Snake Spider Guidelines Gl2007 006 3
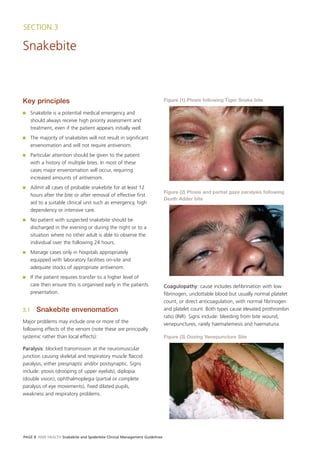
- 1. SECTION 3 Snakebite Key principles Figure (1) Ptosis following Tiger Snake bite ■ Snakebite is a potential medical emergency and should always receive high priority assessment and treatment, even if the patient appears initially well. ■ The majority of snakebites will not result in significant envenomation and will not require antivenom. ■ Particular attention should be given to the patient with a history of multiple bites. In most of these cases major envenomation will occur, requiring increased amounts of antivenom. ■ Admit all cases of probable snakebite for at least 12 Figure (2) Ptosis and partial gaze paralysis following hours after the bite or after removal of effective first Death Adder bite aid to a suitable clinical unit such as emergency, high dependency or intensive care. ■ No patient with suspected snakebite should be discharged in the evening or during the night or to a situation where no other adult is able to observe the individual over the following 24 hours. ■ Manage cases only in hospitals appropriately equipped with laboratory facilities on-site and adequate stocks of appropriate antivenom. ■ If the patient requires transfer to a higher level of care then ensure this is organised early in the patients Coagulopathy: cause includes defibrination with low presentation. fibrinogen, unclottable blood but usually normal platelet count, or direct anticoagulation, with normal fibrinogen 3.1 Snakebite envenomation and platelet count. Both types cause elevated prothrombin ratio (INR). Signs include: bleeding from bite wound, Major problems may include one or more of the venepunctures, rarely haematemesis and haematuria. following effects of the venom (note these are principally systemic rather than local effects): Figure (3) Oozing Venepuncture Site Paralysis: blocked transmission at the neuromuscular junction causing skeletal and respiratory muscle flaccid paralysis, either presynaptic and/or postsynaptic. Signs include: ptosis (drooping of upper eyelids), diplopia (double vision), ophthalmoplegia (partial or complete paralysis of eye movements), fixed dilated pupils, weakness and respiratory problems. PAGE 8 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
- 2. Myolysis: caused by generalised destruction of skeletal ■ Leave PIB in place until patient arrives at a place of muscle with high serum CK (creatine kinase) and definitive care (hospital with appropriate antivenom etc). myoglobinuria (red to brown urine testing positive for ■ As soon as possible after applying first aid as above, blood; can be confused with true haematuria), notify the relevant doctor or hospital, to organise occasionally severe hyperkalaemia. Signs include: muscle medical evacuation. movement pain or weakness, and red or brown urine. ■ If the snake was brought with the patient, place it in Figure (4) Myoglobinuria alcohol (if practical), and ensure it goes with the patient when evacuation occurs. Figure (5a) Pressure immobilisation bandaging Renal damage: primary or secondary (myolysis, Figure (5b) Pressure Immobilisation Bandaging coagulopathy) acute renal failure. Signs include: oliguria (decreased urine output) or anuria (no urine output). General symptoms: include anxiety, headache, nausea, vomiting, abdominal pain, collapse and convulsions. Local symptoms: vary from minimal to obvious bite marks, local pain, swelling, or bruising. A trivial-looking bite site does not mean a trivial bite. NB: Punctures or scratches may occur on the skin. 3.2 First aid Pressure Immobilisation Bandage (PIB) and Splint: Figure (5c) Pressure immobilisation bandaging ■ Maintain airway/breathing if impaired ■ Immediately apply a broad compressive bandage to the bite site at same pressure as for a sprain ■ Extend the bandage to cover the whole of the bitten limb including fingers/toes ■ Splint limb and immobilise ■ Keep the patient still and bring transport to the patient ■ Do not give alcohol, food, stimulants, or cut the wound, or use a tourniquet. ■ DO NOT WASH OR CLEAN THE WOUND NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines PAGE 9
- 3. 3.3 Hospital cllinical assessment 3.3.2 Clinical assessment Assess the patient for the following: 3.3.1 History ■ Evidence of a bite (if an adequate first aid bandage is 1. Establish whether the patient has a in place cut the first aid bandage away from over bite confirmed/witnessed snake bite (single or multiple) site and the area immediately surrounding the bite) OR were the circumstances such that a bite might ■ DO NOT WASH THE WOUND – SWAB FOR VENOM have occurred: DETECTION using the Snake Venom Detection 2. When the patient was bitten (elapsed time) Kit (SVDK) (refer to the SVDK section at page 11 in 3. Description of snake if possible (colour, length) these guidelines for technique of venom detection). Examine for evidence of multiple bites, or venom 4. Geographic location that the incident occurred movement (eg. swollen or tender draining lymph nodes) (snakes in area) ■ Neurotoxic paralysis (ptosis, ophthalmoplegia, diplopia, 5. Timing and type of first aid, and activity, following dysarthria, limb weakness, respiratory distress) the bite ■ Coagulopathy (bleeding gums, prolonged bleeding 6. Type and timing of symptoms, in particular: from venepuncture sites or other wounds, including a headache the bite site) b nausea ■ Muscle damage (muscle tenderness, pain on movement, c vomiting weakness, dark or red urine indicating myoglobinuria) d abdominal pain ■ Oliguria, anuria, or myoglobinuria e blurred or double vision ■ Period of unconsciousness or fitting f slurring of speech ■ General symptoms such as headache, vomiting, g muscle weakness abdominal pain, but beware of these in isolation (i.e. anxiety reaction only). If all other clinical and h respiratory distress laboratory indicators are normal, such general i bleeding from the bite site or elsewhere symptoms alone are not usually sufficient reason to j passing dark or red urine commence antivenom therapy k local pain or swelling at the bite site 3.3.3 Systemic envenomation l pain in lymph nodes draining the bite area (axilla, If it is evident that Antivenom Therapy will be required or groin), then refer to the Antivenom Administration section at m loss of consciousness and/or convulsions. page 22 in these guidelines). 7. Relevant past history – specifically ask about allergy Systemic envenomation is present if there is one or more or past exposure to antivenom, atopic (allergy) of the following: history, renal, cardiac, or respiratory disease and medications (eg. anticoagulants etc). ■ Neurotoxic Paralysis (e.g. ptosis, ophthalmoplegia, limb weakness, respiratory effects) 3.3.2 Presentation scenarios ■ Significant Coagulopathy (e.g. unclottable blood, INR>2, prolonged bleeding from wounds and ■ Possible or definite snakebite. venepunctures) ■ The patient presents unwell, diagnosis uncertain. ■ Significant Myolysis (myoglobinuria) There is a history of possible exposure to snakes (i.e. walking in long grass etc), and the patient has any of ■ Unconsciousness or convulsions the following: loss of consciousness, convulsions, Early non-specific symptoms such as headache, vomiting, headache, vomiting, weakness or paralysis (initially abdominal pain may indicate developing envenomation. ptosis, diplopia, slurred speech), dark or red urine, Beware of these as purely manifestations of anxiety bleeding, renal failure then consider snakebite. rather than envenomation. If these are the only evidence ■ The patient is unwell and may be envenomated. of envenomation then be cautious in deciding if antivenom is required. ■ The patient is well with no apparent envenomation. PAGE 10 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
