TURP
- 1. TEMPLATE DESIGN © 2007
www.PosterPresentations.com
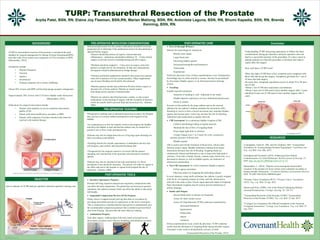
TURP: Transurethral Resection of the Prostate
Arpita Patel, BSN, RN, Elaine Joy Fleeman, BSN,RN, Marian Mationg, BSN, RN, Antonieta Laguna, BSN, RN, Bhumi Kapadia, BSN, RN, Brenda
Kenning, BSN, RN.
BACKGROUND
•TURP or transurethral resection of the prostate is considered the gold
standard for surgical management for Benign Prostate Hyperplasia(BPH)
and other male lower urinary tract symptoms (LUTS) secondary to BPH.
(Mamoulakis, 2014).
•Symptoms include:
• Daytime frequency
• Nocturia
• urgency,
• Incontinence
• Voiding symptoms (slow stream, dribbling)
•About 50% of men with BPH will develop benign prostatic enlargement.
•Approximately 50% of men with LUTS have bladder outlet obstruction.
(Mamoulakis, 2014)
•Indications for surgical intervention include:
• Patients with moderate-to-severe symptoms that reduces
quality of life
• Patient with renal insufficiency secondary to BPH
• Patients with symptoms of urinary retention and cannot be
resolved with medical therapy.
OBJECTIVE
PRE-OPERATIVE MEDICATION CONSIDERATIONS
Both prescription and over-the-counter medications should be reviewed
preoperatively to determine if the medications need to be discontinued or
adjusted before surgery.
•Patients should discontinue all aspirin, nonsteroidal anti-
inflammatory medication and platelet inhibitors 10 – 14 days before
surgery to prevent excessive bleeding during and after surgery.
•Warfarin should be stopped 4 – 5 days prior to surgery unless the
patient is at high risk for clot formation. In that case subcutaneous
enoxaparin would be administered as bridge therapy.
•Vitamins and herbal supplements should be discussed since patients
often fail to mention over-the-counter products. Many supplements
can increase bleeding and should be discontinued.
•Diabetic patients should stop metformin 48 hours before surgery to
decrease risk of lactic acidosis. Patients on insulin require
individualized pre-operative treatment plans.
•Patients are asked to take blood pressure, cardiac, or anti-seizure
medications on the morning of surgery with the exception of diuretics
which are usually held to prevent fluid and electrolyte loss. (Starnes,
2006)
PRE-OPERATIVE TEACHING
•Preoperative teaching such as education about the procedure, the hospital
stay, and use of a urinary catheter postoperative and irrigation of the
bladder.
•An explanation as to how the catheter works to decompress the bladder
and allow the bladder to heal and that the catheter may be needed for a
period of one to three weeks postoperatively.
•Patients may also be taught about the use of leg bags upon discharge for
their convenience and mobility.
•Teaching should also include expectations of ambulation and how diet
will progress, pain control, and expected discharge date.
• Preoperatively the surgical consent is reviewed with the patient
including risks and hazards of the procedure and alternative treatment
options.
•Patients may also be informed of the risks and hazards of a blood
transfusion if one should be necessary. The permit will either be signed in
the office and sent to the hospital or signed at the hospital the day of
admission. (Starnes, 2006)
POST-OPERATIVE TOOLS
Incentive Spirometry Purpose:
Promote full lung expansion and prevent respiratory complications that
can affect the body temperature. The patient has not been given general
anesthesia, but sedation instead, which can affect the ability to take deep
full breaths.
Sequential Compression Devices (SCD) Purpose:
Plastic sleeves wrapped around each leg that aides in circulation by
providing intermittent periods of compression on the lower extremities.
This is connected to a machine that has been preset to automatically give
the recommended compression pressure that is needed to prevent blood
clots from forming. This provides the same effect as walking.
Ambulation Purpose:
Soon after surgery, walking helps with early return of normal bowel
movements, promotes more effective breathing, and mobilizes secretion.
