neck, or oral cavity (100%) (3) Sensorineural hearing loss and/or vertigo (40%)
- 31. Tumour (1) Sudden complete onset similar to Bell’s; (2) Recurrent same side (17%) (3) Slowly progressive weakness beyond 3 weeks (59%) (4) No recovery after 6 months (5) Twitching with paresis (6) Mass in parotid, submandibular gland, or neck (7) Mass between ascending ramus and mastoid tip (8) Progression of other motor cranial nerve deficits (9) Some of branches of facial nerve spared (10) History of cancer
- 32. Bilateral simultaneous facial palsy (1) Guillain-Barré (2) Moebius' syndrome (3) Sarcoidosis (4) Myotonic dystrophy (5) Skull trauma (6) Infectious mononucleosis (7) Cytomegalovirus (8) Acute porphyrias (9) Botulism (10) Lyme disease (11) Bell's - herpes simplex
- 33. Birth (1) Congenital diplegia (Moebius’ syndrome, thalidomide toxicity) (2) Lower lip palsy (developmental) (3) Trauma (4) Tumour Trauma Skull fracture (acute or delayed)
- 34. Infection (1) Bulbar palsy (viral meningitis, encephalitis, or immune reaction) (2) Post influenza, rabies, or poliomyelitis immunization (3) Infectious mononucleosis (4) Botulism (5) Tetanus (6) Syphilis (7) Malaria (8) Lyme disease (9) Herpes zoster cephalicus (10) Otitis media (acute or chronic, with or without cholesteatoma) (11) Leprosy
- 35. Metabolic Acute porphyria Neoplastic Acute leukaemia Iatrogenic Bilateral arterial embolization Idiopathic (1) Guillain-Barré syndrome (2) Sarcoidosis (Heerefordt syndrome uveoparotid fever) (3) Polyarteritis nodosa (4) Bell's palsy
- 36. Melkersson-Rosenthal syndrome (1) Recurrent alternating facial palsy (2) Fissured tongue (3) Labial-periorbital facial oedema (4) Non-specific labial granuloma (5) Positive family history.
- 37. Special diagnostic tests for facial palsy Topognosti c tests • Schirmer test, • Stapedial reflex test, • Taste testing • Salivary flow rates and pH Electric al tests • Maximum stimulation tests • Evoked electromyograpthy • Electromyography Radiograph ic tests • CT Scans of temporal bone • MRI • Chest X ray
- 38. Topognostic testing • The principle behind topognostic testing is that lesions distal to the site of a particular branch of the facial nerve will spare the function of that branch Schirmer test : • Evaluates the function of the greater superficial petrosal nerve . • Filter paper is placed in the lower conjunctival fornix bilaterally. • After 3 - 5 minutes, the length of the strip that is moist is compared to the normal side. • A value of 25% or less on the involved side or total lacrimation less than 25 mm is considered abnormal. An abnormal result can indicate injury to the GSPN or to the facial nerve proximal to the geniculate ganglion and may predict patients at risk for exposure keratitis.
- 40. Stapedial reflex: • This test evaluates the stapedius branch of the facial nerve . • One is the most objective and reproducible. • A loud tone is presented to either the ipsilateral or contralateral ear which should evoke a reflex movement of the stapedius muscle. • An absent reflex or reflex that is less than one half the amplitude of the contralateral side is considered as abnormal
- 41. Taste testing: • This test is extremely subjective. • Can be done by placing a small amount of salt, sugar, or lemon juice, quinine and on the tongue. • The patient is asked to indicate that he perceives the taste before he withdraws the tongue. • Loss of taste may indicate interruption of the ipsilateral chorda tympani nerve.