- 4. 3.4 Snake Venom Detection Kit (SVDK) Figure (6) Snake Venom Detection Kits The SVDK is designed to detect very small amounts of snake venom, and indicate which type of venom is present, corresponding to one of the 5 monovalent antivenoms. It does not necessarily indicate if envenomation has occurred. Specifically: ■ Only use the SVDK to choose which antivenom is appropriate ■ Do not use it to determine if there is envenoming, or exclude snakebite ■ The best sample is a bite site swab (pre-moistened in 1. The best sample is a swab from the bite site. Take an supplied SVDK fluid): unused sample diluent bottle (currently yellow top) and use fingernail to lever off the dropper cap. – Cut away bandage over bite site and swab for venom detection 2. Moisten the swab stick provided, in the solution in the bottle. Rub the swab firmly over the bite site and – Collect at earliest opportunity after presentation adjacent skin. to hospital Figure (7) Swab bite site and adjacent skin – Where systemic envenoming is evident then urine may be used – NB: Blood testing is unreliable ■ The test may take up to 25 minutes and is best performed in a laboratory ■ A positive result in an envenomed patient indicates a definite snakebite and the type of antivenom to use (if required) ■ A positive SVDK is not the sole indication to give antivenom 3. Place the end of the swab back in the bottle ■ Administer antivenom if there is clinical and/or containing solution and twirl around for a few laboratory evidence of significant systemic moments to transfer venom into solution. Then envenoming indicated by the clinical signs and proceed to use the kit as indicated in the instructions. symptoms listed 4. A positive result is indicated by a colour change (to ■ NB: Positive venom detection from the bite site does blue) in one of the first five wells, plus the positive not imply systemic envenoming and is not in itself an control well (well 7), within 10 minutes in the last indication for antivenom stage of the test. Observe all tubes carefully throughout this last 10 minute period to identify the ■ A negative result does not exclude either a snakebite first well to change colour. If one tube changes or systemic envenoming colour, all will do so eventually, but only the first tube ■ Always confirm the SVDK result by comparing with to change is relevant. result from diagnostic algorithms as outlined in Figure (12) combined with knowledge of snakes in region Figure (8) Positive venom detection 3.4.1 Snake venom detection kit testing The SVDK comes in a kit including three separate test well strips, each in protective foil, but only one set of instructions, reagents and accessories. It must be kept refrigerated, though if in a lab at 22ºC, it can be left out of the fridge for the 20–25 minutes required to perform the test. NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines PAGE 11
- 5. 5. A positive result usually indicates that: 11. The SVDK should not be used to determine if a ■ venom was present on the skin snakebite is a likely diagnosis. The only purpose of the SVDK is to determine best choice of ■ the type of snake involved antivenom, should antivenom be indicated on ■ the appropriate monovalent antivenom to use should clinical or laboratory grounds. this be needed Figure (9) Snake/well correlation 6. A positive SVDK result does not indicate systemic envenomation and is not an indicator for antivenom therapy. Well 1 Tiger Snake Venom 7. A negative SVDK result does not exclude snakebite (see these Guidelines on each type of snake for Well 2 Brown Snake Venom further guidance on interpretation). 8. Be aware that false positives from bite site swabs, though rare, are possible. Well 3 Mulga Snake Venom 9. If the patient has evidence of systemic envenoming and the bite site is not available for testing (i.e. been washed, or not apparent), then URINE is worth Well 4 Death Adder Venom testing for venom. See kit instructions for dilutions, if necessary. Do not test urine unless the patient has evidence of systemic envenoming. Do not try and use Well 5 Taipan Venom the SVDK to test on urine as a method of proving or excluding snakebite. Urine can give false positives for venom, especially brown snake venom. A positive SVDK Well 6 Negative Control result for brown snake venom, in the absence of clinical or laboratory evidence of envenoming, such as coagulopathy, in nearly all cases should be Well 7 Positive Control considered a false positive and therefore of no diagnostic value. Well 8 Blank Well 10. Blood has proved an unreliable sample for venom testing with the SVDK, giving both false positives and false negatives. It is not recommended for use with the SVDK. Figure (10) Actual SVDK result in a case of Mulga Snake bite — CSL Snake venom detection kit Weak positive well 1 (cross-linkage effect, not relevant) Strong positive well 3 = mulga snake Weak positive well 5 (cross-linkage effect, not relevant) Negative control well (6) Positive control well (7) PAGE 12 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
- 6. Figure (11) Common patterns of SVDK venom detection results Well number: Diagnostic pattern: 1 2 3 4 5 6 7 8 Only well 7 positive: No snake venom detected. This result does not include snakebite. Wells 7 and 1 positive: If systemic effects include defibrination, paralysis ± myolysis, suggests Tiger Snake or Rough-scaled Snake bite. If systemic effects defibrination only, consider bite by Broad-headed, Pale-headed or Stephen’s Banded Snake. If systemic effects are confined to paralysis, without defibrination, consider possibility of Copperhead Snake. Wells 7 and 2 positive: Most likely a Brown Snake bite. If systemic envenoming develops, expect defibrination coagulopathy, ± renal damage. Paralysis is unlikely and myolysis should not occur. Wells 7 and 3 positive: Most likely a bite by a Mulga Snake (King Brown) or Collett’s Snake. If systemic envenoming, expect myolysis, extensive swelling of bitten limb, ± anticoagulant coagulopathy, ± renal damage, OR possibly a bite by a Red-bellied or Blue-bellied (Spotted) Black Snake. If systemic envenoming, expect only mild myolysis, no coagulopathy, paralysis or renal damage. Wells 7 and 4 positive: Death Adder bite. If systemic envenoming develops, expect post-synaptic paralysis, no coagulopathy, significant myolysis or renal damage. Wells 7 and 5 positive: Taipan or Inland Taipan bite; systemic envenoming very likely. Expect defibrination, coagulopathy, paralysis, ± myolysis, ± renal damage. Wells 7, 1 and 3 positive: This pattern is sometimes seen with bites by several species. With a Copperhead bite, if there is systemic envenoming, expect paralysis without coagulopathy. If a Red-bellied or Blue-bellied (Spotted) Black Snake bite, if there is systemic envenoming, expect only mild myolysis, no coagulopathy, paralysis or renal damage. If a Collett’s Snake bite, if there is systemic envenoming, expect myolysis, possibly anticoagulant coagulopathy, ± renal damage. NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines PAGE 13
- 7. Figure (12) Methods for determining type of snake if venom detection is not available or has failed Determining the most likely snake based on clinical findings Start here Local effects of bite Examine the bite site Minimal local effects, no significant Obvious redness, swelling, redness, swelling, bruising ± bruising Moderate to severe Minimal or no Marked swelling after Only mild swelling local pain local pain 3+ hours after 3+ hours • Brown Snake • Mulga Snake • Tiger Snake • ? Death Adder • Red-bellied Black Snake • Rough-scaled Snake • ? Taipan • Yellow-faced Whip Snake • ? Taipan Combine this information with the result of the systemic effects key (below) to give a best guided estimate for the type of snake most likely to have caused the bite. Accuracy can be improved by matching this with known snake fauna for the region where the bite occurred. Systemic effects of bite Is there a coagulopathy? Yes No Is there paralysis? Defibrination Anti-coagulation Yes No coagulopathy normal low fibrinogen fibrinogen Is there major Is there major raised FDP/XDP and FDP/XDP myolysis? myolysis? Is there paralysis Is there ± myolisis? paralysis? No Yes No Yes No No Yes • Brown Snake • Mulga Snake • Mulga Snake • Red-bellied • Tiger snake • ? Death • Broad-headed • Spotted • Spotted Black Black Snake • Rough-scaled Adder Snake or Black Snake Snake • Yellow-Faced snake • ? Copper- Stephen’s • Collett’s • Collett’s Snake Whip Snake • ? Taipan head Banded Snake Snake • Small-eyed Snake Please note: This chart cannot cover all possible situations and assumes an understanding of the symptoms and signs of local, general and specific envenoming by Australian snakes. If in doubt, seek advice from the Poisons Information Centre (131 126) and from your local Critical Care Referral Network. © 1998 Dr Julian White PAGE 14 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
