4. Transitioning to home setting
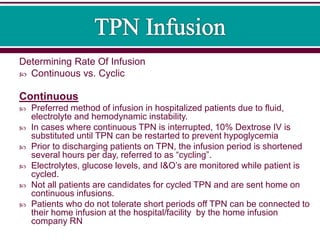
- 1. Determining Rate Of Infusion Continuous vs. Cyclic Continuous Preferred method of infusion in hospitalized patients due to fluid, electrolyte and hemodynamic instability. In cases where continuous TPN is interrupted, 10% Dextrose IV is substituted until TPN can be restarted to prevent hypoglycemia Prior to discharging patients on TPN, the infusion period is shortened several hours per day, referred to as “cycling”. Electrolytes, glucose levels, and I&O’s are monitored while patient is cycled. Not all patients are candidates for cycled TPN and are sent home on continuous infusions. Patients who do not tolerate short periods off TPN can be connected to their home infusion at the hospital/facility by the home infusion company RN
- 2. Cyclic Preferred method for the home TPN patient Infused over 8-16 hours rather than 24. Generally infused at night during sleep to allow patient freedom from the pump during the day, improving quality of life. Allows for increased mobility, which maintains somatic muscle mass Prevention or treatment of hepatotoxicities induced by continuous PN Improved physiological hormonal responses and stimulation of appetite Prevention or treatment of fatty acid deficiency in patients receiving fat-free PN Reduced insulin needs during PN-free periods allow for lipolysis
- 3. The main goal of home TPN therapy is to provide adequate nutrition with minimal to no complications. This will start in the hospital with a pre-discharge educational session if possible. Working with the discharge planner, the patient needs to be evaluated for the following: o The patient or his caregiver must be willing to participate in the program and the basic TPN procedures in the home. o Does the patient or caregiver have adequate manual dexterity and vision to manage the infusion pump and additives for TPN? o Does the patient have long-term IV catheter such as a PICC line or implanted port? Once criteria have been met, services with home health and home infusion agencies are coordinated and the patient is ready for discharge. The home care nurse will then continue education on the initial home visit and subsequent visits as needed.
- 4. As a provider of home nursing, your goals will include: Educating the patient and caregiver to enable them to become independent in TPN administration. Education related to possible complications of TPN therapy Nursing assessment: A thorough patient assessment is necessary including: o Physical assessment of all body systems – this will give baseline data to compare to. o Emotional and Psychosocial assessment- there can be alterations in body image related to having the IV catheter and the attachment to equipment for TPN administration. There also can be alterations in lifestyle. With children on TPN, normal developmental stages can be interfered with. o Support system assessment – assess who will be the primary caregiver and evaluate if this person will be able to master the procedures necessary. Involve the patient in their own care as much as possible o Home assessment – the home environment is extremely important. Do they have electricity, running water and a phone? If not, what arrangements have been made if problems arise.
- 5. Educational needs should be tailored to each individual patient. Verbal and written instructions need to be given so the patient has something to refer to when the nurse is not there. Also during education, there should be adequate return demonstrations given by the patient or caregiver. Further education should be evaluated on the level of comprehension. Some of the points you will want to cover: o What is TPN? o How is it administered? o What monitoring should be done? o What complications might arise and how can they be avoided? o What to do in an emergency?
- 6. What is TPN? TPN (Total Parenteral Nutrition) is an intravenous solution that is used to provide nutrition for people who cannot or should not get their nutrition by eating. The TPN solution usually contains sugars for energy, amino acids to maintain muscle mass, electrolytes to maintain organ function, trace elements and water. Some TPN mixtures also may contain lipids, or essential fats. Some patients may add certain medicines such as multivitamins or Pepcid® to their TPN. TPN is usually infused between 10-24 hours per day. It may be used every day or only a few days per week according to the doctor’s orders. It will infuse slowly through the IV line. If it is not continuous it is usually preferred to infuse overnight allowing more freedom during the day.
- 7. How is it administered? TPN is always infused by an electronic infusion pump. The home patient will be using an ambulatory electronic pump. Educate the patient regarding the pump, power sources, program, attaching the tubing, flushing the IV catheter, connecting the TPN and placing the TPN bag and pump into the backpack. Have printed instructions for the patient readily available for the patient and caregiver to refer to when the nurse is not there.
- 8. Preparation of Solution in the home: The bag of TPN should be taken out of the refrigerator anywhere from 2-8 hours in advance to bring it to room temperature. The solution should not hang for more than 24 hours after the bag has been spiked. Each bag, before being used should be thoroughly inspected. The appearance of the TPN solution should be clear without precipitates. The TPN bag with lipids should be inspected for frothiness, separation or an oily appearance. Make sure to instruct the patient that the TPN bag should never be microwaved to bring it to room temperature. If it is necessary to warm the bag, it can be placed in the sink with tepid water. The bag should never be placed in direct sunlight.
- 9. Storage: The TPN solution will need to be stored in a clean area of the refrigerator. The supplies will need stored in a clean dry area away from children and pets. The tubing for TPN will have an in-line filter. o A 0.22 micron filter should be used for the 2-in-1 Solutions (clear) o A 1.2 micron filter should be used if lipids are being administered.
