Wireless Health
- 1. Social innovation: incentives from “push” to people Last mile delivery in health care and patient empowerment through technology: the case of “Telecommunication for Health” Article by Roberto Tapia-Conye (pictured), Director-General, Carso Health Institute – Carlos Slim Foundation, Mexico, and Rodrigo Saucedo, Researcher, Carso Health Institute – Carlos Slim Foundation, Mexico he epidemiologic profile of the population in Latin therefore limits the success of any treatment. It is necessary T America has been continuously changing for the last 30 years. Noncommunicable diseases have emerged as the main burden of national health systems, shifting the to shift from acute discrete interventions to preventive continuous care, integrating hospital-based interventions with community participation. pattern from the youngest population to the eldest e.g. The second major turnaround refers to the degree of diabetes, cardiovascular diseases and obesity. The average involvement of patients with respect to their own disease. It mortality rate from diabetes mellitus (DM) in Latin America1 is estimated that only 50% of patients comply with their is 35 with the extreme cases of Mexico (83.1) and Uruguay physicians’ prescription irrespective of the disease or their (14)2,3. The International Diabetes Federation estimated that age10. Treatment of chronic diseases requires an intake of in 2007 there were 20.7 million people with DM and several doses of medication on a daily basis, and there is an impaired glucose tolerance whereas in 2025 there will be inverse linear relation between the number of doses and the 41.2 miliion people; this is a 99.2% growth rate. In fact, levels of compliance11. Additionally, people discontinue their WHO estimates that in 2030 nine out of the ten main causes medicine intake within a period of time; patients suffering of death will be attributable to noncommunicable diseases4. from hypertension generally discontinue their medication Research into causes of this increase does not point a linear intake in 90 days12. On the other hand, the ageing of the cause. A sedentary lifestyle and bad diet have been pointed population plays a key role. In Latin America life expectancy to as the main driving forces5. On the other hand, cognitive at birth has increased from an average 61.1 years for the and motivation factors play a key role too6. 1970–1975 period to 73.8 in 2005–2010, and it will Nevertheless, some communicable diseases are present in increase to 77.3 years in 2025–2030, as Figure 1 shows13. people’s entire lives such as HIV/AIDS. The number of people This scenario is immersed in a context of globalization and living with HIV/AIDS in Latin America has grown from 1.3 immigration, which limits the capacity of national health million in 2000 to 1.6 million in 2007; a 20.9% growth systems to provide continuous and sustained health rate7. Thus, the analysis is now between acute and chronic treatment. Health systems must be able to provide mobile diseases8. The centre of the analysis in public health is now on morbidity rather than on mortality9. At the Carso Health Institute, an initiative of the Carlos Slim Foundation, we argue 80 that chronic diseases are conditions of life and an effective 78 76 strategy must integrate health services through multiple 74 bidirectional channels of communication so that the patient, 72 70 the physician and the health system can continuously interact. 68 For the strategy to be effective, we believe that a major 66 64 turnaround is required at two different levels: at the health 62 system-level and at the patient-level. First, there must be a 60 1970-1975 1975-1980 1980-1985 1985-1990 1990-1995 1995-2000 2000-2005 2005-2010 2010-2015 2015-2020 2020-2025 2025-2030 change in the way traditional health services are provided. The current system is hospital-centric, it works on a one-to- one interaction and it is limited in the time of interaction between the physician and the patient. Patients are still Source: UN Population Division passive recipients of vertical and reparative interventions. Figure 1: Life expectancy at birth in Latin America, 1970–2030 This limits follow-up of the patient’s health conditions and 10 Global Forum Update on Research for Health Volume 6
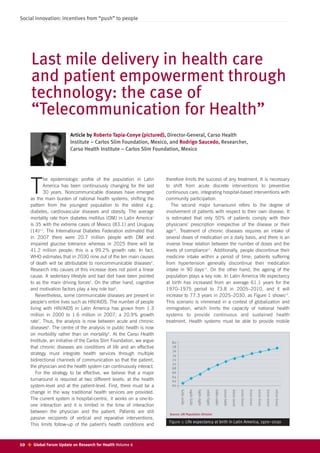
- 2. Social innovation: incentives from “push” to people health care, either with mobile health units or through 400 patients’ remote management. 350 As a consequence, complications related to disease arise, 300 Millions increasing the direct and indirect costs associated to it and 250 driving national health costs in both developed and 200 developing countries. In the US, for diabetes alone, the total 150 cost of treatment and complications was 132 billion in 100 2002, and it will grow at an annual rate of 3.3% to 192 50 billion in 202014. In the UK, National Health Service 0 expenditure will grow at an average real rate of 4.2 to 5.1% 1990 2000 2001 2002 2003 2004 2005 2006 2007 2008 by 202215. Turning to Latin America, the cost of treatment for diabetes was US$ 7 667 million in 2007 and it will grow at Fixed phone lines Mobile phone users an annual rate of 3.8% to US$ 28 080 million in 202516. Source: ITU 2008 Thus, governments are now struggling to find a new way Figure 2: Number of fixed lines and mobile phone users in Latin America, 1999–2008 to approach chronic diseases. We believe that technology is the agent of change for the current paradigm in the delivery of health services. In Latin America the use of technology is 200 180 increasingly becoming a part of people’s everyday lives. In 160 1999 there were 62.7 million fixed phone lines in Latin Millions 140 America, increasing to 99.4 in 2008. With respect to mobile 120 phone users, there were 19 million in 1999, and it 100 dramatically increased up to 374.9 million in 2008 for an 80 60 average of 80 mobile phone users per 100 inhabitants 40 (Figure 2). Some factors explain this. Firstly, mobile phones 20 require wireless infrastructure only. Secondly, mobile phones 0 can be purchased without any credit conditions. 