- 8. 3.5 Laboratory evidence of 2. Defibrination coagulopathy + paralysis ± mild envenomation myolysis Bite site is variable and there may be an ooze of blood. Laboratory testing in cases of possible snakebite is crucial Likely snakes include: in diagnosis and is urgent. Any delay in delivering results may delay definitive and life saving treatment. Frequent ■ Taipan and Inland Taipan (Genus Oxyuranus). repeat testing is almost always required. This is to ensure 3. Defibrination coagulopathy + paralysis + that delayed envenoming or failure to respond to initial moderate to severe myolysis treatment is not missed. Bite site is usually painful with mild swelling, bruising, 3.5.1 Laboratory testing redness, and there may also be an ooze of blood. Likely snakes include: ■ Laboratory tests to monitor for envenoming should include coagulation studies (INR, aPTT, fibrinogen, ■ Tiger Snakes (Genus Notechis) d-dimer), FBC/CBP (including blood film examination ■ Rough-Scaled Snake (Genus Tropidechis) for schistocytes), EUC and CK. (Where direct fibrinogen testing is possible, down to very low levels 4. Moderate to marked myolysis + anticoagulant of fibrinogen, this is also a useful test). coagulopathy (fibrinogen normal, no raised FDP/XDP) ■ If initial tests are normal, repeat testing at least twice, at approximately 2–3 hour intervals, or more urgently No paralysis (beware major myolysis mimicking paralysis). if the patient develops clinical evidence suggestive of Bite site is usually painful, often with marked swelling envenoming. and sometimes bruising. Persistent blood ooze is not common. Likely snakes include: ■ Where laboratory testing is not rapidly accessible a whole blood clotting time (WBCT) may be performed ■ Mulga snake, Collett’s snake, Spotted black snake but should not delay arrangements for transfer of the (Genus Pseudechis). patient. (WBCT – put 10 ml venous blood into a glass 5. Moderate to marked myolysis test tube and measure time taken to clot – normal less than 10 mins). No paralysis (beware major myolysis mimicking paralysis) or coagulopathy. Bite site is usually painful, has marked ■ An INR>2 indicates a coagulopathy (unless the swelling and sometimes bruising. Persistent blood ooze patient is on Warfarin). not common. Likely snakes include: ■ Myoglobinuria or a significantly raised CK indicates ■ Mulga snake, Collett’s Snake, Spotted Black Snake myolysis. (Genus Pseudechis). ■ Abnormally raised creatinine or urea indicates renal ■ Eastern Small-Eyed Snake (Rhinoplocephalus damage. nigrescens). ■ Cut away the bandage over bite site and swab for venom detection (CSL Snake Venom Detection Kit). 6. Paralysis (postsynaptic: reverses with antivenom therapy) ± mild anticoagulant coagulopathy ■ The best sample for venom detection is a bite site swab. No myolysis and renal damage unlikely. Bite site is often 3.5.2 Clinical and laboratory profiles painful, but with little swelling, redness or bruising. following Australian snakebite Persistent blood ooze unlikely. Likely snakes include: 1. Defibrination coagulopathy ■ Death Adders (Genus Acanthophis). No paralysis or myolysis. The bite site usually has minimal 7. General symptoms of envenomation (some or all or no pain, no significant swelling, bruising or redness, of: headache, nausea, vomiting, diarrhoea, but there may be ooze of blood. Likely snakes include: abdominal pain, dizziness, collapse). ■ Brown Snakes (all species except Ringed Brown No paralysis or coagulopathy with no, or generally mild, Snake) (Genus Pseudonaja) myolysis. Bite site is usually painful with marked swelling ■ Broad-headed Snakes, including Stephen’s Banded and sometimes bruising. Persistent blood ooze not Snake and Pale-headed Snake (Genus Hoplocephalus) common. NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines PAGE 15
- 9. Likely snakes include: ■ This is an important indication of possible developing coagulopathy. However, a similar ■ Red-bellied Black Snake (Pseudechis porphyriacus) picture is present in a patient with venous and mild bites by Spotted Black snake and Collett’s thrombosis problems, so careful clinical judgement Snake (Genus Pseudechis). will be required by the treating doctor, to decide ■ Yellow-faced Whip Snake and other large Whip which is the more likely diagnostic explanation. Snakes (Genus Demansia). b. Anticoagulation-type coagulopathy (Mulga Snakes, Collett’s Snake). 3.6 Essential information for hospital ■ Characterised by mild to grossly prolonged PT and laboratory staff aPTT, but normal fibrinogen levels and no significant Details of venom actions and venom profiles for each elevation of d-dimer/FDP. major snake species are contained in these guidelines and c. Patients on Warfarin and similar anticoagulants should be referred to when interpreting laboratory results. ■ These patients may present a problem in interpreting results, if bitten by a snake. Warfarin should cause 3.6.1 Required laboratory testing prolongation of PT in particular, sometimes with 1. Coagulation Studies: PT/INR, aPTT, fibrinogen level, elevated d-dimer/FDP, but normal fibrinogen. If d-dimer/FDP, platelet count (Where direct fibrinogen snakebite defibrination coagulopathy is overlaid testing is possible, down to very low levels of on this background, in most cases, fibrinogen will fibrinogen, this is also a useful test). be depleted and d-dimer/FDP grossly elevated, with a. Defibrination-type coagulopathy (BrownSnakes, an INR of >4, usually >10 (actually infinity). This Tiger Snakes, Rough-scaled Snake, Taipans, Broad- should not cause confusion in interpretation, as headed Snake group). such a pattern is clearly not due to Warfarin, but a result of envenoming. ■ Characterised by grossly prolonged PT & aPTT, undetectable fibrinogen, grossly elevated d-dimer/ ■ This pattern may be complicated by the fact that FDP, platelets normal (sometimes slightly low). warfarin causes low levels of factors, which the toxins need to act on, leading to different ■ Some coagulation machines will have trouble pharmacodynamics. giving results in this situation. If the machine indicates gross prolongation of PT/aPTT, but ■ In cases with early or mild snakebite defibrination fibrinogen “very high”, this usually indicates coagulopathy, changes may be subtle. In this undetectable fibrinogen. setting, significant elevation of d-dimer/FDP may be the most important diagnostic clue that envenoming ■ If d-dimer/FDP is elevated, you can be sure is occurring. In cases of snakebite anticoagulation- fibrinogen will be very low, not very high. As soon type coagulopathy, interpretation may be more as such a picture is evident, immediately report difficult, as elevation of d-dimer/FDP is not a feature. this to the treating doctor. In this setting coagulation tests may not give clear ■ Do not delay while trying to get final results from cut evidence of envenoming. Fortunately, in these the machine. Similarly, if d-dimer/FDP is elevated, cases, clinical features and rising CK are likely to report this first, then go back and determine the assist in diagnosis of envenoming. actual level, which may take time. 2. Complete blood picture (Platelets, Hb, WCC, ■ Do not waste valuable time retesting and calling absolute lymphocyte count, including blood film for new specimens because the machine cannot examination for schistocytes). cope with the grossly abnormal results. Snakebite a. Acute systemic envenoming usually causes an coagulopathy is common and time is of the elevated WCC essence. So, look for the typical defibrination picture and report this as soon as it is clear that it b. There may be an associated absolute lymphopenia, is present. Be aware that in mild cases, in the which can be quite marked early stages, PT/INR and aPTT may be normal, c. Lymphopenia is always present in tiger snake bites fibrinogen level normal or only slightly decreased, with systemic envenoming, but is less consistent for but d-dimer/FDP will be elevated. other snake species PAGE 16 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