- 42. Taste testing (electrogustometry): • Electirical stimulation (electrogustometry), has the advantages of speed and ease of quantification. • The tongue is stimulated electrically to produce a metallic taste & threshold of the test is compared between two sides. • In normal subjects, the two sides of the tongue have similar thresholds for electrical stimulation. • Thresholds difference of more than 25% is abnormal
- 43. Salivary flow test: • Toevaluate functional integrity of the chorda tympani nerve. • Involves cannulation of Wharton's ducts bilaterally with measurement of output after five minutes. • A 25% reduction in flow of the involved side as compared to the normal side is considered significant. • Salivary pH may be examined as an indirect measure of flow. • As the rate of flow increases, the pH increases. therefore, a pH of less than 6.1 may predict loss of function of the chorda tympani. Disadvantages : • Time consuming • Unpleasant. • Cannot perform repeatedly
- 44. Electrophysiologic tests • These tests are useful for patients with complete paralysis for determining prognosis for return of facial function and the endpoint of degeneration by serial testing. The nerve excitability test (NET) • Is the most commonly used. • This test involves placement of a stimulating electrode over the stylomastoid foramen.
- 45. • The lowest current necessary to produce a twitch on the paralyzed side of the face (threshold) is compared with the contralateral side. • A difference of greater than 3.5 milliamps indicates a poor prognosis for return of facial function. Disadvantage: • Even few intact fibres can elicit a response when rest in • undergoing degeneration. • Muscle twitch response is subjective Uncomfortable procedure • Requires patient co-operation
- 46. The maximum stimulation test (MST) • Is a modified version of the NET. • Instead of measuring threshold, however, maximal stimuli (current levels at which the greatest amplitude of facial movement is seen) is employed. • Increasing current levels are used until maximal movement is seen, and the paralyzed side is compared to the normal side. • Maximal nerve stimulation(~5ma). • Movements on the paralyzed side are subjectively expressed as a percentage (0%, 25%, 50%, 75%, 100%) of the movement on the normal side. • Symmetric response within first ten days – complete recovery > 90%. • No response within first ten days – incomplete recovery with significant sequelae.
- 47. Electromyography: • The recording of spontaneous and voluntary muscle potentials by needles introduced into the muscle is called electromyography (EMG). • Records motor unit potentials of the orbicularis oculi & orbicularis oris muscle during rest & voluntary contraction • In a normal resting muscle biphasic / triphasic potentials are seen every 30- 50msec.
- 48. • Fibrillation potentials typically arises 2-3 weeks following injury. • With regeneration of nerve after injury, polyphasic reinnervation potential replaces fibrillation potential. • Reinnervation potentials may precede clinical signs of recovery by 6-12 weeks. • Polyphasic potential indicate regenerative process & surgical intervention is therefore not indicated. • Fibrillation indicate lower motor neuron denervation but viable motor end plates, so surgical intervention needed(to achieve nerve continuity). • Electrical silence indicates atrophy of motor end plates & need for muscle transfer procedure.
- 49. • Records compound muscle action potential (CMAP) with surface electrodes placed transcutaneously in the nasolabial fold (response) and stylomastoid foramen (stimulus). • Responses to maximal electrical stimulation of the two sides are compared. Evoked Electromyography (EEMG) or Evoked Electroneuronography (ENOG)
- 50. • Waveform responses are analyzed to compare peak-to-peak amplitudes between normal and involved sides where the peak amplitude is proportional to the number of intact axons. • Response <10% of normal in first 3 weeks-poor prognosis. • Response >90% of normal within 3 weeks of onset 80-100% probability of recovery