POST-OPERATIVE CARE
First 24 through 48 hours:
Monitor for hemorrhage by looking for
Bloody urine output
Large blood clots
Increasing bladder spasms
Decreased hemoglobin and hematocrit
Tachycardia
Hypotension
Notify the physician if any of these manifestations occur. Postoperative
hemorrhage may be either arterial or venous, and may be precipitated
by movement, bladder spasms, or an obstructed urinary drainage
system.
Teaching:
Explain expected sensations
Sensation of needing to void - Important to not strain!
Bladder Spasms experiences as lower abdominal pain/pressure
Desire to urinate
Pressure on the urethra by the large catheter and on the internal
sphincter by the catheter’s balloon stimulate the micturition reflex.
Straining to void or to have a bowel movement may stimulate bladder
spasms and increase pain; it also may increase the risk for bleeding.
Administer pain medications at regular intervals.
CBI Assessment: In a continuous bladder irrigation (CBI)
Catheter and drainage tubing at regular intervals
Maintain the rate of flow of irrigating fluids
Keep output light pink or colorless
Urinary Output every 1 to 2 hours for color, consistency,
amount, presence of blood clots
Bladder spasms
CBI is used to prevent the formation of blood clots, which could
obstruct urinary output. Bladder distention resulting from output
obstruction increases the risk of bleeding. Irrigating fluids are
continuously infused and drained at a rate to keep urine light pink or
colorless. Urine that is frankly bloody, contains many blood clots, or is
decreased in amount, as well as bladder spasms, are indicators of
obstruction and bleeding.
Non CBI Assessment: In a Non continuous bladder irrigation
Follow agency procedure
Physician orders for irrigating the indwelling catheter
In most instances, using sterile technique, the catheter is gently irrigated
with 50 mL of irrigating solution at a time, until the obstruction is
relieved or the urine is clear. Ensure equal input and output of irrigating
fluid. Intermittent irrigation may be used to prevent obstruction of
urinary drainage.
Intake and Output:
Record fluids taken in and put out frequently
Assess for fluid volume excess
Assess for Hyponatremia (TURP syndrome) manifested by
decreased hematocrit
hypertension
bradycardia
nausea
confusion
If these manifestations occur, notify the physician. TURP syndrome
results from the absorption of irrigating fluids during and after surgery.
Untreated, it may result in dysrhythmias, seizures, or both.
(Transurethral Resection of the Prostate, 2015)
Conclusion
RESOURCES
Cunningham, Glenn R., MD, and Dov Kadmon, MD. "Transurethral
Procedures for Treating Benign Prostatic Hyperplasia." UpToDate.com.
N.p., n.d. Web. Feb.-Mar. 2015.
Farrington and Townsend. (2014). Enhancing Nurse-Patient
Communication: A Critical Reflection. British Journal of Nursing, 23.
DOI: http://dx.org/10.12968/bjon.2014.23.14.771.
Mamoulakis, C. (2014). “Bipolar versus monopolar transurethral
resection of the prostate for lower urinary tract symptoms secondary to
benign prostatic obstruction..” Cochrane Database of Systematic Reviews.
DOI: 10.1002/14651858.CD009629.pub3
"Prostate Cancer Foundation (PCF)." Prostate Cancer Foundation
(PCF). N.p., n.d. Web. 25 Apr. 2015.
Starnes and Sims. (2006). Care of the Patient Undergoing Robotic-
Assisted Prostatectomy. Urologic Nursing, 26, 129-137.
"Transurethral Resection of the Prostate (TURP)." Transurethral
Resection of the Prostate (TURP). N.p., n.d. Web. 25 Apr. 2015.
"Urology Care Foundation The Official Foundation of the American
Urological Association." Urology Care Foundation. N.p., n.d. Web. 25
Apr. 2015.
Aim to educate on TURP and pre-operative and post-operative nursing care.
Understanding TURP and giving importance to follow the basic
considerations during pre-operative and post-operative care can
lead to a successful outcome of the procedure. It is also a must to
educate patients on what this procedure is all about and what to
expect after the surgery.
How well does a TURP work?
•Men who had a TURP have a low symptom score compared with
those who did not go the surgery. Symptoms get better for 7 out of
10 men who had surgery.
•In some men, retrograde ejaculation occurs in about 25 to 99 men
out of 100.
•About 1 out of 100 men experiences incontinence.
•About 2 men out of 100 need to have another surgery after 3 years,
and about 8 men out of 100 need to have another surgery after 5
years.
(Cunningham, 2015)