- 10. d. Thrombocytopenia is not a common acute feature of b. There is no defined picture of envenoming-induced envenoming and when present, is often associated liver damage in humans. However, LDH is a useful with renal damage test in patients with haemolysis, either in Brown e. In rare cases, especially with Brown Snake bite, a Snake bites that develop microangiopathic haemolytic thrombocytopenia like picture may develop, often anaemia or in Black Snake where direct toxin after the initial defibrination coagulopathy is mediated haemolysis may occur. responding to antivenom. In such cases there will be 3.2.1 Derived fibrinogen (important a falling Hb, falling platelet counts, rising creatinine considerations) and urea, and usually schistocytes on the blood film. Derived fibrinogen is merely a reflection of the PT and as 3. Muscle Function (CK) such adds nothing more than a pseudo PT and is not as a. A number of snakes can cause moderate to severe sensitive as a direct Fibrinogen (Clauss). This is poorly systemic muscle destruction (myolysis) including recognised with many laboratories not clearly Mulga Snakes, Collett’s Snake, Tiger Snakes, Rough- distinguishing derived vs direct (Clauss), while others scaled Snake, Taipans and Black Snakes). report both derived and Clauss. b. This may take several hours to become evident, Furthermore, there is a limit of quantification/reporting occasionally days. for Clauss fibrinogen, because this differs on machines c. Clinically the patient develops muscle pain, weakness and most importantly in the way they are reported or and myoglobinuria. At a lab level, CK can become understood by the laboratory staff. grossly elevated. Some analysers will only allow results such as <0.65, and d. Significant myolysis is associated with CK levels it is impossible to get anything lower. This is not very >1,000 IU/L and can exceed 100,000 IU/L (sometimes sensitive because by the time the Fibrinogen is above far higher than this). In such cases beware associated 0.65 the PT/aPPT have usually started to recover. hyperkalaemia that can cause lethal cardiac toxicity. In some laboratories the limit of quantification is <0.5, e. Measurement of serum or urine myoglobin levels does however they will often report 0.2 or 0.3 but say it is not add to the diagnosis, is expensive, and treating below the limit of quantification (not detection) so they doctors should be encouraged to use CK levels as the can’t guarantee the difference. indicator of myolysis rather than myoglobin levels. This is an important difference in those reports below 4. Renal function (creatinine and urea) the LOQ and the LOD, which may not be clear to some Snakebite can cause renal damage and occasionally renal laboratories. failure, often secondary to coagulopathy, myolysis, or hypotension. In mild cases, especially with brown The issues around low levels of Fibrinogen are complex, snakebite, there may be a slow rise in creatinine and not necessarily well understood and are often limited by urea over the first few days, without polyuric or anuric the analyser only reporting <LOQ. This is primarily due to renal failure, which will reverse and gradually improve the broad acceptance that a Fibrinogen <1.5 is low and over a week or so. However, rising creatinine and urea often associated with significant haematological should always be flagged, as it may indicate progression abnormality. However, treated snake bite patients have to major renal failure. very low Fibrinogens which are actually recovering, but take time to get >1.5. For these patients it is important 5. Electrolytes to know that the Fibrinogen is just detectable. Hyperkalaemia is the major risk, most often in It is also common to find a “near normal” PT/aPTT when association with myolysis and secondary renal failure. there is still a low Fibrinogen around 0.5 – 0.9. This is a However, hyponatraemia can also develop, most likely in problem for the analyser and may not be understood response to over vigorous IV fluid replacement. well by Haematologists who are not familiar with results demonstrating a slightly raised INR and a low Fibrinogen. 6. Liver function tests a. LFTs are not routine tests in snakebite cases. It is suspected, but not yet proven, that in snake bite the Temporary elevation of LFTs sometimes occurs but is PT is driven by factor V deficiency (and also factor VIII), rarely of clinical significance and not so much by fibrinogen – the former recovers more rapidly, which is manifested by a normalisation of NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines PAGE 17
- 11. the PT and a gradual recovery of fibrinogen. This is likely results assessed, venom detection performed and to be the main driver for the use of Fresh Frozen Plasma result obtained), stabilised (ABC, IV line in situ, IV (FFP) in these situations. fluid load) and if envenomed, treatment commenced (appropriate type and dose of IV antivenom given). Given the complexity of interpreting derived Fibrinogen and very low Fibrinogen levels in these patients, it is – In a significant number of patients, initial clinical strongly recommended that early expert advice be and laboratory examination will be normal, with obtained in the first instance through the Poisons no indication of systemic envenoming. Such Information Centre on phone 131126. patients do not require antivenom at this time and the pressure immobilisation bandage first aid should be removed. 3.7 Hospital clinical management – The patient should then be fully re-evaluated Venomous snakebite is a medical emergency, potentially within 2 hours (including repeat laboratory life threatening, and is not a simple matter of just giving testing) or earlier if symptoms develop. antivenom. Expert advice is available from the Poisons – Do not leave pressure immobilisation bandage in Information Centre on phone 131126 and through place for long periods of time, especially in an the local Critical Care Referral Network. asymptomatic patient. A considerable number of snakebites do not result in significant illness, and do not require antivenom, but all 3.8 Clinical management of definite probable snakebites should be admitted for observation or probable snakebite in a hospital for at least 12+ hrs or overnight, as some serious effects without antivenom available may be delayed. Where the patient presents with a definite or possible Following the immediate clinical management, the snakebite. definitive clinical management will be dependant upon whether or not the health facility has antivenom stocks 1. If not already applied, immediately apply correct first immediately available. aid, namely a broad compressive bandage bound first over the bite site, at the same pressure as for a sprain 3.7.1 Immediate clinical management (i.e. not so tight that it occludes the blood supply), then bind the bandage over as much of the bitten ■ Assess and maintain airway limb as possible, going over the top of clothing, and ■ 100% Oxygen keeping the limb as still as possible. ■ Respiratory support as indicated 2. Once