Cme one size fits all - final
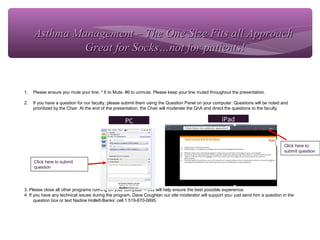
- 1. HOUSEKEEPING 1. Please ensure you mute your line. * 6 to Mute. #6 to unmute. Please keep your line muted throughout the presentation. 2. If you have a question for our faculty, please submit them using the Question Panel on your computer. Questions will be noted and prioritized by the Chair. At the end of the presentation, the Chair will moderate the QnA and direct the questions to the faculty. 3. Please close all other programs running on your computer – this will help ensure the best possible experience. 4. If you have any technical issues during the program, Dave Coughlan our site moderator will support you- just send him a question in the question box or text Nadine Hollett-Banks’ cell 1.519-870-0695. Click here to submit question PC iPad Click here to submit question Asthma Management – The One Size Fits all ApproachAsthma Management – The One Size Fits all Approach Great for Socks…not for patients!Great for Socks…not for patients!
- 2. Asthma Management – The One SizeAsthma Management – The One Size Fits all ApproachFits all Approach Great for Socks…not for patients!Great for Socks…not for patients! Anne K. Ellis, MD MSc FRCPCAnne K. Ellis, MD MSc FRCPC Associate Professor and ChairAssociate Professor and Chair Division of Allergy & Immunology Department of Medicine, Queen’s University ellisa@kgh.kari.net Twitter: @DrAnneEllis Date: Sept 22nd , 2015 Time: 12:15h
- 3. Disclosures Facilitator’s Name: Dr. Anne K. Ellis Grants/research support: Circassia Ltd/Adiga Life Sciences GlaxoSmithKline Novartis SunPharma Advanced Research Corporation Merck Speaker’s bureau/honoraria: Merck, Pfizer, AstraZeneca, Novartis Consulting fees: ALK Abello, Ora Inc. Advisory Boards: Merck, Novartis
- 4. Objectives ∗ By the end of this learning session, the attendee will be able to: ∗ Describe differences in performance characteristic of the various asthma controller therapies ∗ Develop a patient focused approach to asthma management ∗ Learn where to access educational resources for patients
- 5. Introduction - Asthma ∗ Chronic inflammatory lung disorder characterized by: ∗ reversible airflow obstruction ∗ airway hyperresponsiveness ∗ Presents symptomatically with dyspnea, wheeze and sensation of chest tightness
- 7. Barnes PJ. Clin Exp Allergy 1996;26:738-745.
- 8. Diagnosis of Asthma ∗ Confirmed when compatible symptom pattern is accompanied by objective measures of variable airflow obstruction ∗ Spirometry: ∗ >12% improvement in FEV1 15 mins after SABA ∗ OR >20% improvement after 10-14 days of oral prednisone ∗ OR >20% spontaneous variability ∗ Serial PEF ∗ >20% change after bronchodilation or over time ∗ Methacholine challenge ∗ 20% reduction in FEV1 with provocative concentration of methacholine Boulet L, et al. CMAJ 1999;161(11 Suppl):S1-61, Kaplan AG. CMAJ 2009;181:E210-20 FEV1: forced expiratory volume in 1 second, SABA: short-acting bronchodilator
- 9. Asthma – Phenotypes ∗ Eosinophilic Bronchitis ∗ Steroid-responsive ∗ Typically atopic ∗ Neutrophilic bronchitis ∗ Less steroid-responsive ∗ Smoking, viral illness, others ∗ Non-inflammatory ∗ Obesity, others
- 10. Allergic Asthma ∗ Allergen contact with airway mucosa in a sensitized individual results in rhinitis, conjunctivitis, and asthmatic responses ∗ Immediate allergic response maximal 15 to 30 min after allergen challenge, resolves in 1 to 3 hours ∗ ~50% of subjects develop a late-phase allergic response ∗ persistent, less reversible decrease in pulmonary function ∗ maximal in 6-12h and partially resolves within 24h
- 11. Late Phase Asthmatic Response
- 12. The Prevalence of Asthma in Canada: 1.Has increased steadily over the past 20 years 2.Is one of the highest in the world 3.Affects a large portion of the pediatric population 4.Affects nearly 3 million people in Canada 5.All of the above Polling Question: Epidemiology of Asthma in Canada Statistics Canada. Available at:Statistics Canada. Available at: www40.statcan.ca.www40.statcan.ca. Asthma Society of Canada. Available at:Asthma Society of Canada. Available at: www.asthma.cawww.asthma.ca..
- 13. Epidemiology of Asthma in Canada ∗ Prevalence increased over past 20 years among adults until 2001 and remains one of the highest in the world ∗ 1979: 2.3% ∗ 1988: 4.9% ∗ 1994: 6.1% ∗ 2001: 8.4% ∗ 2009: 8.4% ∗ At least 12% of children have asthma Statistics Canada. Available at: www40.statcan.ca. Asthma Society of Canada. Available at: www.asthma.ca.
