Elaina-Dan-Doug-AHECScholarPoster(FINAL)[1]
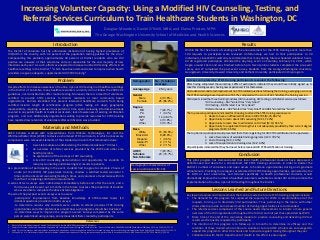
- 1. Increasing Volunteer Capacity: Using a Modified HIV Counseling, Testing, and Referral Services Curriculum to Train Healthcare Students in Washington, DC Douglas Meardon; Daniel O’Neill, MBA; and Elaina Preston, MPH The George Washington University School of Medicine and Health Sciences The District of Columbia has the unfortunate distinction of having highest prevalence of HIV/AIDS in the country, with 3.2 percent of the population testing positive for the virus.1 Compounding this problem, approximately 40 percent of District residents who are HIV positive are unaware of their serostatus and are responsible for the vast majority of new infections each year.1 As such, efforts are needed to increase routine HIV testing efforts in all healthcare settings in the District,2,3 which have been demonstrated to improve when health providers are given adequate, supplemental HIV CTRS training.4 Introduction Problem Results Materials and Methods AHEC Scholars worked with representatives from OraSure Technologies, Inc. and the Whitman-Walker Clinic (WWC) to devise a shortened CTRS curriculum, in which unnecessary components were removed. Elements of the standard curriculum that remained include: 1. A wet-lab module on administering the OraQuick Advance® HIV test. 2. An overview of referral services provided by the WWC and other area health providers. 3. An explanation of the six-steps of HIV counseling. 4. A live HIV counseling demonstration and opportunity for students to role-play counseling and delivering test results to patients. As a precondition of participating in the event, students had to agree to complete 2 hours of onsite (at the WWC) HIV paperwork training, shadow a certified tester/counselor 5 times and be observed counseling/testing 5 times, and volunteer at least twice within 6 months of completing certification requirements. A series of two surveys were administered immediately before and after the event, and a third survey will be sent out 6 months in the future to assess the proportion of students who were able to complete the above listed obligations. The aim of the pre/post event surveys was to assess: -participants’ improvement from baseline knowledge of CTRS-related topics (10 identical questions provided on both surveys) -to determine reasons why students were unable to attend previous CTRS training opportunities and other preferences around how such programs should be structured -to determine ways to improve the program overall. Surveys completed by the same person were linked using unique, anonymous identifiers created by participants. Despite efforts to increase awareness of routine, opt-out HIV testing in all healthcare settings in the District of Columbia, many healthcare workers currently do not follow the 2006 CDC guidelines, nor do institutions offer routine testing. Moreover, there is a dearth of volunteers certified to provide CTRS services to District residents at local community based organizations. Barriers identified that prevent interested healthcare students from being certified include: length of certification program (often lasting 2-3 days); geographic inaccessibility, requiring excessive transportation; time spent reviewing information already covered in any public health or medical curriculum; lack of awareness of existing certification program; and cost. Additionally organizations willing to provide resources for CTRS training have reported low retention of volunteers after certification was provided. Within the first five hours of sending out the announcement for the CTRS training event, more than 100 requests to participate were received. Unfortunately, we had to limit participation to 30 individuals, since WWC could only accommodate that many during future scheduled volunteer hours. All 30 registered participants attended the day-long event on Saturday, February 19, 2011, which began around 10am and was finished before 5pm. Twenty-nine students completed the pre-event survey and 27 completed the post-event survey. Students from the George Washington University, Georgetown University, Howard University, and Catholic University participated in this program. Demographic No. (% total) or Average Average Age 28.4 years Gender Male Female 4 (13.8%) 25 (86.2%) Degree MD PA MPH NP Other 7 (24.1%) 1 (3.4%) 14 (48.3% 4 (13.8%) 3 (10.3%) Race White Black/AA Hispanic Asian/PI Other 15 (53.6%) 