the limb is bandaged then immobilise it using a ■ Establish intravenous access and administer splint and keep it in a neutral position (not elevated intravenous fluids (fluid load) or below the patient). ■ Commence serial clinical observations and serial 3. Do not wash the wound, but if a venom detection kit laboratory testing. If clinical (including antivenom is available then swab the wound prior to applying stocks) or laboratory facilities are inadequate, first aid, but do not delay first aid significantly just to maintain pressure immobilisation bandage and swab for venom, unless the patient appears well and arrange retrieval to an appropriate hospital greater than 20 minutes has elapsed since the bite. ■ Antivenom therapy is indicated in most cases if there 4. Keep the patient as still and quiet as possible. is any evidence of systemic envenoming detected by 5. Fast the patient, and be prepared for vomiting. clinical observation or on laboratory testing 6. Carefully watch for evidence of envenoming, and if ■ Consult early with the local Critical Care Referral Network, there is respiratory distress then provide respiratory Clinical Toxicologist and the Poisons Information support. Centre preferably before commencing antivenom 7. Monitor urine output and colour. ■ Removal of pressure immobilisation bandage: 8. If the snake was brought with the patient, place it in – The bandage should not be removed until the alcohol (if practical) and ensure it goes with the patient is fully assessed (clinical history, patient when evacuation occurs. examination, laboratory tests performed and PAGE 18 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
- 12. 9. As soon as possible after applying first aid as above If patient already has severe envenomation then apply and notify the relevant doctor or hospital to organise pressure bandage/ immobilisation first aid if not in situ medical evacuation. It will assist the retrieval team if (remove only when initial antivenom therapy is completed). you can give the following patient status report: ■ Name, sex, age of patient 3.9.3 Blood samples ■ Brief history of the suspected bite 1. Whole blood clotting time (in glass test tube) ■ Was a snake seen? 2. Coagulation studies (PT/INR, aPTT, Fibrinogen, XDP/d- dimerFDP) full blood profile (CBP/FBE including blood ■ What type of snake? film examination for schistocytes) (Where direct ■ Was it a multiple bite? fibrinogen testing is possible, down to very low levels ■ Are there any symptoms or signs of envenomation? of fibrinogen, this is also a useful test) (Namely: headache, nausea, vomiting, abdominal 3. Electrolytes, renal function, CK pain, collapse, convulsions, early paralysis such as 4. Avoid venepuncture in sites where bleeding may be drooping upper eyelids, double vision, slurred difficult to control (i.e. femoral, neck, subclavian) speech, limb weakness, evidence of bleeding problem such as persistent ooze from the bite 3.9.4 Anaphylaxis site, evidence of muscle damage such as dark or red urine, muscle pain). Anaphylaxis due to allergy to venom is occasionally seen: (i.e. in reptile keepers). Treat with IV Adrenaline infusion or ■ Patient’s past history, particularly past snakebites IM Adrenaline (initial dose 0.25–0.5 mg.). For suggested with antivenom therapy, allergic disease, renal or paediatric dosages and further information, refer to the heart disease, or use of anticoagulant drugs relevant section in these guidelines.) (e.g. warfarin) or anti-platelet drugs (e.g. aspirin or NSAIDS). 3.9.5 Ongoing care 1. Observe closely for evidence of developing paralysis 3.9 Clinical management of definite (ptosis and diplopia). or probable snakebite in a hospital with antivenom available 2. Monitor urine output – indwelling catheter as necessary. 3.9.1 Respiratory failure 3. Serial respiratory function (FVC, O2 saturation and/or Artificial ventilation – mouth to mask; bag/mask, expired CO2). bag/endotracheal tube as indicated. 4. Check and update Tetanus immunisation status (once coagulopathy has resolved). 3.9.2 Circulatory failure 5. Avoid unnecessary venepunctures. 1. If cardiac arrest – commence cardiopulmonary 6. Once the patient is stabilised the pressure. resuscitation. immobilisation bandage may be removed however, if 2. Insert an IV line (normal saline, give initial IV fluid load, the patient has a severe envenomation and requires 500 – 1000ml over 2hrs in adults, 20ml/kg for children, transfer to another hospital and/or if there will be a then run at maintenance, keep the patient fasted). delay in obtaining further supplies of antivenom, consider leaving the pressure immobilisation bandage 3. If possible insert long line in cubital fossa or similar, in situ. to allow frequent blood sampling and avoid the need for further venepunctures. 7. If left in situ, then regular limb circulation observations should be performed. 4. Avoid subclavian, femoral and jugular vessels, as uncontrollable haemorrhage may occur if there is a coagulopathy. 5. If profound hypotension – fluid and electrolyte resuscitation. 6. A degree of hypertension may be encountered which usually resolves. NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines PAGE 19
- 13. Figure (13) Snakebite management chart Patient presents with possible snakebite Patient is severely envenomed, i.e. has Patient is symptom-free, or has only mild one or more of: collapse/unconscious, or general symptoms, i.e. has one or more of: paralytic signs, coagulopathy, myolosis headache, nausea/vomiting, abdominal pain FIRST AID FIRST AID FIRST AID FIRST AID Patient has had correct No effective first aid Patient has had correct No effective first aid has been first aid applied has been applied first aid applied applied DO NOT APPLY i.e. PIB APPLY PIB first aid i.e. PIB now if >1hr post-bite Leave PIB in place until patient is stabilised, TREATMENT fully assessed, and antivenom given (if required) • Insert IV line, given IV fluid load. • Take blood for lab tests. * • Cut away first aid bandage (if present) over bite site and TREATMENT swab bite site for venom detection. ** • Attend to ‘ABC’ but be careful of causing bleeding. • Collect urine and check for haemoglobin/myoglobin • Insert IV line, given IV fluid load. (dip stick) and keep for for venom detection. • Take blood for lab tests* and swab bite site for venom • Secure supply of antivenom (use Polyvalent AV or a detection** collect urine and check for haemoglobin/myoglobin mixture of monovalent AVs if snake identity uncertain (dip stick) and keep bite site swab for venom detection • Monitor fluid balance, consider catheterising if in doubt • Commence IV antivenom (use Polyvalent or mixture of about urine output. monovalent AVs if snake identity is uncertain; do not delay giving AV by waiting for venom detection results) • Consider giving increassed starting doses of antivenom Develops or has significant Remains symptom-free or • Monitor fluid balance, catheterise if in doubt about symptoms or signs or minor general symptoms only urine output. abnormal blood tests, i.e. (i.e. headache, nausea etc) paralytic signs, coagulopathy, and blood tests are normal; myolysis, renal impairment do not give antivenom Repeat blood tests at 3 hrs and 6 hrs post AV TREATMENT: Give appropriate Remove first aid once IV line Coagulopathy is resolving Coagulopathy not resolving Antivenom IV, diluted, inserted, venom detection* (rise in fibrinogen/reduction (no rise in fibrinogen/ adrenaline ready (in case of and blood tests performed in whole blood grossly prolonged whole anaphylactoid reaction and reported as normal clotting time) blood clotting time Leave PIB first aid in place TREATMENT: TREATMENT: Continue to TREATMENT: Give more until patient is stabilised Check patient for signs of monitor closely; repeat antivenom IV, diluted, and antivenom given envenoming frequently and blood tests to ensure adrenaline ready (in case of repeat blood tests after continuing improvement