- 14. Asthma Triggers ∗ Allergens ∗ Dust mites, mold spores, animal dander, cockroaches, pollen, indoor and outdoor pollutants, irritants (smoke, perfumes, cleaning agents) ∗ Pharmacologic agents (ASA, beta-blockers) ∗ Physical triggers (exercise, cold air) ∗ Physiologic factors ∗ Stress, GERD, viral and bacterial URI, rhinitis
- 15. Lung Function Declines with Frequency o Asthma Exacerbations Bai T.Bai T. Eur Respir J 2007;30:452-456Eur Respir J 2007;30:452-456 P<0.05P<0.05 AnnualchangeinFEVAnnualchangeinFEV11mL/yrmL/yr 00 ––1010 ––2020 ––3030 ––5050 ––4040 InfrequentInfrequent ExacerbationsExacerbations FrequentFrequent
- 16. Factors Leading to Inadequate Asthma Control ∗ Wrong diagnosis or confounding illness ∗ Incorrect choice of inhaler or poor technique ∗ Concurrent smoking ∗ Concomitant rhinitis ∗ Individual variation in treatment response ∗ Undertreatment ∗ Unintentional or intentional nonadherence Haughney J, et al. Respir Med 2008;102:1681-1693Haughney J, et al. Respir Med 2008;102:1681-1693
- 17. Goals of Asthma Management ∗ Achieve and maintain control of symptoms ∗ Prevent asthma exacerbations ∗ Maintain optimal pulmonary function ∗ Maintain normal activity levels (+ exercise) ∗ Avoid adverse effects from asthma medications ∗ Prevent the development of irreversible airflow obstruction ∗ Prevent asthma mortality GINA: Global Strategy for Asthma Management and Prevention, 2009GINA: Global Strategy for Asthma Management and Prevention, 2009 1717
- 18. What are the drugs? What are the devices?
- 19. Asthma Medications 1919 Treatment Effects Most common AEs Relievers Short-acting beta-2 agonists • Use on-demand only at min. dose and frequency • Tremor, palpitations, restlessness, headache, muscle cramps, nervousness Controllers Inhaled corticosteroids • For persistent asthma • Not intended as rescue med. • May take 1-2 weeks to see benefits • Local: Oral candidiasis, dysphonia, reflex cough and bronchospasm • Systemic: ↓ bone density, poor growth, adrenal gland suppression, bruising, ↑ blood sugar Leukotriene receptor antagonists • Alternative for persistent asthma and as add-on to ICS • Headaches, stomach pain, and cough Anti-IgE MAb • For moderate to severe asthma with frequent need for oral CS • Headache, malaise, anaphylaxis LemièreLemière et al. Can Respir J 200et al. Can Respir J 2004;11 Suppl A:9A-18A4;11 Suppl A:9A-18A Irwin R. Chest 2006;130(1 Suppl):41S-53SIrwin R. Chest 2006;130(1 Suppl):41S-53S
- 20. Asthma Medications (cont’d) Treatment Effects Most common AEs Add-on therapies Long-acting beta-2- agonists • Improves asthma control in older children and adults • Only to be used as an add-on when asthma not controlled with ICS • Not to be used as monotherapy • Tachycardia, palpitation, irritability, insomnia, muscle cramps, tremor LemièreLemière et al. Can Respir J 200et al. Can Respir J 2004;11 Suppl A:9A-18A4;11 Suppl A:9A-18A
- 22. Canadian Thoracic Society Asthma Management Continuum LABA = long-acting beta agonistLougheed MD, et al. Can Respir J 2010; 17(1):15-24. <6 yr of age < 100 mcg/day<6 yr of age < 100 mcg/day
- 23. Asthma Management - Details ∗ Allergen and Irritant Avoidance ∗ Avoidance of other triggers (e.g. cold air, influenza vaccine, NSAIDs in sensitive px’s) ∗ Education, education, education ∗ Assessment of Control at each patient visit
- 24. I judge patient’s asthma control by: 1.Need for fast-acting beta-agonist 2.Physical activity 3.Night time symptoms 4.Exacerbations 5.Absence from work or school Polling Question: Indicators of Asthma Control Statistics Canada. Available at:Statistics Canada. Available at: www40.statcan.ca.www40.statcan.ca. Asthma Society of Canada. Available at:Asthma Society of Canada. Available at: www.asthma.cawww.asthma.ca..
- 25. Indicators of Asthma Control Characteristic Frequency or Value Daytime symptoms < 4 days/week Night-time symptoms < 1 night/week Physical activity Normal Exacerbations Mild, infrequent Absence from work or school due to asthma None Need for a fast-acting beta-agonist < 4 doses/week FEV1 or PEF ≥ 90% personal best PEF diurnal variation† < 10% to 15% FEV1 = forced expiratory volume in 1 second; PEF = peak expiratory flow. † Diurnal variation is calculated as the highest PEF minus the lowest divided by the highest PEF multiplied by 100 for morning and night (determined over a 2-week period). Lougheed MD, et al. Can Respir J 2010; 17(1):15-24. Educate Patients That This Level of Asthma Control is Generally Achievable
- 26. Actual and Perceived Asthma Control in Canada: TRAC Study 100 Patients(%) Actual (based on CACG) 53% 80 60 40 20 60 47% 3% 97% 12% 88% 10% 90% Patients General practitioners Specialists Perceptions CACG = Canadian Asthma Consensus Guidelines. FitzGerald JM, et al. Can Respir J 2006; 13(5):253-9. Not controlled Controlled
- 27. Why Don’t Patients Take Asthma Medications as Prescribed? ∗ Most do not want to take daily medications when they feel well and have no asthma symptoms ∗ Many believe they know when they need to take their asthma medications ∗ Most use SABAs because these work quickly ∗ Many do not know or believe that poor current asthma control results in future risks SABA = short-acting beta agonist.SABA = short-acting beta agonist.