- 51. • Computed tomography (CT) is valuable for surgical planning in cholesteatomas and temporal bone trauma involving facial nerve paralysis but probably is less useful than MRI in the investigation of atypical idiopathic paralysis. • Magnetic resonance imaging (MRI) with intravenous gadolinium contrast has revolutionized tumor detection in the cerebellopontine angle and temporal bone and is currently the study of choice when a facial nerve tumor is suspected (e.g., in a case of slowly progressive or longstanding weakness). Imaging
- 53. Management of facial palsy Medical Management Steroids Boutulinum toxin Vasodilator therapy Physiotherapy Eye care Reassurance Surgical Management Decompressio n Micro surgery Implants
- 54. Corticosteroids • Prednisolone 1mg/kg. body wt. in divided doses . • Then tapered dependent on whether the paresis progresses to paralysis or remains stable • If the palsy remains stable, we either stop steroids without tapering or rapidly taper the dose for the next 5 days . • If the patient presents with paralysis or progresses to complete paralysis, the dose is proceeded for the next 15 days and tapered in 5 days Ramsey et al. Corticosteroid Treatment for Idiopathic Facial Nerve Paralysis: A Meta-analysis Laryngoscope 110: March 2000
- 55. Boutulinum toxin • Clostridium botulinum toxin (BOTOX) • Neurotoxin • Temporarily interfere with the acetylcholine release from the motor nerve end plates causing skeletal muscle paralysis . • 4 to 6 months • Used to weaken the contralateral side to allow centering of the mouth , more symmetry on smiling and treatment of hypertrophic platysmal bands. Use of Botulinum Toxin A in the Rehabilitation of Facial Nerve Paralysis: A Cases Series. Susana Moraleda,MD (Hospital La Paz,Madrid, Spain); Sandra Espinosa, MD; Mercedes Martinez, MD
- 56. Vasodialators • Stennert’s protocol: In 1979, Stennert devised an infusion therapy • Low molecular wt Dextran I.V infusion 1000cc/day for 3 days over 16 hour period ; reduced to 500 cc/day for 8 days . • Cortisone 200mg/day for 2 days, reduce to 50mg/day in 10 days and stop between 11 & 12 days • Pentoxyphilline 10 mg per day IV • Acyclovir 200 to 400 mg 5 times daily for 10 days
- 57. A. Acute (< 3 wks) 1. Nerve exploration/decompression 2.Nerve repair a.Primary anastomosis b.Cable grafting i.Great auricular nerve ii.Sural nerve B. Intermediate (3 wks- 2 yrs) 1. Nerve transfer a.Hypoglossal-facial b.Spinal accessory-facial c.Masseteric-facial 2.Cross face nerve grafting using sural nerve C. Chronic (>2 yrs) 1. Muscle transfers a.Temporalis b.Masseter c.Digastrics 2.Free muscle flaps/ microneurovascular trans a.Gracilis b.Latissimus dorsi c.Serratus anterior d.Pectoralis minor D. Static procedures/ancillary procedures (can be performed at any time period listed above) 1. Gold weight/spring implants 2.Slings 3.Lid procedures Ryan Ridley. Facial Reanimation .Grand Rounds Presentation, UTMB, Dept. of Otolaryngology Surgical Treatment Modalities
- 58. Nerve decompression • Can be carried out internally or externally • Internal decompression- The nerve is exposed in the fallopian canal and pressure in the canal is relieved by exposing the nerve and the epineural sheath is opened to visualize the nerve fibers and release adhesions or reestablish continuity. • External decompression is done by releasing the epineural sheath from surrounding scar tissue ,bone or foreign body. • To be effective, the surgery must be performed within 2 weeks of the onset of symptoms.
- 60. Micro-neurological Surgery • Facial nerve repair is the most effective procedure to restore facial function in patients who have suffered nerve damage from an accident or during surgery. • It involves microscopic repair of a nerve that has been cut.