anaphylacticoid reaction about 2 hrs, then 2–3 hrs later TREATMENT: Once TREATMENT: recovered, send home but Admit overnight. If remains Remains symptom-free or minor general follow up for serum sick- well, repeat blood tests symptoms only (i.e. headache, nausea etc) and ness. Consider prophylactic next morning and if blood tests are normal; do not give antivenom oral steroids for 1 week. normal, send home. Patient discharged home *Laboratory tests Coagulation If no lab quickly available: • Whole blood clotting time (QBCT) (5–10 ml venous FIRST AID FOR SNAKE BITE SVDK SNAKE VENOM DETECTION KIT blood in glass test tube. Measure time to clot; >10 mins PIB = Broad bandage over **Cut away first aid bandage over bite site only, to allow suggests coagulopathy but test staff member’s blood bite site, then rest of bitten limb, visual access and swab for venom detection. NOTE: bite as normal control. including toes/fingers, at same site swab is best sample. Only test urine if no bite site If lab available, request: pressure as for ankle sprain, available AND patient has systemic envenoming. DO NOT • Prothrombin time/ INR • aPTT then splint limb, keep immobile. use SVDK to determine if patient has snakebite. • FDP/XDP (d-dimer) • CBP/FBE (platelet count and blood film for schistocytes) Please note: This chart cannot cover all possible situations and assumes an understanding of the Other symptoms and signs of local, general and specific envenoming by Australian snakes (see Section • Creatinine and urea • Electrolytes (especially K+) 4: Snakebite, and preceding pages). If in doubt, seek advice from the Poisons Information • CK for myolysis Centre (131126) and from your local Critical Care Referral Network. © 1998 Dr Julian White • CBP/FBE (WCC for leukocytosis ± lymphopenia PAGE 20 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
- 14. 3.11 Antivenom therapy your area. In general terms, in eastern NSW, a mixture of CSL Tiger Snake Antivenom and CSL Brown Snake Anti- Antivenom is the definitive treatment of envenomation, venom will often be appropriate, providing a bite from a potentially life saving and is produced using refined Death Adder can be excluded on grounds of description horse serum therefore it is potentially allergenic and as of the snake. However, there are areas where such a mix such its use is not without risk. Therefore, antivenom will not be sufficient, such as far North-Eastern NSW should only be used if there is systemic envenoming. where there is a chance of Taipans being present. Overall, less than 1 in 4 patients require antivenom therapy. 3.11.1 Key antivenom therapy principles 3.12 Antivenom therapy dose ■ The treatment of choice for systemic envenoming is The minimum dose is one vial of the appropriate to use a monovalent (specific) antivenom in antivenom however for some antivenoms the initial dose preference to polyvalent antivenom if the identity of is higher. snake is known. Multiple bites or severe envenoming mandate higher ■ Use the SVDK in conjunction with the diagnostic doses; increase the dose by 1 to 3 vials, depending on the algorithms along with consideration of the type of type of antivenom, and be prepared to give more. Four snakes found in region to determine the most to 6 or more vials is not unusual in a severe snakebite. appropriate antivenom therapy. If there is a coagulopathy then the dose can be titrated ■ Consult with the NSW Poisons Information Centre against serial coagulation results (see relevant section in Ph: 131126 if unsure or if there is a conflict between these or guidelines for managing coagulopathy). the SVDK and diagnostic algorithm results. ■ Do not overlook polyvalent antivenom as backup if 3.12.1 Brown Snake insufficient monovalent antivenom available. The starting dose for severe Brown Snake envenomation ■ 1 vial of CSL Polyvalent Snake antivenom is is currently being investigated by a national multi-centre equivalent to 1 vial of relevant monovalent prospective trial. The initial dose may range from 2 to 5 antivenom. vials. ■ Dosage varies with the type of antivenom, type of snake and number of bites however, children In small remote centres, the current recommended initial require the same dose as adults. dose in a life-threatening situation is 2 vials. Organise medical retrieval as early as possible for the patient to be ■ Further doses of antivenom may be required in major immediately transferred to the closest Rural Referral cases. Hospital for ongoing management and additional doses as required. 3.11.2 Snake identified In Rural Referral and Tertiary Referral Hospitals sufficient Monovalent Antivenom is preferred to Polyvalent as it is antivenom stocks will be available to give additional doses less hazardous and has fewer side effects, and is less as required and replenish stocks at the small remote centres. expensive. Refer to the relevant section on specific snake management, in these guidelines, for the appropriate, safe As dosing recommendation may evolve with time, and effective administration of antivenom therapy. It must consultation with a clinical toxicologist via the New be noted that bites by some snakes may not need anti- South Wales Poisons Information Centre Phone venom even if there is mild to moderate envenoming. 131126 is recommended in all cases. 3.11.3 Snake not identified 3.12.2 Tiger Snake Where an SVDK is not available, or failed, or the patient Starting dose for a major bite is 4 vials of CSL Tiger requires antivenom before a SVDK result is possible, then Snake Antivenom. either Polyvalent Antivenom or an appropriate mixture of Monovalent Antivenoms should be used. Diagnostic For some smaller rural hospitals, the recommended stock algorithms (Figure 12, page 14) may assist in choice of level is only 2 vials, to be given in life-threatening antivenom. Refer to Appendix (1) to determine if there is situations, whilst supplementation of stocks from another an appropriate mix of two monovalent antivenoms for hospital, plus medical retrieval, are being arranged. NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines PAGE 21
- 15. 3.12.3 Taipan Snake 7. Record blood pressures on the other side to the fluid/adrenaline infusion, to avoid prolonged cuff Starting dose for a major bite is 3 vials of CSL Polyvalent inflations and thus extravasation of infusion fluids. or 3 vials of Taipan Antivenom. 3.13.2 Administration method 3.12.4 Mulga Snake 1. Antivenom for snakebite should always be given IV, Starting dose for a major bite is 1 vial of CSL Black Snake with all facilities ready to hand to treat Antivenom or 1 vial Polyvalent Antivenom. anaphylaxis in the rare event that it should occur. 3.12.5 Red-bellied Black Snake 2. Intravenous fluids running. 3. Dilute the antivenom about 1:10 (1:5 or less may be Starting dose for a major bite is 1 vial of CSL Tiger Snake needed if volume is a problem, i.e. polyvalent Antivenom (not Black Snake Antivenom). antivenom, paediatric patient), in IV fluid (e.g. normal saline, or Hartmans). 3.12.6 Death Adder 4. Start infusion very slowly carefully observing patient Starting dose for a major bite is 1 vial of CSL Polyvalent for reaction (look for flushing, rash, tachycardia, or 1 vial Death Adder Antivenom. hypotension, bronchospasm; in children warning As dosing recommendation may evolve with time, signs also include nasal, palatal, or ocular pruritis, consultation with a clinical toxicologist via the New coughing, sneezing, profuse sweating, faecal or South Wales Poisons Information Centre, phone urinary urgency or incontinence, abdominal pain, and 131126 is recommended in all cases. a sense of impending doom) and increase rate aiming to give whole dose over 15 to 20 minutes. 5. If the patient has had 25 mLs or more Antivenom then 3.13 Antivenom administration consider a 7-day course of prophylactic oral steroids. Prepare the patient and clinical environment for potential 6. Ensure snakebite patients are followed up adequately, anaphylaxis or anaphylactoid reaction to antivenom. particularly if given Antivenom, watching specifically for serum sickness. 