- 28. Short Acting Beta-Agonists (SABA) ∗ Onset of action 5 to 15min, duration ~4 hr ∗ Salbutamol (Ventolin®) ∗ MDI (100 mcg) ∗ Diskus (200 mcg) ∗ Terburtaline (Bricanyl®) ∗ Turbuhaler (500 mcg)
- 29. Long Acting Beta-Agonists (LABA) ∗ Black Box warning against monotherapy ∗ Only for 12 yr of age and up ∗ Salmeterol (Serevent®) ∗ Maximal dose 100 mcg/day ∗ Onset of action ~ 1 hr ∗ MDI – 25 mcg; Diskus – 50 mcg ∗ Formoterol (Oxeeze®) ∗ Maximal dose 48 mcg/day ∗ Onset of action ~ 15 min ∗ Turbuhaler – 6 mcg
- 30. Inhaled Corticosteroids Generic Name Formulation Doses Beclomethasone (QVAR®)*** Inhalation aerosol (MDI) 50 mcg 100 mcg Fluticasone (Flovent®) Dry powder for inhalation (Diskus**) ¥ ¥ Contains lactose/milk protein Inhalation aerosol (MDI)* 50 mcg 100mcg 250 mcg 500 mcg 50 mcg 125 mcg 250 mcg Budesonide (Pulmicort®)*** Dry powder for inhalation (Turbuhaler) 100 mcg 200 mcg Ciclesonide (Alvesco®)*** Inhalation aerosol (MDI) 100 mcg 200mcg Mometasone (Asmanex®)§ Dry powder for inhalation (Twisthaler)** 200 mcg 400 mcg ***6 yoa and up***6 yoa and up § 12 yoa and up§ 12 yoa and up**4 yoa and up**4 yoa and up*12 mo and up*12 mo and up
- 31. Available ICS + LABA Single-inhaler Combinations Advair® Product Monograph. GlaxoSmithKline Inc., July 2010. Symbicort® Product Monograph. AstraZeneca Canada Inc., December 2010. ZenhaleTM Product Monograph. Merck Canada Inc., January 2011. Combination Formulation Doses Fluticasone + salmeterol (Advair®) Dry powder for inhalation (Diskus¥ ) ¥ Contains lactose/milk protein Inhalation aerosol (MDI) 100 mcg/50 mcg 250 mcg/50 mcg 500 mcg/50 mcg 50 mcg/25 mcg 125 mcg/25 mcg 250 mcg/25 mcg Budesonide + formoterol (Symbicort®) Dry powder for inhalation (Turbuhaler) 100 mcg/6 mcg 200 mcg/6 mcg Mometasone + formoterol (Zenhale®) Inhalation aerosol (MDI) 50 mcg/5 mcg 100 mcg/5 mcg 200 mcg/5 mcg
- 32. Use of Asthma Inhalers/Meds ∗ PRN SABA alone ∗ Fixed dose ICS (and/or LTRA); PRN SABA ∗ Fixed dose ICS/LABA (± LTRA); PRN SABA ∗ At times of acute exacerbation, double or quadruple ICS dose or introduce oral CS ∗ Single inhaler Maintenance and Rescue Therapy (SMART) – Fixed dose ICS/LABA and PRN ICS/LABA* ∗ * Only effective if the LABA is formoterol due to onset of action differences ∗ * Only Health Canada approved for Symbicort®
- 33. ICS Safety: Key Pharmacokinetic and Pharmacodynamic Properties ICS Oral bio- availability (%) Receptor binding affinity Protein binding (%) Beclomethasone 15 53/1,345a 87 Budesonide 11 935 88 Fluticasone < 1 1,800 90 Mometasone < 1 2,200 98-99 Ciclesonide < 1 12b /1,212c 99 Key characteristics: ↑ receptor binding/potency ↑ lipophilicity ↑ plasma protein binding ↑ metabolism ↓ bioavailablity ↓ systemic exposure ↑ therapeutic index Rossi GA, et al. Pulm Pharmacol Ther 2007; 20(1):23-35. Bousquet J. Int J Clin Pract 2009; 63(5):806-19. a Relative receptor affinity for 17-beclomethasone monopropionate. b Ciclesonide. c Desisobutyryl-ciclesonide
- 34. Corticosteroid Trade name Daily ICS dose, mcg^ Adult (>12 years old) Low Medium High Beclomethasone dipropionate HFA QVAR† ≤250 251-500 >500 Budesonide* Pulmicort Turbuhaler‡ ≤400 401-800 >800 Ciclesonide* Alvesco§ ≤200 201-400 >400 Fluticasone Flovent MDI and spacer; Flovent Diskus¶ ≤250 251-500 >500 Mometasone Asmanex Twisthaler** 200 400 >400 Adapted from Lougheed MD, et al. Can Respir J. 2012;19:127-64. ^Comparative clinical significance has not been established What is Low Dose ICS?