8 (28.6%) 1 (3.6%) 2 (7.1%) 2 (7.1%) AHEC Scholars Non-Scholars 7 (23.3%) 23 (76.7%) Conclusion This pilot program has demonstrated that local health professional students have expressed a definite need and desire for a streamlined, HIV CTRS training curriculum, in order to bolster the District’s number of volunteers and open access to hands-on opportunities during one’s graduate school tenure. Providing more regular, accelerated HIV CTRS training opportunities, sponsored by the DC DOH or local universities, and tailored specifically to health professional students, would dramatically improve the number of qualified volunteers available to combat HIV and to promote the implementation of routine, opt-out HIV testing throughout the District. Lessons Learned and Future Directions Key lessons learned and improvements that can be made to a future CTRS training program include: 1. The demand for this program far surpassed the capacity for WWC to accommodate all of the requests, forcing us to drastically limit participation. Thus, partnering in the future with other clinics able to provide an increased number of training opportunities is recommended. 2. The referral services component of this course needs improvement to include a more general overview of the HIV organizations throughout the District and not just those provided by WWC. 3. More time at the end of the counseling module to practice counseling and delivering HIV test results was frequently requested by participants. 4. The intention of this program is to follow-up in 6 months to determine its efficacy and the retention of those trained who continue to volunteer. Future AHEC scholars are encouraged to expand this program to other DC schools and to provide regular training throughout the year. 5. Collaboration with the DC Department of Health in this effort is encouraged. References Demographic characteristics of session participants (N=29). Surveys completed by CTRS training participants revealed the following: After having completed the workshop, 100% of participants indicated they would have initially signed up to take this training session, having now experienced it for themselves. All students demonstrated improvement on CTRS-related questions following the training, averaging a score on the CTRS knowledge-based questions of 81.3%, compared with a score of 62.1% before the training session. Participants rated the three training modules (HIV counseling, HIV testing; and Referral services) as follows: • HIV counseling – 66.7% rated it as “Very Good.” • HIV testing – 88.9% rated it as “Very Good.” • Referral Services – 40.7% rated it as “Very Good” and 48.1% rated it as “Good.” The top reasons participants indicated for choosing to attend the CTRS training session were: 1. Desire to have an official certification in HIV CTRS (N=25; 86.2%) 2. Opportunity to learn about HIV counseling (N=21; 72.4%) 3. Opportunity to learn how to administer an HIV test (N=19; 65.5%) 4. Opportunity to supplement training that is not adequately provided by their current degree programs (N=19; 65.5%) The top barriers participants said prevented them from registering for HIV CTRS certification in the past were: 1. Lack of awareness of available training programs (n=23: 79.3%) 2. Cost of training (N=3; 10.3%) 3. Lack of transportation to training sites (N=2; 6.9%) All participants indicated that they had never before received HIV CTRS certification or training. 1. District of Columbia Department of Health. The District of Columbia HIV/AIDS Epidemiology 2009 Update. 2. Centers for Disease Control and Prevention. Expanded HIV testing and trends in diagnoses of HIV infection - District of Columbia, 2004-2008. MMWR Morb Mortal Wkly Rep. 2010 Jun 25;59(24):737-41. 3. Hsieh YH, et al. Emergency medicine resident attitudes and perceptions of HIV testing before and after a focused training program and testing implementation. Acad Emerg Med. 2009 Nov;16(11):1165-73. 4. Phillips, KA, et al. A multicenter study of internal medicine residents' perceptions of training, competence, and performance in outpatient HIV care. AIDS Patient Care STDS. 2010 Mar;24(3):159-64
Notas do Editor
- Figures: Demographic chart RESULTS: 100% said they would attend again Rating of 3 components(Q7) Top 3 reasons for attending Top barrier for registering in the past (Q8) Pre-post testing averages District of Columbia Department of Health, 2010.The District of Columbia HIV/AIDS Epidemiology 2009 Update.