3.13.1 Preparation prior to commencing antivenom 3.13.3 Management of an anaphylactic reaction 1. High flow oxygen. 1. Most reactions are related to the rate of antivenom 2. Dedicate one small bore (18–20g in adults) IV line to infusion. antivenom administration, and one large bore IV line 2. Some mild reactions resolve with temporary cessation (16–14g in adults) for emergency resuscitation of the antivenom infusion and recommencing (equivalent size suitable for children). infusion at a slower rate. 3. Prepare 1L Normal Saline (20 mL/kg in children) ready 3. Envenomed patients may be severely coagulopathic, to give under pressure. so caution must be observed when giving Adrenaline 4. Prepare adrenaline 1:1000 (1 mg in 1mL) drawn up to to avoid blood pressure surges, which might lead to a dose of 0.01 mg/kg (max. 0.3 mg, i.e. max 0.3 mL) intracerebral haemorrhage. and label “Adrenaline for IM injection only (dose in mg)”. 4. Initial management of severe reactions (sudden 5. Prepare an IV infusion of adrenaline 1 mg in 100mL hypotension, bronchospasm): or as per local protocol (controlled by infusion pump a. Suspend the antivenom infusion or syringe driver) ready to attach by a side arm to the b. Lie the patient flat (if not already), continue high resuscitation line. Anti-reflux valves must be attached flow/100% oxygen and support airway/ventilation above the side arm on any other infusions using this as required IV, to prevent adrenaline going back up into the other fluid bags. To prevent erroneous administration, do c. Rapid infusion of 1L Normal Saline (20 mL/kg in not attach the adrenaline infusion unless it is needed. children) over 2–3 minutes 6. Continuous monitoring of vital signs including ECG, d. Adrenaline IM into the lateral thigh, 0.01mg/kg to Pulse, BP and Sa02%. maximum of 0.3 mg (observe puncture site for PAGE 22 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
- 16. bleeding). Alternatively an IV Adrenaline infusion 2. Simultaneously take blood for later laboratory tests. may be used as per point 5b below 3. The most useful tests are: prothrombin ratio (INR), e. Liaise with toxicology service regarding ongoing aPTT, fibrinogen level, and fibrinogen degradation management products (XDP/d-dimer or FDP). 5. For reactions that do not respond to initial management: 4. In some laboratories a thrombin clotting time (TCT) a. If hypotensive, repeat Normal Saline bolus as may be useful to assess fibrinogen level. above (up to 50mL/kg may be required) 5. A complete blood picture (CBP/FBE) should be b. Commence IV infusion of adrenaline performed for platelet count. (0.5–1mL/kg/hour, of 1mg in 100mL) and titrate 6. In most cases, a single batch of tests will not be according to response; monitor BP every 3–5 sufficient, and serial studies will be needed. minutes (using the arm opposite to the infusion); beware that as the reaction resolves adrenaline Expected results in coagulopathy: requirements will fall, the blood pressure will rise 1. Whole blood clotting time will be greater than 15 and the infusion rate will need to be reduced minutes or there may be only a weak clot in less 6. Consider nebulised salbutamol for bronchospasm, severe cases (usually will not clot even after 1 hour) / nebulised adrenaline for upper airway obstruction, (normal = less than 10 minutes). and IV atropine for severe bradycardia. 2. INR (prothrombin time) grossly prolonged (>4, usually 7. Seek advice urgently from the local/regional ED infinity) / (normal = 1.0). Consultant and/or ICU Consultant. 3. aPTT grossly prolonged (>150 secs) / (normal = less than 40 secs). 3.14 Snakebite coagulopathy 4. Thrombin clotting time (TCT) grossly prolonged (>150 secs) (normal 15 secs). 3.14.1 Defibrination 5. NOTE: TCT may be the first parameter to show Some snakes may cause a significant coagulopathy as part improvement as a result of antivenom therapy, of envenoming (e.g. Brown Snakes, Tiger Snakes, dropping from >150 secs to less than 100 secs. If this Rough-scaled Snakes, Broad-headed Snakes, Stephen’s occurs it probably indicates that enough antivenom Banded Snakes, Taipans). This is due to potent has been given, despite the lack of improvement in procoagulants in the venom, which in vivo cause other parameters, therefore cease further antivenom consumption of fibrinogen and fibrinolysis i.e. therapy and repeat tests in 1 hour to confirm trend Defibrination Syndrome. of improvement. 6. Fibrinogen level very low (<0.1g/L) / (normal = 1.5 to This may occur rapidly following envenoming, within 30 4.0g/L). This is the key diagnostic finding in to 60 minutes, with the blood being unable to clot. defibrination coagulopathy. Platelets are usually unaffected. 7. Fibrinogen degradation products grossly elevated Snakebite coagulopathy can prove complex to manage, (XDP/d-dimer > 16) / (normal = <0.25). This is and it is preferable to treat the patient in a major another key diagnostic finding. hospital, with full coagulation laboratory facilities on site. 8. NOTE: Degradation products are in themselves anticoagulant, and at such high levels may interfere Tests for coagulopathy: with some clotting tests, giving falsely high levels of 1. If there is no laboratory in your hospital, perform a abnormality, particularly INR and aPTT on some whole blood clotting time (5 to 10 mL venous blood in automated coagulation machines. This may obscure a glass tube, e.g. test tube, and observe time to clot; the first signs of recovery. normal is less than 10 mins, if there is a coagulopathy there will be no clotting at 15 minutes or only a very Management principles: weak clot). However, performing a WBCT is not a 1. If initial studies are normal, remove PIB first aid and substitute for laboratory coagulation tests and should repeat studies after 2 hours, or sooner if the patient only be used as initial assessment while transfer to a appears envenomed. hospital with laboratory facilities is being organised. NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines PAGE 23
- 17. 2. If the second set of tests are also normal, repeat a hard to ascertain, and the whole blood clotting time third time, a further 3 hours later. might be prolonged in these patients, though a clot 3. If there is a significant coagulopathy (unclottable blood, should eventually form, unlike true defibrination or INR>2 + low fibrinogen), then this must be treated. coagulopathy, as discussed earlier. 4. Antivenom is the treatment of choice. Replacement Experience has shown that persistent ooze from the bite therapy with clotting factors (e.g. whole blood, FFP, site or elsewhere is not likely as a result of venom cryoprecipitate) should be avoided as it is liable to induced direct anticoagulation, again, different to make the coagulopathy worse if there is still active defibrination coagulopathy. Brown Snakes, Tiger Snakes, venom. Once active venom is all neutralised by Taipans and other species causing defibrination do not antivenom normal homeostasis rapidly rectifies the cause this direct anticoagulation, as discussed earlier. problem (sometimes within 3 hours), placing the Antivenom is very effective at rapidly reversing direct patient out of danger (i.e. INR <4), usually without anticoagulation coagulopathy. Usually one vial of need of any other treatment. antivenom will suffice. 