- 35. LABA Differences: Onset of Bronchodilation **pp ≤ 0.016 vs. fluticasone + salmeterol.≤ 0.016 vs. fluticasone + salmeterol. Bernstein DI, et al. Allergy Asthma Clin Immunol 2010; 6 (Suppl 2):33.Bernstein DI, et al. Allergy Asthma Clin Immunol 2010; 6 (Suppl 2):33. 350350 MeanchangefrombaselineinFEVMeanchangefrombaselineinFEV11(mL)(mL) Minutes post doseMinutes post dose 00 300300 250250 200200 150150 100100 5050 00 55 1010 1515 2020 2525 3030 3535 4040 4545 5050 5555 6060 ** ** ** ** Mometasone + formoterol 200/10 mcg bidMometasone + formoterol 200/10 mcg bid Fluticasone + salmeterol 250/50 mcg bidFluticasone + salmeterol 250/50 mcg bid
- 36. ∗ Specific for CysLTR1 ∗ CysLT2 is present in the lung but appears to be confined to blood vessels ∗ Available agents: ∗ Singulair® = montelukast ∗ 4mg, 5mg and 10mg tablets, dosing is OD ∗ Accolate® = zafirlukast ∗ 20mg BID Leukotriene Receptor Antagonists (LTRA’s)
- 37. ∗ Montelukast is approved for use in children 1 year of age and older for asthma and 2 years of age and older for allergic rhinitis ∗ Pregnancy category B ∗ Zafirlukast approved for children 12 y and older ∗ Pregnancy category B Leukotriene Receptor Antagonists (LTRA’s)
- 38. Personalized Asthma Treatment ∗ Assess patient preference and ability to use device(s) ** ∗ Patients fearful of ICS, evaluate steroid alternatives for maintenance, such as LTRAs; ensure Aerochamber in use ∗ Ask patient about desire for rapid onset, and select the ICS/LABA accordingly ∗ Choose ICS with lowest bioavailability and associated with lowest risk of adverse effects but that also produces desired efficacy outcomes
- 39. Patient Compliance to ICS Therapy Can Prevent Asthma Deaths Suissa S, et al. N Engl J Med 2000; 343(5):332-6.Suissa S, et al. N Engl J Med 2000; 343(5):332-6. Fitted rate ratio for death from asthma as a functionFitted rate ratio for death from asthma as a function of the number of canisters of ICS used during yearof the number of canisters of ICS used during year before index date.before index date. 2.52.5 RateratiofordeathfromasthmaRateratiofordeathfromasthma 2.02.0 1.51.5 1.01.0 0.50.5 00 Number of canisters of ICS per yearNumber of canisters of ICS per year 3311 44 55 12129988 1010 111166 7700 22
- 40. Non-adherence to Asthma Therapy Intentional Motivation Beliefs/preferences Perceptual barriers Non-intentional Capacity and resources Practical barriers Barriers to assessing adherence: Patient and physician may prefer to avoid the subject Lack of clear, easy methods for addressing barriers to adherence Perception that little can be done? Horne R, et al. Chest 2006;130:65SHorne R, et al. Chest 2006;130:65S--72S72S 4040
- 41. Strategies to Improve Adherence ∗ Focus on patient education ∗ Ensure language at appropriate level ∗ Write it down ∗ Consider referral to an asthma educator ∗ Encourage self-monitoring ∗ Use a written asthma action plan ∗ Monitor adherence to medication regimen and proper inhaler techniques ∗ Combination therapy may improve complianceNational Heart, Lung, and Blood Institute National Asthma Education and Prevention Program Expert Panel.National Heart, Lung, and Blood Institute National Asthma Education and Prevention Program Expert Panel. Guidelines for the Diagnosis and Management of Asthma Full Report 2007Guidelines for the Diagnosis and Management of Asthma Full Report 2007 Stoloff SW, et al. J Allergy Clin Immunol 2004;113:245-251Stoloff SW, et al. J Allergy Clin Immunol 2004;113:245-251 4141
- 42. Asthma Education Centres A link to this resource has been posted as a hand out in your control panel that you can download.