- 61. Direct end to end anastomosis • Direct nerve repair: indicated when sharp precise lacerations of facial nerve . • Can be performed with defect < 17 mm. • Can beperformed < 72 hrs of injury • Adequate preparation of nerve ends by resecting devitalized tissue/debris with fine scalpel. • Epineural sheath approximated with 9-0/10-0 nonabsorbable suture(nylon or prolene ) • Avoid tension at suture line
- 63. • Recovery of function begins around 4-6 months and can last up to 2 years following repair • Nerve regrowth occurs at 1mm/day • Goal is tension free, healthy anastomosis
- 64. Nerve grafting • Nerve grafting- whenever there is evidence of neuroma or loss of portion of the nerve, nerve grafting can be considered. • Used when defect > 17mm; nerve cannot be reapproximated without tension • Autogenous nerve grafts remains the standard • The length of the graft should be 20% longer than the gap. • Common donor sites • Greater auricular nerve – up to 10 cm • Sural nerve –for longer grafts(35 cm) • Antebrachial cutaneous nerve
- 65. Greater auricular nerve grafting • Harvesting; • Located on lateral surface of SCM at the midpoint of a line drawn between mastoid tip and mandibular angle • Postauricular incision or use separate neck incision • Advantages: • Proximity to facial nerve • Cross-sectional area • Limited morbidity • Limitations: • Reconstruction of long defects • Ideal for defects < 6cm in length
- 66. Sural nerve • Is the branch of tibial nerve in the middle of the popliteal fossa . • Can be identified adjacent to the lesser saphenous vein posterior to the lateral malleolus • Advantages : • Length : as much as 40 cm • Accessibility • Low morbidity . • Disadvantages: • Variable caliber • Often too large • Difficult to make graft approximation • Unsightly scar
- 67. Median antebrachial cutaneous nerve • Can be harvested from the upper extremity . • Identified adjacent to the basilic vein . • Divides into anterior and posterior branches near antecubital fossa. • Incision parallel to the plane formed by the fascial plane separating the biceps and triceps muscles
- 68. • Branches from the cervical plexus, from the ipsilateral or contralateral side are also most frequently used for facial nerve autografting
- 69. Nerve transposition/ crossover • Nerve transposition is also known as facial- hypoglossal transfer. • Restores movement to the side of the face that has been paralyzed. • With the stump of the 12th nerve hooked up to the end of the 7th nerve, the face will move when the tongue is moved. • Contralateral facial nerve is used to reinnervate paralyzed side using a nerve graft Sural nerve often employed.
- 70. Indications: • Irreversible facial nerve injury • Intact facial musculature/distal facial nerve • Intact proximal donor nerve • Prior to distal muscle/facial nerve atrophy • Ideal if performed within a year of facial paralysis Advantage: • Time interval until movement • 4-6 months • Avoid multiple sites of anastomosis • Mimetic-like function achievable with practice
- 71. Disadvantages : • Surgical intrusion on normal side • Highly specialized technique & longer time • Longer time required for reinnervation from long shafts by which time there may be further muscle atrophy • Results not free of mass movements, synkinesis
- 72. Hypoglossal-Facial Technique 1. Parotidectomy incision extended into cervical crease ~ 2- 3 cm below inferior border of mandible 2. Facial nerve identified and dissected distal to pes anserinus 3. Identify hypoglossal nerve a. SCM retracted posteriorly b. Dissect superiorly until posterior belly of digastic is identified c. Retract digastric superiorly and CN XII is found inferiorly. d. Hypoglossal is within 2-3 c m of main trunk of the facial nerve 4. Hypoglossal nerve is dissected anteriorly and medially into the tongue. 1. Transect distal to ansa hypoglossis 5. Facial nerve transected at the stylomastoid foramen 6. Anastomose nerves using 9-0 epineural suture.
- 73. Hypoglossal Facial Nerve Transfer Entire hypoglossal nerve transected Hypoglossal nerve reflected superiorly Jump graft modification
- 74. Cross-facial nerve grafting • Contralateral facial nerve used to reinnervate paralyzed side using a nerve graft • Sural nerve often employed • ~25-30cm of graft needed • Restitution of smile and eye blinking obtained. • Disadvantage • 2nd surgicalsite • Violation of the normal facial nerve
- 75. Cross-facial nerve grafting Four techniques Sural nerve graft routed from buccal branch of normal vii to stump of paralyzed vii Zygomaticus and buccal branch of normal vii used to reinnervate zygomatic and marginal mandibular portions respectively 4 separate grafts from temporal, zygomatic, buccal and marginal mandibular divisions of normal CN VII to corresponding divisions on paralyzed side. Entire lower division of normal side