- 10. The patient will need instructed on using aseptic technique. Start by educating in the proper hand washing technique. o Use warm water to wet hands o Apply soap and rub hands together vigorously for a least 15-20 seconds o Rinse hands, avoiding splashing o Keep hands down so that run-off will go into the sink and not down the arm o Dry hands well with a disposable towel o Use the towel to turn off the faucet o Discard towel in the appropriate container Instruct the patient on how to prepare a clean and safe work area. o The work area should be out of the family traffic pattern. o The work surface should be one that can be repeatedly cleaned. The area should be clear of clutter. o The patient or caregiver should never smoke while preparing the solution. o Keep pets and children out of the area when preparing the TPN solution.
- 11. TPN preparation: Instruct the patient on preparing any additives using aseptic technique. o Have them clean injection port of TPN bag with new alcohol wipe vigorously for 15 seconds before injecting each additive into bag. After adding any medications and vitamins to the bag, if ordered, instruct the patient to gently rock the bag gently back and forth to evenly distribute the medication throughout the TPN solution. o The bag of TPN should never be shaken. Instruct the patient in the proper way to spike the bag of TPN by removing the cover from spike on tubing and inserting the spike into TPN bag using a pushing twisting motion. o Make sure they are aware that if the spike touches anything, a new tubing will need to be used.
- 12. Once the TPN bag is spiked, the patient will need educated in the ambulatory infusion pump. Pump instructions: Instruct in the basic functions of the ambulatory pump: Power source – importance of using a power pack versus just a battery How to attach tubing to the ambulatory pump Priming tubing – trouble shoot how to remove air from tubing if bubbles should appear. Loading pump and TPN bag into a backpack for portability Instruct the patient on preparing flush syringes and how to appropriately flush the IV catheter: o Remove any air from syringe. o Recap until ready to flush the catheter. o Scrub the cap on the catheter vigorously for 15 seconds any time the cap will be used, either to flush or to connect tubing. o Flush the catheter with Normal Saline. o If any resistance is felt, do not force flush.
- 13. After scrubbing the cap again vigorously for 15 seconds, attach the TPN tubing to the cap of the catheter. Instruct the patient on starting the pump. o If there is a taper up mode ordered, instruct the patient that the pump will start slow then ramp up to a “plateau” rate. o If there is a taper down mode ordered advise them that the TPN will slow down over the last period of the infusion. Most pumps will be programmed to enter into a KVO rate once the actual infusion of TPN is completed. The patient will also need to be instructed in how to o discontinue the TPN o discard the bag and tubing o do their final flushing with Normal Saline and Heparin (if indicated).
- 14. The home care patient will need taught what to monitor while receiving TPN therapy. Even though every doctor may have specific items for the patient to monitor, the most common are the following: Weight – the patient should report any fluctuation in their weight as this could indicate signs that they are not getting enough calories in their solution if they notice a weight decrease. A weight gain could indicate fluid retention. Intake and Output – if the patient has any oral intake, this should be recorded. Also if they notice an increase in urination, report this also. Quite a few patients on TPN at home will have ostomies. Have them monitor for an increase in ostomy output. Temperature – normally if the patient experiences a temperature of 100.5F, they should notify the nurse and/or physician.
- 15. Signs of infection – this would include general signs of infection along with signs or symptoms of IV catheter infections. Make them alert to monitor for temperature elevations, chills, fever, drainage (if they have an incision) or change in the drainage indicating infection, also drainage at the IV catheter site. IV catheter site – the patient needs to monitor their IV catheter site daily for tenderness, redness and drainage – all signs of IV line infection. Also if they have difficulty with flushing or experience any “odd” sensation when flushing their catheter (many patients report it as an “instant flu like sensation”) they should notify their home care nurse or doctor immediately. Urine glucose – many patients are sent home from the hospital with urine glucose test strips. Instruct the patient in how to use these strips and what the normal range of urine glucose should be. Encourage your patients to get a notebook to record all of these items and to have it handy so that you can assess the results on your visits. They should also take these notes to the doctor’s appointments with
- 16. Teach your patients what complications are possible and what they should be alert to. Along with their regular monitoring, they should know the signs of catheter complications which would include: o What to do if they should experience difficulty flushing their catheter o Signs and symptoms of Central Line Infections as previously mentioned o Sign and symptoms of hyperglycemia and hypoglycemia o Signs and symptoms of dehydration and fluid overload. o What to do in an emergency should arise: • If they are experiencing chest pain or shortness of breath, call 911
- 17. When to call the home care nurse: o If there is bleeding at the catheter, have them call the home care nurse immediately o If there is damaged to the IV line or the IV line is cut in any way or “falls out” call the home care nurse or doctor immediately o If they are experiencing a problem with the infusion pump – call the home care nurse or the infusion company for assistance. o If they are experiencing any difficulty in preparation of the TPN or the infusion of the TPN call the home care nurse for assistance or direction.