- 43. Unique Considerations ∗ Pediatrics ∗ Allergic Asthma
- 44. Pediatric Considerations ∗ Diagnostic challenge before age 5 ∗ Atopy risk factor for persistence of childhood wheeze ∗ Lower ICS doses usually sufficient ∗ Aerochambers not optional – discussion of benefits can improve adherence ∗ Adherence to oral/non-steroidal therapy often higher but must assess patient response ∗ Spirometry generally becomes reliable around age 8 to 10 to provide objective assessment of disease
- 45. Unique considerations – Allergic Population ∗ Allergic rhinitis and asthma often co-exist ∗ Treating rhinitis improves asthma outcomes ∗ Remember to treat with INCS as well ∗ LTRA’s indicated for both, as is omalizumab and immunotherapy ∗ Dual targets one medication: ∗ LTRAs ∗ Allergen specific immunotherapy ∗ Omalizumab
- 46. Biologic Therapy ∗ Omalizumab (Xolair®) ∗ Monoclonal antibody against IgE molecule ∗ Indicated for moderate to severe allergic asthma ∗ Shown to decrease hospitalizations, ER visits, and requirements for oral corticosteroids ∗ Typically given under specialist supervision (injection, risk of anaphylaxis)
- 47. Allergen immunotherapy ∗ Reached its 100th anniversary (Noon, 1911) ∗ Currently, subcutaneous immunotherapy (SCIT), a.k.a ‘allergy shots’ established as effective in the treatment of IgE-mediated reactions to: ∗ Hymenoptera venom ∗ Allergic rhinitis ∗ Allergic asthma
- 48. What is immunotherapy? ∗ Decrease allergen sensitivity via gradual administration of increasing doses of allergen extracts ∗ Advances over last 25 yrs include improved quality of extracts, better understanding of underlying immune mechanisms ∗ Modifies immune response from an allergic, inflammatory pattern to a more protective, less damaging response ∗ IT and allergen avoidance are the only treatments that modify the natural history of allergic disease, inducing remission and/or long-term cure
- 49. Efficacy in Asthma ∗ Confirmed in 3 meta-analyses of RCTs of specific immunotherapy for patients with allergic asthma ∗ Most recent included 75 trials involving over 3500 patients ∗ 33 dust mite ∗ 20 pollen ∗ 10 animal ∗ 2 mould ∗ 6 multiple aeroallergens Abramson et al. Cochrane Database System Rev 2009Abramson et al. Cochrane Database System Rev 2009
- 50. Efficacy ∗ Standardized Mean Difference in symptoms scores were best for dust mite and all pollens; overall SMD -0.72 (95% CI -0.99 to -0.44) ∗ If studies reported better, same, worse: ∗ Overall NNT = 4 to prevent one asthma deterioration ∗ Pollen NNT = 3 ∗ NNT = 5 to prevent one increase in medication requirements; NNT = 4 to prevent worsening of BHR
- 51. Established aspects ∗ Effective doses of allergen extract: ∗ Ragweed ∗ Timothy ∗ Birch ∗ D. pteronyssinus ∗ D. farinae ∗ Cat dander ∗ Dog dander ∗ Duration: ∗ After 5 years of SCIT, benefit generally persists ∗ If after 1-2 years at an appropriate maintenance dose, and no benefit noted, can discontinue Rx
- 52. Safety of Immunotherapy ∗ Local, systemic, and even fatal reactions are a recognized complication of SCIT ∗ Large local reactions not predictive of future systemic reactions (SRs) ∗ Incidence of SRs a function of: ∗ Patient sensitivity ∗ Dose ∗ Modifications to extract ∗ Systemic reactions to SCIT occur in 0.9 – 3.3% of injections with traditional schedules ∗ Rush protocols, up to 38% Nelson. J Allergy Clin Immunol 2007Nelson. J Allergy Clin Immunol 2007
- 53. Additional Agents/On the Horizon Ipatropium bromide (Atrovent®) 500 ug q4h PRN Tiotropium bromide (Spiriva®) 18 mg QAM Mepolizumab (Mepo®) Monoclonal anti-IL-5 antibody Other biologics?
- 54. Summary ∗ Asthma is a chronic disease–control inflammation to prevent symptoms ∗ Avoidance of triggers with ongoing education essential components of asthma management ∗ Review device technique/adherence whenever possible ∗ Uncontrolled asthma and severe exacerbations accelerate decline in lung function ∗ Unique considerations in allergic populations ∗ United airways; Disease modifying therapy
- 55. Questions? ∗ ellisa@queensu.ca or ellisa@kgh.kari.net ∗ Twitter: @DrAnneEllis
Notas do Editor
- If a patient exhibits symptoms suggestive of asthma, the diagnosis should be confirmed using objective measurements to show variable airflow obstruction. The preferred method of assessment is spirometry. An improvement in FEV1 of 12% or greater (ie, at least 180 mL) from baseline 15 minutes after the use of an inhaled short-acting β2agonist (SABA), a 20% (250 mL) or greater improvement after a 10- to 14-day trial of oral prednisone when symptoms are stable, or a 20% (250 mL) or greater “spontaneous variability” is considered significant. Additional measures of airway obstruction include serial measures of PEF and methacholine challenge. Change in serial measures of PEF of greater than 20% after administration of a bronchodilator over time, or a 20% reduction in FEV1 following a provocative concentration of methacholine (up to 8 mg/mL) is suggestive of asthma. Reference: Boulet LP, Becker A, Bérubé D, Beveridge R, Ernst P. Canadian Asthma Consensus Report, 1999. Canadian Asthma Consensus Group. CMAJ 1999;161(11 Suppl):S1-61.