- 76. Muscle Transposition (“Dynamic Sling”) • It is employed when there has been long standing paralysis and the muscles of facial expression have atrophied. • The masseter and temporalis muscles are the two most commonly used. Indication: – Congenital facial paralysis – Facial nerve interruption of at least 3 years • Loss of motor endplates – Crossover techniques not possible due to donor nerve sacrifice
- 77. • Often used for reanimation of the oral commisure. • Middle 1/3 of muscle is best for transfer. Temporalis
- 78. Temporalis transfer 1. Incision in preauricular crease extending to superior temporal line 2. Obtain wide exposure of temporalis muscle by dissecting above the SMAS 3. Incise down on periosteum to elevate muscle fibers - Harvest middle 1/3 4. Large tunnel created over zygomatic arch 5. Orbicularis oris muscle exposed via vermilion border incision at oral commissure 6. Large tunnel over zygomatic arch used to connect oral commisure to zygomatic arch/superior incision. 7. Temporalis flap detached and elevated from its origin and tunneled to the oral commissure. 8. 3-0 prolene used to suture orbicularis to temporalis at oral commissure 9. Overcorrection of nasolabial fold and oral commissure
- 79. Masseter • Used when temporalis muscle is not opted. • May be preferred due to avoidance of large facial incision Disadvantage: – Less available muscle compared to temporalis – Vector of pull on oral commisure is more horizontal than superior/oblique like temporalis
- 80. Masseter transfer 1. Expose muscle with gingival incision along mandibular sulcus 2. Dissection carried out in a plane between mucosa and muscle. 3. Muscle freed off of mandible medially and from the inferiolateral edge of mandible. 4. Vertical incision made in inferior portion of muscle 5. Anterior half of muscle is split into 2 divisions. 6. The 2 anterior slips of muscle are tunneled anteriorly to reach the oral commisure via external vermillion border incisions. 7. Muscle slips are attached to lips and oral commisure in the deep dermal layer using suture
- 81. • They have potential of achieving individual segmental contractions reduction of synkinesis • Muscle flaps used are: • Gracilis • Latissimus dorsi • Inferior rectus abdominus Microneurovascular transfer free muscle flaps
- 82. • Requires viable muscle and nerve innervation • They have potential of achieving individual segmental contractions • Reduction of synkinesis • Traditionally done in 2 stages • 1st: cross-face nerve graft 1 yr prior to muscle transfer • 2nd:muscle transfer performed after neural ingrowth of graft, 9 to 12 months later.
- 83. Gracilis • “Workhorse” for free muscle transfer • Long, thin muscle in medial thigh -Good neurovasular pedicle • Adductor artery and vein • Anterior obturator nerve • 2 stages involved: • Sural nerve employed for cross-face graft • Gracilis muscle transferred after 6-12 months • Vascular anastomosis to the facial artery and vein or to superficial temporal vessels. Anterior Obturator nerve Adductor a. & v.
- 84. • Static facial suspension is used to lift the corner of the mouth so that balance is restored to the face and drooling out of the mouth is helped. Indications: • Debilitated individuals; poor prognosis • Nerve or muscle not available for dynamic procedures • Adjuct procedure with dynamic techniques to provide immediate benefit Advantages: • Immediate restoration of facial symmetry at rest • No oral commissure ptosis • Drooling, disarticulation, mastication difficulties • Relief of nasal obstruction caused by alar collapse Static slings
- 85. • Variety of materials used • PTFE (Polytetrafluoroethylene) (Gor-Tex) • Alloderm • Fascia lata • Gor-Tex and alloderm have advantage of no donor site morbidity but higher risk of infection.
- 86. Static facial sling technique 1. Preauricular, temporal or nasolabial fold incision may be used 2. Additional incisions made adjacent to oral commisure at vermillion border of upper and lower lip 3. Subcutaneous tunnel dissected to connect temporal to oral commisure incisions 4. Dissection may be carried out in midface adjacent to nasal ala, if needed (for alar collapse) 5. Implant strip is split distally to connect to the upper/lower lips 6. Implant secured to orbicularis oris/commisure using permanent suture 7. Implant is suspended and anchored superiorly to superficial layer of deep temporal fascia, or zygomatic arch periosteum, using permanent suture.