5. Antivenom therapy can be titrated against the resolution of the coagulopathy, in particular, the 3.14.3 Snakebite myolysis fibrinogen level. After the initial dose of antivenom retest clotting studies at 3 and 6 hours after This occurs most commonly after bites by Tiger Snakes, completion of antivenom dose. If still showing a non- Rough-scaled Snakes and Mulga Snakes/King Browns, resolving coagulopathy at 6 hours (i.e. no significant but may also occur occasionally after Taipan bites, while rise in fibrinogen level), it is usually necessary to give bites by Red-bellied Black Snakes and Spotted/Blue- more antivenom and repeat tests as above, bellied Black Snakes may result in low level myolysis continuing this process until there is evidence of (CK 500–3,000IU). resolution, but if there is no resolution after an It is the result of widespread direct damage to striated adequate initial dose, then expert advice should be muscle cells, resulting in complete muscle cell breakdown sought to determine further dosing, rather than within 1–3 days, though damage probably commences giving ever increasing amounts of antivenom. within 1–3 hours of venom reaching the muscle. Full 6. NOTE: even if enough antivenom has been given, recovery is possible, but will take 4+ weeks. many coagulation parameters will remain abnormal for hours or days, especially fibrinogen degradation The key diagnostic indicators are myoglobinuria (easily products, which may remain elevated for 48 hours, mistaken for haematuria) and a dramatic rise in plasma CK. longer if there is renal failure. A rise in fibrinogen The latter may reach figures much greater than level from zero to detectable is the key indicator of 100,000IU. In addition, patients complain of generalised resolution of the defibrination coagulopathy, not a muscle pain, with tender muscles. return to normal fibrinogen levels, which may take The secondary effects of myolysis are renal failure and many hours. In some laboratories, the first evidence massive hyperkalaemia, which can be very difficult to of such a rise may be a fall in the aPTT or INR, rather control and has proven lethal. than a change in detectable fibrinogen titres. Once myolysis is established it is uncertain if antivenom 3.14.2 Anticoagulation will reverse damage, but in severe cases it may be worth trying further large doses of specific antivenom. This occurs after some severe bites by Mulga Snakes, Collett’s Snakes and possibly Spotted/Blue-bellied Black 3.14.4 Snakebite neurotoxic paralysis Snakes and is due to direct anticoagulants in the venom, which interfere with the extrinsic and, to a lesser extent, Presynaptic neurotoxic flaccid paralysis may occur after the intrinsic clotting pathways. bites by Tiger Snakes, Rough-scaled Snakes, Copperheads, Taipans, rarely Brown Snakes. This can result in a prolonged clotting time, elevated INR and aPTT, but fibrinogen levels and fibrinogen degradation It usually first manifests as ptosis, 1–3+ hours after the products are within the normal range. The INR, in bite, with potential progression to partial ophthalmoplegia, particular, may be grossly elevated, occasionally >12. complete ophthalmoplegia, fixed dilated pupils, dysarthria, However, without a full clotting laboratory, this may be dysphagia, peripheral weakness, culminating in PAGE 24 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
- 18. respiratory paralysis, though it may take 24+ hours to ■ Test for venom in urine using SVDK. reach this final stage. Once complete paralysis is ■ If in doubt discuss with a Clinical Toxicologist or established it may take days, weeks or longer to reverse Toxicologist at the NSW Poisons Information sufficiently for the patient to survive off a ventilator. Centre on 131126 or your local Critical Care Referral Antivenom will not reverse well established presynaptic Network. paralysis. Pure postsynaptic neurotoxic flaccid paralysis may occur 3.16 Management of the patient with after bites by Death Adders, resulting in similar, but often no evidence of envenomation more rapid progression of symptoms and signs. This form of paralysis is usually reversible if sufficient antivenom is 3.16.1 Relevant history given. Neostigmine may also reduce the degree of paralysis. ■ Was a snake seen to bite (?multiple bites) OR were the circumstances such that a bite might have 3.14.5 Follow-up of snakebite patients occurred? All patients with systemic envenoming should be ■ When did the patient get bitten (elapsed time)? followed up over 6 months, with particular concern for ■ Description of snake if possible (colour, length). serum sickness over the first 14 days. ■ Geographic location the incident occurred (snakes in Consider giving a 7-day course of oral steroids as prophylaxis the area). if more than 25 mLs of antivenom has been given. ■ Timing and type of first aid and activity after the bite. It is important to follow up all patients with initially trivial ■ Determine if there has been any evidence of or no apparent envenoming, especially if discharged less envenoming; specifically ask about headache, than 24 hours post-bite, to ensure late onset envenoming nausea, vomiting, abdominal pain, blurred or double is not missed. In particular, look for late onset neurotoxic vision, slurring of speech, muscle weakness, envenoming, myolysis (not if proven Brown Snake bite) respiratory distress, bleeding from the bite site or and renal damage. elsewhere, passing dark or red urine, local pain or swelling at the bite site, pain in lymph nodes draining the bite area (axilla or groin), loss of 3.15 Management of the severely ill consciousness, convulsions. patient where diagnosis of ■ Relevant past history; specifically allergy or past snakebite is obscure exposure to antivenom, atopic history, renal, cardiac, If the patient presents with unexplained onset of or respiratory disease. collapse, convulsions, bleeding, paralysis, rhabdomyolysis (e.g. muscle breakdown, myoglobinuria), or renal failure, 3.16.2 Examination in a setting where snakebite might have occurred (e.g. in Assess for: rural areas, or gardens, paddocks, long grass in urban areas), and particularly in children who may give no ■ Evidence of a bite (if there is an adequate first aid history of exposure to snakes, then include snakebite in bandage in place, cut it away from over the bite site, the differential diagnosis. keeping bandage away from area adjacent to skin (DO NOT WASH WOUND; SWAB FOR VENOM Useful tests to establish if there has been a snakebite DETECTION) looking for evidence of multiple bites, include: or venom movement (i.e. swollen or tender draining ■ Examine patient on exposed areas for bite marks or lymph nodes). scratches. ■ Neurotoxic paralysis (ptosis or drooping eyelids, ■ Whole blood clotting time or coagulation studies to diplopia or double vision, dysarthria or slurred establish if there is a coagulopathy. speech, limb weakness, respiratory distress). ■ Check for myolysis manifested by dark or red urine ■ Coagulopathy (bleeding from bite site or elsewhere). indicative of myoglobinuria (positive for “blood” and ■ Muscle damage (muscle tenderness, pain on so may be mistaken for haematuria), elevated CK movement, weakness, urine colour). (>1000). NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines PAGE 25
- 19. 3.16.3 Investigations ■ Whole blood clotting time in a glass tube OR ■ Complete blood picture (CBP/FBE/FBC) ■ Coagulation studies (PT/INR, aPTT, Fibrinogen, d- dimer/XDP/FDP) ■ Electrolytes (especially K++), renal function, CK (for myolysis) If envenomation is evident then refer to the relevant section in these guidelines and the Snakebite Management Chart (Figure 13: page 20). If envenomation is not evident then the patient will still need admission to hospital for observation overnight, preferably to a high intensity nursing area, ensuring that nursing staff are instructed to regularly check for signs of emerging envenomation, in particular early signs of paralysis (e.g. ptosis, diplopia, etc). (See Appendix 3.) NOTE: There is no point in leaving first aid in place if the patient is well and in hospital and the hospital is able to treat snakebite (i.e. has the appropriate antivenom available). The first aid bandage and splint merely delays venom absorption, it does not inactivate venom, and delay in removing first aid will delay onset of definitive treatment of snakebite. PAGE 26 NSW HEALTH Snakebite and Spiderbite Clinical Management Guidelines