- The World Health Organization reported in 1995 that there were more than 100 million people around the world with asthma. While a precise cause has yet to be determined for the steady rise in asthma prevalence, such a rise has been observed around the world and in Canada. In 2001 and 2009, Statistics Canada reported a prevalence of 8.4% for diagnosed asthma among those aged 12 and older. The disease is most common during childhood, and the prevalence among Canadian children was estimated to be at least 12% in the National Population Health Survey of 1996-1997. References: Statistics Canada. Asthma, by age group and sex. Available at: www40.statcan.ca. Accessed February 2011. Asthma Society of Canada. Asthma Facts & Statistics. Available at: www.asthma.ca. Accessed February 2011.
- The World Health Organization reported in 1995 that there were more than 100 million people around the world with asthma. While a precise cause has yet to be determined for the steady rise in asthma prevalence, such a rise has been observed around the world and in Canada. In 2001 and 2009, Statistics Canada reported a prevalence of 8.4% for diagnosed asthma among those aged 12 and older. The disease is most common during childhood, and the prevalence among Canadian children was estimated to be at least 12% in the National Population Health Survey of 1996-1997. References: Statistics Canada. Asthma, by age group and sex. Available at: www40.statcan.ca. Accessed February 2011. Asthma Society of Canada. Asthma Facts & Statistics. Available at: www.asthma.ca. Accessed February 2011.
- Factors that influence the risk of asthma can be divided into those that cause the development of asthma (primarily genetic) and those that trigger asthma symptoms (usually environmental). Common triggers include allergens, such as dust mites, mold spores, animal dander, cockroaches, pollen and irritants; pharmacological agents such as acetylsalicylic acid and beta-blockers; physical triggers, such as exercise and cold air; and physiologic factors such as stress, gastroesophageal reflux disease (GERD), upper respiratory tract infections, and rhinitis. Reference: Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma (GINA), 2009. Available from www.ginasthma.org.
- Among 93 nonsmoking asthmatics with moderate-to-severe followed for a minimum of five years (median follow-up 11 years), 56 (60.2%) experienced at least one severe exacerbation (median rate 0.10/year). Asthma patients who experienced frequent exacerbations had a significantly larger annual decline in FEV1 (median difference of 16.9 mL/year) than those who experienced infrequent exacerbations. Exacerbations, indicating intermittent periods of worsening airway inflammation, are associated with excess lung function decline in asthma. Reference: Bai TR, Vonk JM, Postma DS, Boezen HM. Severe exacerbations predict excess lung function decline in asthma. Eur Respir J 2007;30:452-456.
- The majority of patients with asthma have difficulty achieving adequate control of their disease, and a number of factors may contribute to suboptimal control. The first step in assessing suboptimal control is to ensure that a correct diagnosis of asthma has been made, by returning to the basics of history taking and physical examination, in conjunction with lung function measurement when appropriate. Practical barriers such as poor inhaler technique must be also addressed. Concomitant rhinitis, a common comorbidity of asthma can contribute to poor control. Smoking has also been identified as a cause of poor asthma control. Individual patient characteristics that could predict individual responses to asthma therapies also need to be addressed. Reference: Haughney J, Price D, Kaplan A, et al. Achieving asthma control in practice: understanding the reasons for poor control. Respir Med 2008;102:1681-1693.
- Current asthma therapies allow for optimism in terms of achieving relative patient satisfaction in asthma management. The goals of therapy as indicated above are the current targets for patients and include preventing further degeneration of lung function. Reference: Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma (GINA), 2009. Available from www.ginasthma.org.
- The available asthma medications, including their effects and common adverse effects, are summarized on this slide.1,2 Reference: 1. Lemière C, Bai T, Balter M, et al., on behalf of the Canadian Adult Consensus Group of the Canadian Thoracic Society. Adult Asthma Consensus Guidelines Update 2003. Can Respir J 2004;11(Suppl A):9A-18A. 2. Irwin RS, Richardson ND. Side effects with inhaled corticosteroids: the physician&apos;s perception. Chest 2006;130(1 Suppl):41S-53S.
- The available asthma medications, including their effects and common adverse effects, are summarized on this slide.1,2 Reference: 1. Lemière C, Bai T, Balter M, et al., on behalf of the Canadian Adult Consensus Group of the Canadian Thoracic Society. Adult Asthma Consensus Guidelines Update 2003. Can Respir J 2004;11(Suppl A):9A-18A. 2. Irwin RS, Richardson ND. Side effects with inhaled corticosteroids: the physician&apos;s perception. Chest 2006;130(1 Suppl):41S-53S.