- 87. Addressing paralytic eyelids Complications of orbicularis oculi paresis • Delayed blinking • Impairment of nasolacrimal system • Dry eye • Risk of exposure keratitis, corneal ulceration and blindness Goal of treatment is to maintain cornea Treatment options • Tarsorrhaphy • Gold weight/spring implants • Open / endoscopic brow lifts for significant brow ptosis
- 88. Gold weight implantation 1.Small incision made several millimeters above the upper eyelid margin. 2.Tarsal plate exposed with sharp dissection. 3.Gold weight secured to tarsus using 8-0 nylon. 4.Wound closed in 2 layers.
- 89. Tarsorrhaphy • Tarsorrhaphy is a surgical procedure in which the eyelids are partially sewn together to narrow the eyelid opening. • Horizontal mattress 5-0 nylon. • Begin 3mm medial to lateral canthus, 6mm from lid margin. • Stitch travels through gray line to 5mm below lower lid margin. • Cosmetically unappealing, visual field affected.
- 90. • Addresses the aging neck and lower two-thirds of the face. • A small window is made in the orbicularis oculi muscle just lateral to the lateral orbital rim at the lateral canthus level with deep temporal fascia exposed. • Suture is with consecutive bites of 0.5 cm to 2 cm below the lateral canthus in a purse-string fashion causing microimbrications in a subcutaneous plane. • This technique provides a simple, quick, and stable result for midface elevation and support of the lower eyelid, reducing vertical lid height. • However, it does result in excess lower eyelid skin Minimal Access Cranial Suspension (MACS) Lift
- 91. • Patients with a ‘‘negative vector’’ have poor lower lid support and are particularly challenging to manage in facial paralysis. • They tend to develop lower lid retraction that is not amenable to typical techniques such as tarsal strip procedures. • Often, a midface-lift is necessary to support the lower lid. • The author prefers the subperiosteal midfacelift utilizing the CoApt midface Endotine .
- 92. • The nose • The collapse of the nasal side wall can be corrected either from the outside or the inside of the nose. • Outside techniques involve placing strips of suspension material from the cheekbone, under the skin, to the nasal sidewall , and suspending the nasal sidewall in its anatomic position, • To widen the nasal cavity from inside small cartilage gtafts can be inserted into the framework of the nose.
- 93. Adjunctive procedures Soft tissue procedures to improve symmetry • Rhytidectomy • Excision of redundant intraoral mucosa • Blepharoplasty • Brow lift Procedures for drooling • Wilkie procedure • Submandibular gland resection with parotid gland ligation Modification of normal side to improve symmetry • Neurectomy • Myectomy
- 95. Recent advances • Surgeons from UC Davis Medical Center have demonstrated that artificial muscles can restore the ability of patients with facial paralysis to blink • Sling that is attached to the electroactive polymer artificial muscle device (EPAM) after passing through an interpolation unit that is implanted in the lateral orbital wall (note screw fixation). The power supply and artificial muscle are implanted in the temporal fossa. conceptually, when the normal right eyelid blinks, the electrical sensor (green) sends a signal to the battery to activate the EPAM
- 96. • The basic EPAM is a three layered structure with a thin film of dielectric elastomer layered on each side with conductive electrodes made of carbon particles suspended in a soft polymer matrix. • When a voltage is applied to the electrodes, they attract to each other and expand, compressing the dielectric elastomer and expanding the sheet. • Removal of the voltage contracts the sheet. • Additional study will needed, including biocompatibility and durability studies, which are being performed, for further development of the EPAM device.
- 97. • Addressing paralytic eyelids • More recently, flexible platinum chains have been used as this is better able to contour the upper eyelid tarsus, of lower profile with the same mass secondary to a higher density and better biocompatibility.
- 98. Conclusion • The human face signals expressions of happiness, anger, fear, and surprise that appear to be universal in character. • Impairment of the facial nerve interferes with the transmission of this intimate information that is an essential addition to the flow of our conversation that significantly supplements the meaning of our speech. • Therefore it is highly essential to have a precise diagnosis of the problem and then the surgeon should use his skill and imagination to bring back the expressions of the face which will eventually take a long way in improving the patients functional esthetical and emotional status.
- 99. Thank you