1990 2000 2001 2002 2003 2004 2005 2006 2007 2008 With respect to personal computers (PCs), in 1999 there Number of PCs Internet users were 18.6 million PCs in Latin America, increasing to almost Source: ITU 2008 87 million in 2008, a growth rate of 368% in only 9 years. Figure 3: Number of PCs and Internet users in Latin America, Nevertheless, the trend is much steeper for Internet users. 1999–2008 There were 9.97 million Internet users in 1999, increasing to 183.5 million in 2008, 17.4 times the number of users found out that 93% of SMS-based interventions delivered in 1999. Two possible factors explain this. Firstly, a single PC positive behaviour changes22. He found that dialogue may be used by more than one person in a household; initiation, continuous interactivity and customization of SMS secondly, the number of public Internet kiosks has risen were highly effective; this is consistent with a 2003 WHO dramatically since 2000, as is the case in Mexico17. study in which motivation and behavioural skills were The use of technology to deliver health services is now a described as the main drivers of compliance23. Furthermore, current practice. Scholars and project designers have even mobile phones were not used for information sharing only. created some terms to define them: eHealth, telemedicine, Some studies have demonstrated a decline of between 33 telehealth or mHealthi. Furthermore, there has been a large and 50% in missed appointments given the SMS reminders24. movement about the benefits of it; yet only a few studies Nevertheless, SMS may not be the most effective way to provide solid evidence to support this argument. address chronic diseases given that the elderly group uses Some systematic reviews have been performed but the phone a lot less frequently compared to younger groups, unfortunately some methodological limitations in the projects especially in developing countries, where the use of mobile evaluated impede their replication and escalation18,19,20. phones is mainly by adolescents and young adults. Furthermore, almost all mHealth projects are designed to Therefore, an integral strategy must consider the use of the improve health system efficiency, or to improve efficiency in Internet, the fixed phone line and community-based the way physicians allocate their time. Finally, none of the participation. As some studies have proved, phone-based studies found in the literature refer to projects implemented interventions have demonstrated positive results among in Latin America. To our knowledge, those projects are only persons with low socioeconomic status19. found in grey literature, i.e. research and technical papers, With this scenario, at the Carso Health Institute we created government reports, surveys, etc21. Telecommunication for Health in which the mobile phone, Nevertheless, the very few studies that performed the Internet and the fixed phone converge in a unique controlled studies or clinical trials provide interesting insights technological platform created to provide strategic integral worth a deeper analysis. Within all the technologies the most bottom-up services to the individual and achieve last mile studied is the mobile phone. In a recent study, Fjeldsoe delivery. If users have access to multiple communication platforms, we expect an increase in the extent to which users i Hereafter we will refer to this movement as mHealth. are informed and willing to treat and control their disease. Global Forum Update on Research for Health Volume 6 11
- 3. Social innovation: incentives from “push” to people Key messages Furthermore, users can test themselves at home, and then send the results through the channel that is most convenient to them, either at home through the 01-800 telephone Chronic diseases are conditions of life and an number, at their personalized website or through their mobile effective strategy must integrate health services phones. For us, mHealth does not refer to the use of mobile through multiple bidirectional channels of devices to provide a health service; it refers to mobilizing the communications, setting the patient at the centre health resources to wherever the user goes, literally following of the analysis. him and enhancing the probability of a treatment succeeding. It is necessary to change the current paradigm of With Telecommunication for Health it is the user that provision of health services, from acute discrete demands results from the health system, setting a new interventions to continuous preventive care, bidirectional channel of communication and empowering him integrating hospital-based interventions into a to take further action. These innovations are available even in nonspatial environment. the poorest communities. The current view of patients as passive recipients of To our knowledge, this is the first scalable project that uses care must be shifted to a full partnership in health a bottom-up approach that places the person in the centre of care, where patients are informed, are aware of their the strategy. Some studies have demonstrated that remote diseases, and are empowered to take further