- As mentioned, the latest recommendations for the management of asthma in Canada come from the Canadian Thoracic Society (CTS) Asthma Management Continuum 2010 Consensus Summary. The continuum itself is shown here. As shown, treatment begins, after confirmed diagnosis, with environmental control, education and provision of a written action plan. As mentioned, such action plans should outline recommended daily preventive management strategies to maintain control, when and how to adjust reliever and controller therapy in cases of loss of control, and clear instructions regarding when to seek urgent medical attention. In terms of pharmacotherapy, very mild/intermittent asthma may be treated with a prn SABA. ICS should be introduced early as initial maintenance treatment for asthma, even for patients with infrequent (&lt; 3 times per week) asthma symptoms. LTRAs are considered second-line monotherapy for mild asthma. If low-dose ICS does not provide adequate control, additional therapy should be considered. In children aged 6-11 years, the ICS should be increased to a moderate dose before an additional agent such as a LABA or LTRA is added. In patients aged 12 years or older, a LABA should be considered first as add-on therapy only in combination with an ICS. Increasing to a moderate dose of ICS or addition of an LTRA are third-line options. Theophylline may be considered as a fourth-line agent in adults. Severely uncontrolled asthma may require additional treatment with prednisone. Omalizumab may be considered in patients aged ≥ 12 years with poorly controlled atopic asthma despite high doses of ICS and appropriate add-on therapy, with or without prednisone. Symptom control, lung function tests, inhaler technique, adherence to treatment, exposure to asthma triggers in the environment, and the presence of comorbidities should be re-assessed at each visit and before altering the maintenance therapy. After achieving proper asthma control for at least a few weeks to months, the medication should be reduced to the minimum necessary to achieve adequate asthma control. Reference: Lougheed MD, Lemière C, Dell SD, et al. Canadian Thoracic Society Asthma Management Continuum--2010 Consensus Summary for children six years of age and over, and adults. Can Respir J 2010; 17(1):15-24.
- The World Health Organization reported in 1995 that there were more than 100 million people around the world with asthma. While a precise cause has yet to be determined for the steady rise in asthma prevalence, such a rise has been observed around the world and in Canada. In 2001 and 2009, Statistics Canada reported a prevalence of 8.4% for diagnosed asthma among those aged 12 and older. The disease is most common during childhood, and the prevalence among Canadian children was estimated to be at least 12% in the National Population Health Survey of 1996-1997. References: Statistics Canada. Asthma, by age group and sex. Available at: www40.statcan.ca. Accessed February 2011. Asthma Society of Canada. Asthma Facts & Statistics. Available at: www.asthma.ca. Accessed February 2011.
- The latest recommendations for the management of asthma in Canada come from the Canadian Thoracic Society (CTS) Asthma Management Continuum 2010 Consensus Summary. As stated in the CTS paper, “the primary goal of asthma management is to control the disease and, by so doing, prevent or minimize the risk of short- and long-term complications, morbidity and mortality.” The authors also stated that the existing Canadian criteria for acceptable levels of asthma control remain appropriate, and these are shown here. It is important to educate patients that this level of control for each of these criteria is generally achievable and should be the target of therapy. Also, it is important to ask patients about each of these criteria, in order to properly assess level of asthma control. Reference: Lougheed MD, Lemière C, Dell SD, et al. Canadian Thoracic Society Asthma Management Continuum--2010 Consensus Summary for children six years of age and over, and adults. Can Respir J 2010; 17(1):15-24.
- Results from the TRAC study, mentioned earlier, further highlight the gap between actual and perceived asthma control in Canada. As mentioned, only 47% of asthma patients in this survey were being adequately controlled according to the 1999 Canadian Asthma Consensus Guidelines’ symptom-based criteria. Despite this, 97% of patients said they thought their asthma was under control, while 88% of general practitioners and 90% of specialists in the same survey thought their patients were adequately controlled. The survey also found that only 39% of physicians surveyed based their treatment recommendations on the published guidelines most or all of the time (despite having a high level of awareness about the guidelines). Also of note, only 11% of patients had written action plans, and half of patients with action plans did not use the plans regularly. Reference: FitzGerald JM, Boulet LP, McIvor RA, et al. Asthma control in Canada remains suboptimal: the Reality of Asthma Control (TRAC) study. Can Respir J 2006; 13(5):253-9.
- There are several patient-related barriers to compliance with prescribed asthma therapy, beginning with the facts that most patients do not feel a need for daily maintenance therapy during periods when they are asymptomatic, and many believe they know when they need to take their asthma medications. Furthermore, most patients rely on SABAs because these work quickly to alleviate symptoms when they do occur. Finally, many patients do not take their maintenance therapy as prescribed because they do not know or believe that poor control of their asthma will result in important future risks.
- In Canada, three products are available which combine an ICS and a LABA in a single inhaler (at various fixed doses). These include a fluticasone + salmeterol combination, a budesonide + formoterol combination, and the most recently made available mometasone + formoterol combination. Compared to ICS + LABA combination therapy in which each agent is taken via a separate inhaler, single-inhaler combination therapy can have a number of important benefits. The regimen is easier and more convenient for patients to follow, as it requires the use of only one device, which can promote enhanced compliance. As well, this approach avoids the risk that patients might choose to use their prescribed LABA as monotherapy. References: Advair® Product Monograph. GlaxoSmithKline Inc., July 2010. Symbicort® Product Monograph. AstraZeneca Canada Inc., December 2010. ZenhaleTM Product Monograph. Merck Canada Inc., January 2011.