action management of chronic diseases decreases the number of to control and manage their health. hospitalizations by up to 32%, the number of emergency room visits by 40%, the number of hospital admissions by 63% and the number of hospital bed days of care by 60%25. appointed a member of the Influenza Global Action Plan Advisory Shifting the current paradigm means changing the focus of Group. He is an active member of the Mexican Academy of care, from discrete services to integral continuous services Sciences, the Mexican Academy of Medicine, the Mexican that place prevention as the main approach, considering the Academy of Surgery and the Mexican Public Health Society, which community as a strategic player in addressing health needs. he chaired in 1997. Roberto Tapia-Conyer holds a Master of Public It also means setting a turnaround in the location of care, Health degree from Harvard University and a Doctorate in Sciences from hospital-based interventions to nonspatial interventions, conferred by the University of Mexico. where health care is present everywhere. Finally, it implies shifting the balance of responsibility, transforming the Rodrigo Saucedo is a researcher at the Carso Health Institute. traditional view in which patients are passive recipients of He is actively involved in the design of technology-intensive health care towards a full partnership in their management of projects, as well as the strategic positioning of the various health health. It is when patients are aware and empowered to act projects. He has been a consultant for the Mexican Ministry of that the strategy may succeed. J Health, the Mexican Ministry of Social Development and the Centre for Research and Development in Economics in Public Roberto Tapia-Conyer is the Director-General of the Carso Health Finance, Financial Protection in Health and sustained public Institute. Prior to that, he served as the Vice-Minister of Prevention policies. Rodrigo Saucedo holds a Bachelor in Economics from and Health Promotion for 12 years. He also chaired the Strategic CIDE in Mexico, specializing in Public Finance and has taken Technical Advisory Group of WHO’s TB Programme and has been courses in Management and Corporate Finance. References 1. Latin America refers to Argentina, Belize, Bolivia, Brazil, Chile, Colombia, 13. 2008 World Population Prospects. Geneva, UN Population Division, Costa Rica, Ecuador, El Salvador, Guatemala, Honduras, Mexico, 2009. http://esa.un.org/unpp/index.asp (last accessed 3 August 2009). Nicaragua, Panama, Paraguay, Peru, Uruguay and Venezuela. 14. Rifat A et al. Use of mobile technologies to enhance control of type 1 2. There was no information for Belize, Bolivia and Honduras. diabetes in young people: economic evaluation. In: The role of mobile 3. Basic Health Indicators 2008. Geneva, World Health Organization, 2009. phones in increasing accessibility and efficiency in healthcare. Vodafone 4. World Health Statistics 2008. France, World Health Organization, 2008. Policy Paper Series 4, 2006. 5. Mobile health: the potential of mobile telephony to bring health care to the 15. Chauhan D et al. The upward trend in healthcare spend. In: The role of majority. Washington, Inter-American Development Bank, 2009. mobile phones in increasing accessibility and efficiency in healthcare. 6. Tackling obesities: future choices – project report. Scotland, UK Vodafone Policy Paper Series 4, 2006. Government, 2007. 16. Diabetes Atlas, 3rd ed. Brussels, International Diabetes Federation, 2008. 7. Report on the global AIDS epidemic. Geneva, UNAIDS/WHO, 2008. 17. World Telecommunication/ICT Indicators Database online. Geneva, 8. Frenk J. Reinventing primary health care: the need for systems integration. International Telecommunications Union. http://www.itu.int/ITU-D/ict/ (last Lancet, 2009, 374: 170–173. accessed 3 August 2009). 9. Frenk J et al. La transición epidemiológica en América Latina. Bol. of 18. Whitten P Systematic review of cost-effectiveness studies of telemedicine . Sanit Panam 1991, 111(6):485–496. interventions. British Medical Journal, 2002, 324:1434–1437. 10. Bloom B. Daily regimen and compliance with treatment. British Medical 19. Krishna S et al. Healthcare via cell phones: a systematic review. Journal 2001, 323:647. Telemedicine and e-Health, 2009, 15(3):231–240. 11. Bloom B. Direct medical costs of disease and gastrointestinal side effects 20. Guide to regional good practice: eHealth. Brussels, IANIS, 2007. during treatment for arthritis. American Journal of Medicine, 1988, 21. Two projects are the Andean e-Health Initiative 84(2a):20-24. (www.andeanehealthhomestead.com) and the Cell PREVEN project in 12. Bloom B. 2001, ídem. Peru (www.perupreven.org). 12 Global Forum Update on Research for Health Volume 6
- 4. Social innovation: incentives from “push” to people References continued 22. Fjeldsoe et al. Behavior change interventions delivered by mobile 24. Rifat A. A review of the characteristics and benefits of SMS in delivering telephone Short Message Service. American Journal of Preventive healthcare. In: Vodafone Policy Paper, The role of mobile phones in Medicine, 2009, 36(2):165–175. increasing accessibility and efficiency in healthcare. Vodafone Policy 23. Adherence to long term therapies: Evidence for action. Geneva, World Paper Series 4, 2006. Health Organization, 2003. http://www.who.int/chp/knowledge/ 25. Technology trends: how technology will shape future care delivery. San publications/adherence_report/en/index.html (last accessed 3 August Francisco, Health Tech Report, 2008. 2009). Global Forum Update on Research for Health Volume 6 13