- Factors that influence the efficacy and safety of available ICS agents include physiochemical properties that affect pharmacologic, pharmacokinetic, and pharmacodynamic profiles. Low systemic bioavailability and high relative binding affinity for the glucocorticoid receptor are properties that allow for a favorable efficacy and tolerability profile of a given ICS. References: Rossi GA, Cerasoli F, Cazzola M. Safety of inhaled corticosteroids: room for improvement. Pulm Pharmacol Ther 2007; 20(1):23-35. Bousquet J. Mometasone furoate: an effective anti-inflammatory with a well-defined safety and tolerability profile in the treatment of asthma. Int J Clin Pract 2009; 63(5):806-19.
- Reference: Lougheed MD, et al. Canadian Thoracic Society 2012 guideline update: diagnosis and management of asthma in preschoolers, children and adults. Respir J. 2012;19:127-64.
- Rapidity of onset of action is an important characteristic of asthma therapy that can have meaningful impact for patients and can distinguish agents from each other. This randomized, active-controlled, multicentre, non-inferiority trial comparing the effects of mometasone + formoterol combination to those of fluticasone + salmeterol (both in single-inhaler formulations) included 722 subjects aged ≥ 12 years previously treated with medium-dose ICS alone or in combination with a LABA. The primary endpoint was change from baseline in area under the curve (AUC) in FEV1 0-12 hours post-dose. Key secondary endpoints included onset of action, defined as change from baseline in FEV1 at 5 minutes post-dose on day 1. Mometasone + formoterol was found to be non-inferior to fluticasone + salmeterol in terms of mean FEV1 AUC (0-12 hours) at endpoint, but was found to have a significantly faster onset of action (as shown on this slide). Reference: Bernstein DI, Murphy KR, Nolte H. Non-inferiority efficacy comparison of mometasone furoate/formoterol versus fluticasone propionate/salmeterol combination therapies in subjects with persistent asthma. Allergy Asthma Clin Immunol 2010; 6(Suppl 2):P33.
- Asthma treatment can be tailored for individual patients in order to optimize compliance, efficacy and safety/tolerability. Patients’ preferences should be discussed, and their ability to use potential treatment devices assessed. In those who express fears about ICS use, risks should be properly discussed but steroid alternatives for maintenance should also be evaluated. Patients should also be asked about their need/desire for rapid onset of action, and treatment should be selected accordingly. Finally, choosing an ICS with the lowest bioavailability and associated with the lowest risk of adverse effects will increase the likelihood of patient satisfaction and therefore of treatment success.
- These investigators used the Saskatchewan Health databases to form a population-based cohort of subjects aged 5-44 years who were using anti-asthma drugs during the period from 1975 through 1991, and conducted a nested case-control study in which subjects who died due to asthma were matched with controls within the cohort. The cohort consisted of 30,569 subjects; 562 deaths occurred, of which 77 were classified as asthma-related. The mean number of ICS canisters used per year was 1.18 among patients who died, and 1.57 among controls. On the basis of a continuous dose-response analysis, the investigators calculated that the rate of death from asthma decreased by 21% with each additional canister of ICS used in the previous year (adjusted rate ratio 0.79; 95% CI 0.65-0.97). The fitted dose-response curve for the one-year period is shown on this slide. The rate of death from asthma among ICS users vs. non-users was reduced by about 50% with the use of &gt; 6 canisters per year. The figure also suggests that sporadic use of ICS (&lt; 4 canisters per year) may be associated with higher rates of death from asthma. Reference: Suissa S, Ernst P, Benayoun S, et al. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med 2000; 343(5):332-6.
- Non-adherence to asthma therapy can be thought of as two types of behaviour – intentional and non-intentional. Intentional non-adherence occurs when the patient decides not to take the medication or to take it in a way that differs from the recommendations. The patient may lack motivation to take the medication, have doubts about their need for medication, or have concerns about potential adverse effects. Unintentional non-adherence occurs when the patient is prevented from taking the medication as prescribed, by factors beyond their control, such as a lack of capacity or resources, including poor comprehension (eg, of the drug regimen)or language barriers, and practical barriers, such as a physical inability to manage the medication (eg, poor inhaler technique) or poor recall of the consultation. In order to improve adherence to asthma treatments, physicians must be able to counter patient doubts and address their concerns. This can be difficult if physicians avoid the subject with their patients, lack clear, easy methods of addressing barriers to adherence, or have a perception that little can be done to improve adherence. Reference: Horne R. Compliance, adherence, and concordance: implications for asthma treatment. Chest 2006;130(1 Suppl):65S-72S.
- Education is an important factor in ensuring patient adherence to asthma medications. When educating patients, physicians should ensure that they are using language that is appropriate for the patient, and should write down any important information. All patients should be provided with an written asthma action plan. When necessary, patients may be referred to an asthma educator.1 Patients should be encouraged to self-monitor their condition. The physician should ensure that the patient is using proper inhaler techniques to ensure adherence. Combination therapies may be recommended to improve compliance.2 References: 1. National Heart, Lung, and Blood Institute National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma Full Report 2007. NIH Publication No. 07-4051. Bethesda, MD: National Heart, Lung, and Blood Institute, August 28, 2007. 2. Stoloff SW, Stempel DA, Meyer J, Stanford RH, Carranza Rosenzweig JR. Improved refill persistence with fluticasone propionate and salmeterol in a single inhaler compared with other controller therapies. J Allergy Clin Immunol 2004;113:245-251.
